Hematology PPT Flashcards Unit 1
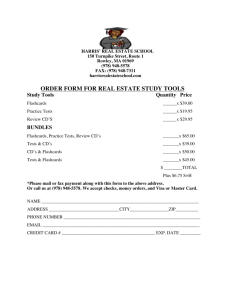
advertisement

Hematology PPT Flashcards Unit 1 The study of blood cells is called ___ A human body contains about ____ liters of blood Blood transports _____ from the lungs to the tissues. Blood also clears those tissues of _____ The liquid portion of blood is called ___ Describe the morphology of a normal RBC How many nuclei does a normal human RBC contain RBC’s are filled with a reddish protein called What is the diameter of a normal RBC The center of an RBC will appear _____ compared to the rest of the cell When did the first automated particle counters become available The _____ Principle of direct current electrical impedance is still used today in automated profiling instruments An RBC count below normal is An RBC count above normal is How is hemoglobin concentration derived. Hematocrit is a ratio of ___ over ___ A normal hematocrit approaches ___% Who first described worms in the blood back in the mid-1600s Who first gave an account of RBCs around the same time Who described platelets as petite plaques over 200 years ago In 1902 James Homer Wright developed the Wright stain. Why was this so important. RBC are fully described using these 6 parameters How many red blood cells are in 5 liters of blood? What cells have no nucleus? Why are red blood cells biconcave? What are the smallest cells in the body? What are red blood cells filled with that carry oxygen throughout the body? What is the average lifespan of an erythrocyte? Where in the body are old erythrocytes destroyed? Hematology 5 O2 CO2 Plasma Biconcave disc None Hemoglobin 6-8 microns Pale 1958 Coulter Anemia Polycythemia Sample is measured in a photometer at 540 nm after conversion of hemoglobin to cyanmethemoglobin with Drabkin’s reagent. Volume of RBC’s over volume of whole blood 50 Athanasius Kircher Antony van Leeuwenhoek Giulio Bizzozero It allowed detailed visual examination of blood using a microscope of things previously difficult or impossible to see. Shape, color, size, central pallor, contents and function 30 trillion Red blood cells To increase surface area Red blood cells Hemoglobin 120 days In the spleen and liver 1 Hematology PPT Flashcards Unit 1 What percentage of the body's cells are RBC's? How many RBC's are destroyed (as well as made) per second? How many RBC's are made each hour? Where are RBC's made? Hereditary spherocytosis is a red cell membrane disorder What is the condition in which too many red blood cells are produced and requires therapeutic phlebotomy? What is any condition of red blood cells in which the blood's capacity for carrying oxygen is diminished? What is the lack of oxygen to the tissues called? 25% 2.4 million What is the reduced blood flow to a tissue called? What are some of the causes of hypoxia? Ischemia Ischemia, malfunctioning hemoglobin, increasing altitude Reticulocytes in the blood Immature red blood cells True True Hemolysis Hereditary, acquired What is the characteristic sign of anemia? What are reticulocytes? Anemia can be caused by too few RBCs. Anemia can also be cause by iron deficiency. What is the rupture of RBCs? Hemolytic anemia can be ______, from autoimmune disorders or G6PD deficiency, or ________, from infections, or receiving the incorrect blood type in a transfusion. G6PD deficiency is hereditary and X-linked, so almost all are ______. G6PD is an ______ that is important for RBC metabolism. G6PD is the most common human enzyme deficiency. Pernicious anemia is also known as ___. Pernicious anemia is caused by a lack of vitamin B12 or intrinsic factor. After gastric bypass surgery, the stomach is no longer able to produce intrinsic factor, which is needed to absorb ______, which is needed to make _____ in RBCs. Without vitamin B12, the blood cells become fewer and larger than normal, or _______. Gastric bypass surgery patients must take vitamin B12 shots or sublingual supplements for the rest of their lives. What is Thalassemia? 8.6 billion In the red bone marrow True Polycythemia Anemia Hypoxia Male Enzyme True Megaloblastic anemia True Vitamin B12, hemoglobin Megaloblastic True A hereditary form of anemia where the 2 Hematology PPT Flashcards Unit 1 What is sickle cell disease? Which group of people that sickle erythrocytes present than other groups? What kind of infections that the sickle shape can prevent? What is hereditary spherocytosis? What is red blood cell (RBC) count? What does Hemoglobin (Hgb) measures? What does Hematocrit (Hct) measures? What is a quick screening test for anemia? How to perform the hematocrit test? What does hematocrit measures? What is the ratio of the hematocrit? What percentage is normal hematocrit What is a measurement of the average size of your RBCs? What is elevated when RBC are larger than normal? What is the term for larger than normal RBC? Name one condition where MCV is elevated What is the term for smaller than normal RBC? What is a calculation of the average amount of oxygen-carrying hemoglobin inside a red blood cell? What is a calculation of the average concentration of oxygen on the hemoglobin molecules inside a red cell? What is the term for decreased MCHC values? What is the term for increased MCHC values? What is a calculation of the variation in the size of RBCs have abnormal hemoglobin that deforms the cells A hereditary mutation resulting in one valine amino acid substituted for glutamic acid. people with African ancestry helps prevent malaria infections, but it also causes blood clots. The red blood cells shrink over time due to problems with the red blood cell membrane. is a count of the actual number of red blood cells per volume of blood. Both increases and decreases can point to abnormal conditions. the amount of oxygen-carrying protein in the blood. the percentage of red blood cells in a given volume of whole blood. the hematocrit test A drop of blood is drawn up a small glass capillary tube and the tube is centrifuged to pack the red blood cells at the bottom with the plasma on top. the percentage of blood volume that consists of erythrocytes. the ratio of packed red blood cells to total blood volume. about 45% (46% for men and 38% for women.) Mean corpuscular volume (MCV) Mean corpuscular volume (MCV) Macrocytic Anemia caused by B12 deficiency Microcytic Mean corpuscular hemoglobin (MCH) Mean corpuscular hemoglobin concentration (MCHC) Hypochromia Hyperchromia Red cell distribution width (RDW) 3 Hematology PPT Flashcards Unit 1 your RBCs? Having few RBC’s with various shapes is called? Having many RBC’s with various shapes is called? What is the practice of boosting the number of red blood cells in the bloodstream by giving an athlete an unnecessary blood transfusion in order to enhance athletic performance? Which athlete who won seven straight Tour de France titles confessed to using blood doping? What is the technique for determining which specific protein type is present on the RBC membranes? What are the proteins called when the cell membranes of the red blood cells carry certain types of proteins that another person’s body will think is a foreign body and reject it? What are the 2 types of blood antigens? If a person with type A blood gets a transfusion of type B blood, what would happen? Which blood type is considered the universal donor? Why is this possible? Which blood type is considered the universal acceptor? Why is this possible? What is the rarest blood type? What protein does the term “positive” or “negative” refer to in blood typing. What occurs when an Rh- mother has an Rh+ fetus in her womb (from an Rh+ father), and she has antibodies to the Rh factor? If a woman is Rh- and pregnant the doctor will administer an injection of what at 18 weeks and again within 72 hrs after giving birth? About how old is a fetus when it begins making Rh factor? True or False: During an Rh- woman's first pregnancy an Rh+ baby is not at risk of Hemalytic Disease of the Newborn. What protein is another RBC antigen and similar to Rh factor; in that, it can cause Hemolytic Disease of the Newborn. Anisocytosis Poikilocytosis Blood doping Lance Armstrong Blood typing Antigens (something that causes an allergic reaction) Type A and Type B the donated blood will clump in masses (coagulation), and the person will die. O negative. It is possible because there are no antigens on the blood cell. AB positive. This is possible because the plasma does not contain antibodies to A or B or Rh antigens. AB negative Rh Factor her antibodies will attack the red blood cells of the fetus because her body detects the Rh protein on the baby’s red blood cells and thinks they are foreign objects. This is called Hemolytic Disease of the Newborn (HDN). Rhogam 18 weeks True; during the first birth (or miscarriage), the placenta tears away and that’s when the baby’s blood cells get into the mother’s bloodstream. This begins the immune response. The Kell protein. People either have big K or little k proteins. Most people have little kk. If one parent has big K (either Kk or KK), the child can get Hemolytic 4 Hematology PPT Flashcards Unit 1 Define Pathogen Bacterium, virus, fungi, yeast, protozoa, and worms are examples of what type of pathogen? What is an example of a non-biological pathogen? How many bacteria can fit inside a white blood cell? Where do bacteria live in the body? How do bacteria cause harm? How many viruses can fit inside the nucleus of one white blood cell? How many viruses can fit inside the nucleus area of a bacterium? Where do viruses live in the body and why? What happens when a body cell has been invaded by a virus? What is an antigen? What are some examples of non-biological antigens? List the Leukocytes What percentage of all Leukocytes are Basophils? What is secreted by Basophil granules and why? What interferes with the function of Basophils? What is a Basophil that leaves the blood vessel and enters the tissues? What percentage of Leukocytes are Eosinophils? What roles do eosinophils play? Disease of the Newborn. Something that causes a disease. Biological Pathogens Toxic chemicals, asbestos are two examples. Bacteria are so small that hundreds of them can fit inside one WBC. They usually do not invade cells, they live between cells of the body, using nutrients in the area. By secreting toxins Thousands Hundreds They always try to invade body cells because they need host DNA or RNA to replicate The entire host cell must be killed by a white blood cell. An Antigen is anything that can cause an immune response, not necessarily a biological pathogen. Pollen, dust, grass, or anything that a person is allergic to. 1) Basophils -Mast Cells 2) Eosinophils 3) Neutrophils 4) Monocytes -Macrophages 5) Lymphocytes -B cells -T cells • 0.5 % • Histamines. It causes vasodilation so more WBCs can get to the infection site. • Antihistamines • Mast Cell • • 1-4% Ending allergic reactions and parasitic infections. They increase in numbers during these 5 Hematology PPT Flashcards Unit 1 Which is the most numerous White Blood Cell? Which White Blood Cell is the first to respond to infection? What roles do neutrophils play in response to infection? How many lobes does the nucleus of an Eosinophil have? How do Neutrophils contribute to immunity? When bacteria have capsules, they are harder to phagocytize. What action makes this process easier? What has some bacteria around them developed as a defense against phagocytosis. True or False: If a bacteria develops a capsule, neutrophils nor macrophages can not engulf that particular bateria. The process of facilitation of phagocytosis is called? What is the structure called when an invading bacteria has the antibody attached to its cell membrane? If a bacterium does not have a this structure, the neutrophil can destroy it without opsonization. When a capsule is present around a bacterium, what two that best work together are needed to kill the bacteria? This type of cell comprise about 5% of all WBC’s. This type of leucocyte use antibodies for opsonization. They phagocytize bacteria,old cells, and foreign bodies. When monocytes leave the bloodstream and enter the tissue, they are called? What cells are considered to be the most numerous of white blood cells? True or False: There are more macrophages in the tissue of the body than they are everywhere. Neutrophils live only a few days where as Monocytes/Macrophages live for how long? What cells phagocytize bacteria until they die? What type cell phagocytize and then take pieces of dead bacteria and present them to lymphocytes so a larger immune response can occur? What are the two type of phagocytes? What are Lymphocytes mostly needed to do? Neutrophils and macrophages main function is not to phagocytize viruses, but to what? • • conditions (Eosinophilia) Neutrophils Neutrophils 1) Phagocytize and destroy bacteria 2) Also destroy bacterial toxins in body fluids • a) 2-6 lobes b) Engulfing bacteria and foreign bodies (thorns, dirt) in a process called phagocytosis. They release the contents of lysosomes onto invader, dissolving it. c) Opsonization by antibodies d) Capsule e) 1 f) Opsinization g) Antigen-antibody complex h) Capsule i) Neutrophil and antibody j) Monocytes k) Monocytes l) Macrophages m) Neutrophils n) 1 o) Monocytes/Macrophages live for a few months. Neutrophils p) Macrophages Neutrophils and macrophages Kill off body cells infected by viruses. To phagocytize bacteria 6 Hematology PPT Flashcards Unit 1 What do macrophages have that make them recognize the surface of the pathogen’s cell membrane? When macrophages phagocytize bacteria, pop their lysosomes onto it and dissolve it, what do the macrophages do to their own cell membrane and for what reason? Macrophages present pieces of T cell lymphocytes and that T cell will present it to a what type of lymphocyte? The B lymphocyte feels the shape of the bacteria pieces, and the B lymphocyte can them launch an attack in the rest of that type of bacteria still alive in the body. What is this process called? What is a lymphocyte? There are two types of lymphocytes. What does one do and what does the other do? What are the two main classes of lymphocytes? Where do the B cells originate from? B cell that has not been presented to an invader is called a? After a B cell has been introduced to an invader, the B cell will mature into a what? A mature plasma cell fights infection by producing what? After the war of infection is over, the plasma cell will mature into a queen called a what? Where do the T cells originate from? Who do the T cells attack directly. What does a B cell mature into once they have been presented to? What is a function of a Plasma Cell? What is the function of the antibody from a Plasma cell? How do the antibodies of a Plasma Cell kill an attacking cell? How do the antibodies of a Plasma Cell kill an attacking cell? How do the antibodies of a Plasma Cell kill an attacking cell? Define the term Mononucleosis What is the cause of Mononucleosis? What is a characteristic of Mononucleosis? What is Lymphangitis? Surface receptors Macrophages place a piece of the bacteria’s cell membrane on it’s own cell wall until the macrophage finds a lymphocyte to present it to. B cell lymphocyte Antigen presentation Lymphocytes are cells which produce antibodies to kill any pathogens which invade the body. One makes antibodies and the other engages in direct combat with viruses. B cells and T cells Bone marrow Virgen B cell Plasma cell Antibodies Memory cell Thymus gland They attack foreign cells including organ transplants. Plasma Cell Secrete Antibodies Kill the attacking cell They attach to bacteria and pop the cell membrane They attach to encapsulated bacteria to help neutrophils and macrophages to phagocytize them They agglutinate (clump all over the bacteria, binding their receptor site so they cannot cause harm) A disorder of B-cell lymphocytes The Epstein Barr Virus Inflammation of lymph vessels(lymphangitis) Lymph vessel inflammation; usually from infection 7 Hematology PPT Flashcards Unit 1 What is a visual characteristic of Mononucleosis? What is the function of a T-cell? How does a T-cell directly destroy bacteria? How does a T-cell directly destroy a foreign cell? Host body cells that have become infected with viruses may be killed by what type of cell? What are characteristics of a T-cell regarding the killing of an invading cell? What is the relationship of a T-cell and antibodies? Which type of patient is at risk due to the function of T-cells? What type of cell attacks the organs of an organ transplant patient? What types of drugs are designed to inhibit the action of T-cells? What cell is attacked by the HIV (AIDS) virus? Where do T-cells originate from? What does the Thymus Gland secrete? What happens when a T-cell becomes immunocompetent? What are the three types of T-cells? What is the function of a Cytotoxic (killer) T-cell? What are the functions of a Helper T-cell? What happens when a T-cell presents a macrophage’s antigen to a B-cell? What are the functions of a Suppressor T-cell? What type of B-cell remembers how to destroy a pathogen that has once invaded the body? What is the function of Memory B-cells? Infected lymphocytes have a scalloped edge where they touch RBC’s Coordinate the immune response by recruiting other white blood cells. Popping their cell membrane Popping their cell membrane T-cell They do not need to phagocytize the invading cell, they just kill the cell and the macrophage dissolves the debris. T-cells do not need the assistance of antibodies in order to destroy an invading cell. Organ transplant patients T-cell Immunosuppressive drugs T-cell Thymus Gland Certain hormones which can cause Tcells to become immunocompetent Makes the cells mature and start to work Cytotoxic (killer), Helper, and Suppressor T-cells Go out and directly kill bacteria or infected host cells Release chemicals called “cytokines” to call more white blood cells of all types to join the war. Present the macrophage’s antigen to a B-cell. Produce antibodies against that particular bacteria Stop the immune process when it is over Tell plasma cells to “remember” how to destroy that specific pathogen. Memory B-cells React to remembered pathogens faster the next time it invades. 8 Hematology PPT Flashcards Unit 1 Why can Memory B-cells react to remembered pathogens faster? True or False? A pathogen can get past the body’s physical and chemical barriers and the inflammation response. What are pathogens engulfed by? What is another word for macrophage? What does the macrophage release onto a bacterium to dissolve it? True or False? There are still some pieces of the bacterium’s cell membrane left. What are surface proteins of macrophages also known as? Where does the macrophage force the antigens of the bacterium? True or False: B-cells touch these surface antigens to make a copy of their shape. Which cell is presented the surface antigen? B-cells create ________ against pathogens. True or False? Helper T-cells multiply and have two main roles Helper T-cells activate which type of cells? What does the Helper T-cell “tell” the B-cells to do? What do the B-cells turn into? Plasma cells multiply and produce _________ to ________ a specific pathogen What is the second role of the Helper T-cells? What do Killer T-cells secrete? True or False? Killer T-cells can destroy the pathogen itself (bacteria) Why would a Killer T-cell destroy an entire body cell? When an immune response is over, what kind of cell stops the process? What do Supressor T-cells “tell” some B-cells to do? B-cells (plasma cells) now become __________. What is leukemia? And what kind of cell does it involve? Memory B-cells already have the proper antibodies stored up for that pathogen. True Macrophages Neutrophil The contents of its lysosomes True Antigens To it’s own cell surface. False. Correct cell: Helper T-cells B-cells Antibodies True B-cells and Killer T-cells Helper T-cells tell B-cells how to neutralize the pathogen by presenting the pieces of the bacterium cell membrane. Plasma cells Antibodies; neutralize To activate the Killer T-cells. Cytokines True It is infected with a virus Suppressor T-cells Suppressor T-cells “tell” some B-cells (plasma cells) to “remember” how to destroy that specific pathogen Memory B-cells Cancer of the blood involving the white blood cells 9 Hematology PPT Flashcards Unit 1 What happens when one stem cell does not function properly? What is a result from a decrease of WBC? Where are the immature white cells sent to? Define Leukemia True or False? Even though WBC count is high, they are all immature forms Leukemia is a form of cancer classified as a disorder of ________ where too few mature ______ are made True or False? Lymphoblastic is defined as too many mature lymphocytes Too many immature neutrophils is defined as? What do people with severe leukemia need transplated? Before a bone marrow transplant, what has to happen with the recipients WBCs? The donor usually has a small cylinder of bone removed from their _____ How is the bone marrow given to the recipient? True or False? The new WBC’s may kill the patient or it may save their life Define WBC count True or False? An increase or decrease is WBC’s can be significant Define White blood cell differential How many different types of WBC are there? Name the different types of WBC’s Neutrophils are also known as Excess neutrophils is defined as Too few neutrophils is defined as Define thrombocytophilia Define thrombocytopenia How long do Lymphocytes live How long do Erythrocytes live How long do Platelets live It will make huge amounts of clones of itself which do not function the right way, resulting in not enough normal WBC being made The body cannot fight infection The bloodstream Leukemia can be defined as too few mature WBC True Leukocytes; WBCs False. Lymphoblastic is defined as too many immature lymphocytes Myeloblastic A bone marrow transplant The WBCs of the recipient have to be killed off with a medicine since they are mostly malfunctioning. Hip Via i.v True A count of the actual number of white blood cells per volume of blood. True It identifies the types of white blood cells present Five Neutrophils, lymphocytes, monocytes, eosinophils, and basophils. Segs, PMNs, granulocytes, grans Neutrophilia Neutropenia Excess platelets Too few platelets can live a lifetime 4 months about 2 months 10 Hematology PPT Flashcards Unit 1 How long do Monocytes live How long do Neutrophils live Antibodies are also known as what? What are antibodies made by? What are typically basic structural unit? What shape does the antibody form? What are the tips of the “Y” ? What does the stem of the “Y” do? What is the hypervariable region? What is the advantage of the hypervariable region? What is the function of IgD? What is the function of IgE? What is the function of IgG? What is the function of IgA? What is the function of IgM? Why are people sick more often as children than in their 20’s and 30’s? What is Myasthenia gravis (MG)? What are symptoms of MG? What are platelets made from? What happens when a platelet encounters a broken blood vessel? Platelets are responsible for what? What is a platelet? What is the primary function of a platelet? Where are platelets located? 30 days about a week immunoglobulins, abbreviated Ig are proteins made by plasma cells. each with two large heavy chains and two small light chains to form a unit shaped like the letter “Y” have receptors that are specific for a particular antigen can be grasped by a phagocyte. Small region at the tip of an antigen allowing millions of antibodies with slightly different tip structures, or antigen binding sites, to exist allows the immune system to recognize an equally wide diversity of antigens initiation of immune response stimulates allergic reactions, good for worm infections highest concentration in blood, highest amounts in most secondary responses. Indicates infection was in the past. It can also cross the placenta. secretory Ig, found in secretions, highest concentration in body produced first, best at C’ activation. Indicates infection is current we build up many varieties of memory lymphocytes during childhood, providing immunity from more and more antigens during adulthood autoimmune disease where antibodies destroy or block receptors for acetylcholine, a neurotransmitter. Causes flaccid muscle paralysis Pieces break off of a megakaryocte and are known as platelets it uses clotting factors (made in the liver and circulating in the blood) to form a web to clots blood. clot (thrombus) formation Is the cell fragment that is broken off from megakaryocytes. Function in clotting of blood In the plasma called Clotting factor in order for then to become activated form 11 Hematology PPT Flashcards Unit 1 What Term means lack of platelets? Primary vitamin that is needed for blood clotting factor? Where is vitamin K found? What is a Therapeutic use for Aspirin What is hemophilia? What is a thrombus? What is an Embolism? What is platelet count? What can thrombocytophilia and thrombocytopenia indicate? What is the Mean Platelet Volume and how does it relate to the age of platelets? What are the uses of PT and PTT tests and which are the coagulation factors they evaluate? a clot. They are found in Fibrin; it is made from Fibrinogen. Thrombocytopenia; it is abnormal lowing concentration of platelets. Vitamin K Found in green, leafy vegetables. Can help blood clots by blocking the action of platelets. It A hereditary disease of males, where they are unable to clot properly because they are missing some clotting factors. When they get even a slight bump or bruise they have to have an intravenous infusion of clotting factors or they will bleed to death. A clot in a vessel A thrombus that broke away and travels in the blood stream. It usually lodges in a smaller blood vessel and blocks circulation distal to that point. The platelet count is the number of platelets in a given volume of blood. Both increases (thrombocytophilia) and decreases (thrombocytopenia) can point to abnormal conditions of excess bleeding or clotting. Mean platelet volume (MPV) is a machine-calculated measurement of the average size of your platelets. New platelets are larger, and an increased MPV occurs when increased numbers of platelets are being produced. The PTT test is used to investigate unexplained bleeding or clotting. It may be ordered along with a PT (Prothrombin Time) test to evaluate hemostasis (the process of clot formation). The PTT evaluates the coagulation factors XII, XI, X, IX, VIII, V, II (prothrombin), and I (fibrinogen). A PT test evaluates the coagulation factors VII, X, V, II, and I (fibrinogen). By evaluating the results of the two tests together, a doctor can gain clues as to 12 Hematology PPT Flashcards Unit 1 How Heparin is used as anticoagulant drug therapy? What primary diseases are monitored by CBC and what are the parts of a Complete Blood Count? what bleeding or clotting disorder may be present. These tests are used to monitor heparin anticoagulant therapy. Heparin is a drug that is given intravenously (IV) or by injection to prevent and to treat blood clots. IV’s are also flushed with heparin to prevent clot formation. When it is administered for therapeutic purposes, it must be closely monitored. If too much is given, the treated person may bleed excessively; with too little, the treated person may continue to clot. The complete blood count or CBC test is used as a broad screening test to check for such disorders as anemia, infection, and many other diseases. It is actually a panel of tests that examines different parts of the blood and includes the following: White blood cell (WBC) count White blood cell differential Red blood cell (RBC) count Hemoglobin Hematocrit Mean corpuscular volume (MCV) Mean corpuscular hemoglobin (MCH) Mean corpuscular hemoglobin concentration (MCHC) Red cell distribution width (RDW) platelet count PT, PTT (separate test from CBC) List the three different types of granulocytes in the blood 13 Hematology PPT Flashcards Unit 1 List the two agranulocytes in the blood What is septicemia? What entry points bacteria can use in order to gain access to the blood? What consequences the presence of bacteria have in the blood? What is the treatment of septicemia? What are the stem cells? What are the advantages of stem cells and why would research use embryos as stem cell sources rather than the placenta? Septicemia (aka bacteremia or toxemia) is the condition when bacteria invade the body and circulate in the blood. Bacteria can enter the bloodstream as a severe complication of infections (like pneumonia or meningitis), during surgery (especially when involving mucous membranes such as the gastrointestinal tract), or due to catheters and other foreign bodies entering the arteries or veins (including intravenous drug abuse). Bacteremia can have several consequences. The immune response to the bacteria can cause sepsis and septic shock, which has a relatively high mortality rate (kills 1 person in 5). Bacteria can also use the blood to spread to other parts of the body (which is called hematogenous spread), causing infections away from the original site of infection. Examples include endocarditis or osteomyelitis. Treatment is with antibiotics, and prevention with antibiotic prophylaxis can be given in situations where problems are to be expected. STEM CELL: A cell that has not matured and differentiated yet. An embryo has lots of stem cells which have not decided to become a nerve cell, muscle cell, liver cell, etc. Stem cells become the type of cell the body needs. The placenta of a newborn infant has many of these stem cells, too, but not as many as an embryo. That’s why people 14 Hematology PPT Flashcards Unit 1 What is the first step for a stem cell? What is hematopoiesis? How many new blood cells are formed each day? Where are plasma proteins made? Where are blood cells made? Where is red bone marrow located? What are characteristics of yellow bone marrow? What is released into the bloodstream once completely mature? Where are blood cells destroyed once they are old? Where do T cells mature? What cells originate from blood stem cells? What happens when a RBC loses its nucleus? What are reticulocytes? What is the relationship between lymphoblasts and lymphocytes What are myeloblasts? What is Leukemia? What is an inflammation reaction? What are the four signs of inflammation? What causes redness in the stages of inflammation? want to research stem cells on embryos; there are more stem cells there. To differentiate in order to decide which cell it belongs to. blood cell formation 100 billion In the liver In the red bone marrow/spongy bone Epiphyses of long bones, girdles (clavicle, scapula pelvic bones), axial skeleton (sternum and vertebral bones) Contains many fats cells, located in long bones of adults, has nothing to do with forming blood cells. blood cells in the spleen and the liver the thymus gland erythroblasts: red blood cells lymphoblasts: lymphocytes myeloblasts: all other white blood cells it gains room for more hemoglobin cells with some bits of nucleus for about two days Lymphoblast give rise to lymphocytes These are the stem cells that mature into the other leukocytes. Leukemia is cancer of the stem cells When you get stuck by a thorn or have an infected cut, the body goes through a series of events called an inflammatory reaction. – Redness (erythema or rubor) – Heat (calor) – Swelling (edema or tumor) Pain (dolor) a. Redness is caused from the blood vessels dilating to allow more blood flow to the area. Within the blood are platelets to clot the blood, proteins to 15 Hematology PPT Flashcards Unit 1 repair the damage, and macrophages, which are white blood cells that eat up the foreign body, bacteria, or the dead cells. What causes heat in the stages of inflammation? b. Heat is caused because of the extra amount of warm blood flow to the area. What causes swelling in the stages of c. Swelling is caused from inflammation? the plasma that leaks out of the swollen blood vessels. What causes pain in the stages of inflammation? d. Pain is caused from the pressure of the extra fluid pressing on nerves in the area. What are the two types of immune response? The immune response is divided into two parts: Innate Immunity (WBC) and Adaptive Immunity e. (Antibodies) What are the two types of Adaptive Immunity? Active immunity and Passive immunity What is active immunity? Active means the person’s own body makes the antibodies. Naturally Acquired – The body is naturally exposed to an infectious agent and launches an immune reaction Artificially Acquired The person is injected with a weakened (attenuated) or killed organism, as found in a vaccination What is naturally acquired active immunity? It is when the body is exposed to an infectious agent and the body has to work to produce antibodies which specifically attack that infectious agent. In naturally acquired active immunity, which cells The white blood cells secrete these secrete these antibodies, how long can they live, antibodies which will continue to and how do they attack? circulate sometimes for years, ready to attack that type of bacteria and cause them to pop like a balloon before the body can become sick. Can you get the same cold virus twice? No, you will become immune to it. Your next cold is from a different virus. Which diseases may kill you at first exposure? Polio, diphtheria, tetanus, and influenza. 16 Hematology PPT Flashcards Unit 1 What is a vaccine? What is the point of vaccination? What is an example of Artificially Acquired Active Immunity? What does passive in Passive Immunity mean? What is an example of naturally acquired immunity? What are the two types of passive immunity? What are two examples of artificially acquired immunity? Are active or passive immunity for life or short life? What are allergies? What are the two types of allergic responses? What is an immediate allergic response? What will stop an allergic reaction for peanuts or seafood? What is a delayed allergic response? What is an example of a delayed allergic response? What are the two types of chemical mediators of allergies? What are the two preformed chemical mediators of allergies? What are the newly formed chemical mediators of It is an altered or attenuated form of the virus that the body recognizes as foreign, but they can’t cause disease. If the person is exposed to the real organism later, the antibodies are already there to kill it off without the body getting sick. An example is when a child is vaccinated against measles as a baby, so when he gets to school and is exposed to the disease, he doesn’t get sick. PASSIVE means the person’s body does not have to make the antibodies. An example is the passing of antibodies from mother to infant in breast milk. Naturally acquired or artificially acquired The first example is when a person receives an infusion of antibodies from someone else. The second is an example of an ebola survivor that donates his blood to another infected person. Active immunity is long-lived, and may last for years or even a life time. Passive immunity is short lived, and may last only for a few months. It is a hypersensitivity to substances such as pollen or animal hair that would not ordinarily cause a reaction. Immediate and delayed. A reaction that occurs within seconds of contact with the thing causing the allergy. A shot of epinephrine will stop the reaction. When the body’s first exposure to the substance will not cause a reaction, but all exposures afterward will trigger the response. Not itching the first time you touch poison ivy. Pre-formed and newly formed Histamine and proteases. Leukotrienes, platelet activating factor, 17 Hematology PPT Flashcards Unit 1 allergies? Bodily reactions to histamine? Bodily reactions to proteases? Bodily reactions to Leukotrienes? Bodily reactions to platelet activating factor? Bodily reactions to prostaglanin D2? Bodily reactions to cytokines? Where to symptoms of allergic reactions manifest themselves? What is a wheal-and-flare reaction? What are some examples of symptoms of an allergic reaction? What is localized anaphylaxis? What is the definition of pruritis? What is the definition of urticarial? What is allergic rhinitis? What is atopic dermatitis? What are the types of stimulants of an allergic asthma attack? What are the symptoms of an allergic asthma attack? What percent of the U.S. population is hypersensitive to allergens, and classified as asthmatic? What is an autoimmune disease? What is Hematology? What is done in a Hematology Laboratory? What is one of the most common types of tests prostaglanin D2, cytokines, Elevated vascular permeability; smooth muscle contraction Mucous secretion, generation of complement split products Elevated vascular permeability; contraction of pulmonary smooth muscles Platelet aggregation; contraction of pulmonary smooth muscles Vasodilation; contraction of smooth muscles Chemotactic and inflammatory They are dependent upon site of allergen exposure Pruritis (itching), erythema on the skin bronchoconstriction mucous secretion vasodilation (shock) A reaction limited to the site of allergen exposure Itching Hives Hay fever Eczema Airborne, blood borne, and degranulation of mast cells due to IgE cross-linking in the lower respiratory tract. airway edema mucous secretion inflammation 5% A hereditary problem where the body thinks its own tissues are foreign bodies, and it constantly tries to kill off its own tissues. Study of the diseases of blood The fundamental concepts of biology and chemistry are applied to the medical diagnosis and treatment of various disorders. CBC 18 Hematology PPT Flashcards Unit 1 performed in Hematology Laboratory? What is a CBC? What are two common instruments used in molecular diagnostics? What types of people are employed in a Hematology Laboratory? Assays and examinations performed in the Laboratory are used for what purpose? What are some of the safety procedures in a Hematology Laboratory? What are the duties of the safety officer? What are OSHA Standards? What is a Chemical Hygiene plan? What is a MSDS? How were HAZCOM Standards procedures described? Complete Blood Count, for example, Red Blood Cells diagnosis Anemia, White Blood Cells diagnosis Leukemia’s and Platelet diagnosis coagulation. Flow cell cytometry and Digital Imaging MLS, MLT, Lab assistants, and phlebotomists play a major role in patient care. Establish a diagnosis, rule out a diagnosis, detect an Unsuspected disorder, monitor the effects of therapy, Detect minimal residual disease following therapy. Exercising good technique, staying alert, a formal safety program, specifically mandated plans for example, chemical hygiene, bloodborne pathogens, identification of various hazards for instance, chemical and biological. Duties affecting staff including compliance with existing regulation affecting laboratory and staff for instance labeling of chemicals and providing supplies for proper handling and disposal of biohazardous materials Occupational Safety Health Administration Acts is to ensure safe and healthful working conditions for workers suitable protective equipment, exposure control procedure, and implementation of training and education programs Ensures Laboratory workers are fully aware of hazards associated with chemicals in their workplaces. Material Safety Data Sheet describes hazard, safety handling, storage and disposal of hazardous chemicals. • Revised criteria for the classification of chemical hazards • Revised labeling provisions that 19 Hematology PPT Flashcards Unit 1 How were HAZCOM standards administrated by OSHA? When did Occupational Exposure to Bloodborne Pathogens become law? Occupational Exposure to Bloodborne Pathogens standard requirements: Know how to handling medical waste: How did the CDC and CLSI involve in the safety precaution standards? What did CDC provide in HIV prevention and treatment? How did the HIV-1 prevention administrated? include requirements for the use of standardized signal words, pictograms, hazard statements, and precautionary statements • A specified format for safety data sheets (currently known as material safety data sheets) Related revisions to definitions of terms used in the standard and requirements for employee training on labels and safety data sheets Legislation on chemical hazard precautions, such as state “right to know” laws, and OSHA document 29 CFR 1910 set the standards for chemical hazard communication (HAZCOM) and determine the types of documents that must be on file in a laboratory. 1. March 1992 Regulation requires that laboratories develop, implement, and comply with a plan that ensures the protective safety of laboratory staff to potential infectious bloodborne pathogens, hepatitis B virus (HBV), and human immunodeficiency virus (HIV). The law further specifies the rules for managing and handling medical waste in a safe and effective manner. The CDC also recommends safety precautions concerning the handling of all patient specimens, known as standard precautions. New the CLSI also establish guidelines for laboratory work in regard to the protection from bloodborne diseases spread through contact with patient specimens. CDC provides recommendations for treatment after occupational exposure to potentially infectious material. The recognition of HIV-1 generated new policies from the CDC and mandated regulations by OSHA: Guidelines "Recommendations for Prevention of 20 Hematology PPT Flashcards Unit 1 When did HHS regulations pass? Does HIV transmit through human saliva? What were the OSHA requirements for an employer? How many cases were estimated of needlestick injuries occur in US each year? What is the most risk device that is caused injuries? What is the most infected HIV varieties at workplace? How does the HIV transmission? HIV Transmission in Health-Care Settings" Dept. of Labor, OSHA has “Occupational Exposure to Blood-borne Pathogens" US Department of HHS regulations for Implementing the Clinical Laboratory Improvement Amendments of 1988 How did the HIV transmit into human body? HIV has been isolated from blood and body fluids for example semen, imaginal secretions, saliva, tears, breastmilk, cerebral spinal fluid (CSF), amniotic fluid, and urine, but only blood semen factional secretions and breastmilk have been implicated in transmission of HIV to date new recently, sperm cells themselves have been discovered to be able to be capable of transmitting HIV. Evidence for the role saliva in the transmission of the virus is unclear, but standard precautions do not apply to saliva uncontaminated with blood. Provide a safe work environment. OSHA mandates that an employer − Educate and train all healthcare workers in standard precautions and in preventing bloodborne infections. − Provide proper equipment and supplies, e.g., gloves. Monitor compliance with the protective biosafety policies. The CDC estimates that more than 380,000 needlestick injuries occur in US hospitals each year 61% of these injuries are caused by hollow-bore devices. Blood is the most frequently advocated infected body fluid and HIV and HBV exposure in the workplace. Occupational exposure is a percutaneous 21 Hematology PPT Flashcards Unit 1 What is the HIV prevention procedure among healthcare personnel? What will be the higher risk of HIV infection? How risk does a non-intact HIV transmit through human skin or mucous membranes? What were the risks of HIV infection? When did the needlestick Safety and Prevention become law? What were the requirements for needlestick Safety and Prevention Act? injury, for example needlestick or cut with a sharp object, or contact by mucous membranes or nonintact skin (especially when the skin is chapped, Abraded, or affected with dermatitis), or the contact is prolonged or involves an extensive area with blood, Tissues, blood-stained body fluids, body fluids to which standard precautions apply, or concentrated virus. Among healthcare personnel with documented occupationally acquired HIV infection, prior percutaneous exposure is the most prevalent of infection. Certain percutaneous injuries carry a higher risk of infection. 1) A deep injury late stage HIV disease in the source patient 2) Visible blood on the device that caused the injury Injury with a needle that had been placed in a source patient's artery or vein There are a small number of instances when HIV has been acquired through contact with non-intact skin or mucous membranes: a) Splashes of blood in the eye Aerosols The risk of infection not only varies with the type of exposure but also may be influenced by: q) Amount of infected blood in the exposure Length of contact with infectious material r) Amount of virus in the patient's blood or body fluid or tissue at the time of exposure Needlestick Safety and Prevention Act became law, November 6, 2000. 1) Requires healthcare employers to provide safety engineered sharp devices and it'll assist him to employees to reduce the risk of occupational exposure to HIV, 22 Hematology PPT Flashcards Unit 1 What was the good news in Occupational Exposure to Bloodborne Pathogens recently? How was the risk of HIV transmission? What is used as the most widespread control measure required by OSHA and CLSI in sharps prevention? What is the primary purpose of a sharps container? Where are sharps containers to be located? Who should carry these red, puncture-resistant containers in their collection trays? How should needles not be placed in the container? What does the use of special sharps containers allow? What is the recommendation of the manipulation of any “sharp” by hand? hepatitis C, and other bloodborne disease. 2) Expands the definition of engineering controls to include devices with engineered sharps injury protection. 3) Requires that exposure control plans document consideration and implementation of safer medical devices designed to eliminate or minimize occupational exposure. 4) Annual review of occupational exposure implementation 5) Requires each healthcare facility to maintain a sharps entry along with detailed information regarding cutaneous injuries Requires employers to solicit input from healthcare workers when identifying and selecting sharps and document process. Good news-most occupational exposures do not result in infection • The average risk of HIV transmission after exposure to infected blood is low-about three per 1000 entries. Puncture-resistant sharps containers. To eliminate the need for anyone to transport needles and other sharps while looking for a place to discard them. Located in the patient areas as well as conveniently placed in the laboratory. Phlebotomists. Needles should not project from the top of the container. It permits quick disposal of a needle without recapping and other sharp devices that may be contaminated with blood. It is recommended that you not recap, bend, break, or otherwise manipulate any needle or lancet device. 23 Hematology PPT Flashcards Unit 1 How have most needlestick accidents occurred? How can other accidents happen? How can these disposal-related exposures be eliminated? How are sharps containers discarded? Who should you report your needlestick injury to? Medical personnel must be aware that what two viruses are totally different? How common is exposure to HIV in an occupational transmission to a healthcare personnel with no other know high risk factors? Why shouldn’t HIV be underrated? What is the least likely to occur if proper safety practices are followed? What is fatal and more probable than HIV? Which virus is found in lower concentrations of blood and which is found in higher concentrations of blood? How many days does HIV retain infectivity for? What was the leading occupationally acquired infection of healthcare workers before the invention of its vaccine? Approximately how many healthcare workers are still infected with HBV each year following occupational exposure? What factors does the likelihood of infection after exposure of HBV or HIV depend on? What federal standard did OSHA issue in 1991 as a mandate to employers to provide? During the recapping of a needle after phlebotomy. During housekeeping, when contaminated sharps are left on a bed, concealed in linens or disposed of improperly in a trash can. With the proper use of sharps containers. The containers are closed and placed in biohazard waste. Either the supervisor or another designated individual. HBV and HIV. Uncommon but it has been documented. Although is an unlikely work-related hazard, it can be fatal. HIV. HBV. HIV is usually found in lower concentrations where as HBV is found in higher concentrations and is present in blood or blood products. Three days in dried specimens at room temperature, one week in an aqueous environment at room temp. Hepatitis B virus (HBV). 800. The concentration of the virus in the sample (HBV has a higher level of viral concentration than HIV), if there are any skin lesions or abrasions on the exposed skin of the healthcare worker, and the immunity status of the healthcare worker for HBV. It requires employers to provide the hepatitis B vaccine to all employees at no cost to them who have or may have 24 Hematology PPT Flashcards Unit 1 What must an employee do if they refuse a vaccine? What is the best prophylaxis against blood-borne pathogen exposure? What is given if an individual has not been vaccinated for HBV and is exposed to hepatitis B in a penetrating injury? If administered in accordance with the manufacturers directions, what are both of these products considered? What is the most important strategy for reducing risk of occupational HIV transmission? What organization has issued guidelines for the management of healthcare personnel exposures to HIV and recommendations for PEP. Why is occupational exposure considered to be an urgent medical concern? What should the lab staff members be informed of if an accidental occupational exposure does occur? Why should a course of action be planned ahead of the occurrence of an actual incident? If a “source patient” can be identified, what should the work up then include? How do the patients rights in regard to testing of a source patient vary? What does the ACIP recommend after Skinner mucosal exposure to blood? If an individual has not been vaccinated, what is given? What does HBIG contain? What should the doctors be alerted of if an exposure occurs? If a parenteral exposure takes place, what should a laboratory professional do? Monitoring and follow-up counseling should be what? What happens if voluntary informed consent is obtained? When should the laboratory professional be had an occupational exposure to blood or potentially infective materials. They must sign a declination form. Vaccination against HBV and compliance with precautions. Hepatitis B immune globulin (HBIG) is given concurrently with hepatitis B vaccine. Both (HBIG and hepatitis B vaccine) are considered safe and proven free of any risk of infection with HBV or HIV. To prevent exposures but there should be a plan for post exposure management. The CDC. To ensure timely post exposure management. They should be informed of their options for treatment. Because it can trigger an emotional response. The work up should include testing the patient for various infectious diseases. The laws vary from state to state. Immunoprophylaxis, depending on several factors. HBIG is usually given within 24 hours, concurrently with hepatitis B vaccine. Antibodies to HBV and offers a pump but short lived protection. Risk of infection, and be evaluated medically for any history, signs or symptoms consistent with HIV infection. They may request follow-up monitoring for hepatitis or HIV antibodies. Provided free of charge. The source of the potentially infections material and the technical/technologist should be tested immediately. Immediately, but also at intervals after 25 Hematology PPT Flashcards Unit 1 tested? What should be filed after exposure? What are not recommended for PEP or hepatitis C? What are some steps you must follow after postexposure? exposure. An injury report. Immune globulin and anti-viral agents (interferon with or without ribavirin). * Although the most important strategy for reducing the risk of occupational HIV transmission is to prevent occupational exposures, plans for post exposure management of healthcare personnel should be in place. * The CDC has issued guidelines for the management of healthcare personnel exposures to HIV and recommendations for PEP. * An occupational exposure should be considered to be an urgent medical concern to ensure timely post exposure management. * If an accidental occupational exposure does occur laboratory staff members should be informed of options for treatment. * Because a needle stick can trigger an emotional response it is wise to think about the course of action before the occurrence of an actual incident. When can a TB test come out to be a false When the healthcare worker has recently negative? spent time with and been exposed to someone with active TB, their skin test may not yet be positive. When will a healthcare worker need to get a They may need a second skin test 10 to second Tb test? 12 weeks after the last time they had contact with the infected person. How long does it take for the immune system to It can take up to several weeks after the react to the TB skin test? exposure. What does a second negative TB test mean? They may need a second skin test 10 to 12 weeks after the last time they had contact with the infected person. What should workers who have strongly positive They should be evaluated clinically and reactions, with a skin test diameter greater than 15 microbiologically, and two sputum mm, and symptoms suggestive of TB do? specimens collected on successive days should be investigated for TB by microscopy and culture. What are some vaccines that all lab staff needs to Rubella and Hepatitis B have if antibodies are not demonstrable? Why is immunization of all lab staff important? Individuals are recognized for being at 26 Hematology PPT Flashcards Unit 1 What is an important component of a health care organization? Where can programs’ information about employees’ vaccination be found? What are some major considerations of employees’ vaccination program information’s? Preemployment health profiles with baseline screening of students in laboratory staff should include? What is something that a laboratory must always have? What does a SDS contain? How long does each lab requires to evaluate the effectiveness of its plan? Who should the written plan be available to? What must a lab written plan include? Because many hazards in the clinical laboratory happened, what word was created? Why is this word posted throughout the lab? Where can you encounter potential risk? How does an infection occur in the lab? Where are laboratory policies found? Where are manuals frequently published, and risk for exposure to, and possible transmission of, diseases that can be prevented by immunizations. A well-planned and properly implemented immunization program. They are available from advisory committee on immunization practices hospital infection controls practices advisory committee and CDC. Space characteristics of healthcare workers employed an individual served, as well as the requirements of realtor agencies and local, state, and federal regulations. An immune status evaluation for hepatitis B, rubella, and measles at a minimum. Each laboratory must have an up-to-date safety manual. This manual contains a comprehensive listing of approved policies, accept practices, questions including standard precautions. At least annually And two updated as necessary. Employees The purpose and scope of the plan, references, definitions of terms and responsibilities, and detailed procedural steps to follow. A uniquely special term biohazard was devised. To denote infectious materials or agents that presents a risk to humans’ health or animals and the laboratory. Through direct infection or through the environment. During the process of specimen collection or from handling, transporting, or testing the specimen. They are included in the laboratory reference manual that is available to all hospital personnel. They are frequently published online 27 Hematology PPT Flashcards Unit 1 what do they contain? Where are approved policies regarding the reporting of abnormal values are clearly stated in? What is a very important safety precaution? When should hand washing be performed? and contain information regard patient preparation for laboratory tests. In the safety manual. Hand washing After contact with patients and laboratory specimens. Gloves should be used as an? 1)____and not as a? 1) Adjunct 2) ______ for?______. 2) Substitute 3) Hand washing What is the efficacy of hand washing? Reducing transmission of microbial organisms. When, at the very minimum, should hands be 1) After completing laboratory work and washed with soap and water (if visibly soiled) and before leaving the laboratory. or by hand anti-sepsis with an alcohol-based hand 2) After removing gloves. rub (if hands are not visibly soiled)? Glove quality variability with leakage in 4% to 63% of vinyl gloves and 3% to 52% of latex gloves 3) Before eating, drinking, applying makeup, and changing contact lenses, as well as before and after using the lavatory. 4) Before all activities that involve hand contact with mucous membranes or breaks in the skin. 5) Immediately after accidental skin contact with blood, body fluids, or tissues. When should the gloves be removed and hands thoroughly washed? What should you do if accidental contamination occurs to an exposed area of the skin or because of a break and gloves? Two important points in the practice of hand hygiene technique are: If the contact occurs through breaks in the gloves One must wash first with the liquid soap, rinse well with water, and apply a 1:10 dilution of bleach or 50% isopropyl or a full alcohol. Then the bleacher alcohol is left on the skin for at least one minute before final washing with liquid soap and water. 1) When decontaminating hands with the waterless of antiseptic agent (e.g., an alcohol-based hand rub), apply product the palm of one hand and rub hands together, covering all surfaces of hands and fingers, until hands are dry. Follow the manufacturer's recommendations on the volume of product to use. If an 28 Hematology PPT Flashcards Unit 1 adequate volume of an alcohol-based hand rub is used it should take 15 to 25 seconds for hamster dry. 2) When washing with a nonantimicrobial or antimicrobial soap, wet hands first with warm water, apply 3 to 5 mL of detergent to hands, and rub hands together vigorously for at least 15 seconds, covering all surfaces of the hands and fingers. Rinse hands with warm water and dry thoroughly with a disposable towel. Use the tile to turn off. What does PPE stand for ? Who is responsible for regulating standards and guidelines to protect employees from exposure of pathogens present in human blood and body fluids ? What does PPE mean? What are some examples of PPE use Use of latex free is provided by the healthcare to use when dealing with personnel with sensitivity to latex? You do not need to use of gloves when working in the laboratory processing area ? When performing phlebotomy procedure for each patient you must wear gloves and disposed of them in a proper biohazard container the one that is provided by your work facility and should use of a new pair of gloving for each new patient ? A laboratory coat should be used whenever laboratory personnel are working with potentially infectious specimens. Coats that become soil with blood or body fluids can still be use and could be disposed in a regular bid trash What is a disinfected ? What is use as a multi-barrier strategy to prevent healthcare associated infections All work areas should be disinfected by the employee Personal Protective Equipment OSHA Personal protective equipment use of specialized clothing or equipment used by workers to protect from direct exposure to blood or other potential infections or hazardous material Gloves Laboratory facial shields mask Eye protection and breathing apparatus True False True True False Eliminates many or all pathogenic microorganisms except for bacterial spores on in and objects Disinfectant True 29 Hematology PPT Flashcards Unit 1 at the beginning and end of shift or when needed to prevent infection to patient and staff ? There is no need of use of gloves when disinfecting an area with a 1 to 10 dilution of household bleach or EPA registered disingfectant? What is the most widely used chlorine product of aqueous solutions of 5.25% to 6.15% disinfectants? Which is a broad spectrum of antimicrobial activity and does not leave a toxic residue and is unaffected by water hardness ? A disinfectant of bleach should have a dilution of _____concentrated bleach solution ? How employer should clean and the dilution at work? When instruments such as scissors or centrifuge carriages to be sanitize? Where are disposable materials contaminated with blood must be placed? Where disposable materials contaminated with blood must be placed in? How treat an area contaminated by either blood or body fluids needs What is protocol recommended for managing spells in the clinical laboratory? False Hypochlorite Bleach 1:10 While wearing gloves employers should clean and sanitize all work surfaces at the beginning and end of their shift with household bleach 1:10 dilution Before and after the workday with the diluted solution of bleach For example about studies have demonstrated the HIV is inactivated rapidly after being exposed to common chemical genocides at concentrations that are much lower than those used in practice. Disposable materials contaminated with blood must be placed in containers marked quote Biohazard" properly discarded containers marked quote Biohazard Potentially hazardous, with prompt removal and surface disinfection. Neither HBV (or HCV) nor HIVAs being transmitted from a housekeeping surface, e.g. countertops - Wear gloves and a laboratory coat. - Absorb the blood with disposable towels. Remove as much liquid blood or serum as possible before decontamination. - Using a diluted bleach (1:10) solution, clean the spill site of all visible blood. - Wipe down the spill site with paper towels soaked with diluted 30 Hematology PPT Flashcards Unit 1 Who need programs to minimize risks to? How to maintain safe operations? How general infection control safety practices What is autodilutor? How general infection control safety practices? bleach. - Place all disposable materials used for decontamination into a biohazard container. Decontaminate nondisposable equipment by soaking overnight in a dilute bleach (1:10) solution and rinsing with methyl alcohol and water before reuse. Disposable glassware or supplies that have come in contact with blood should be autoclaved or incinerated. The health and safety of employees, volunteers, and patients. 2. Suitable physical arrangements, and acceptable work environment, and appropriate equipment need to be available to maintain safe operations. • All devices in contact with blood that are capable of transmitting infection to the donor or recipient must be sterile and nonreusable. • Food and drinks should not be consumed in work areas or stored in the same area as specimens. Containers, refrigerators, or freezers used for specimens should be marked as containing a biohazard. • Specimens needing centrifugation should be capped and placed into a centrifuge with a sealed dome. Rubber-stoppered test tubes are opened slowly and carefully with a gauze square over the stopper to minimize aerosol production (the introduction of substances into the air). 1. Autodilutors or safety bulbs are used for pipetting. Pipetting of any clinical material by mouth is strictly forbidden (see following discussion • No tobacco products can be used 31 Hematology PPT Flashcards Unit 1 How to use pipetting safeguards? How specimen processing protection What can result in an occupational exposure in Hematology lab? What covered a cap when removed from a specimen tube or a blood collection tube? in the laboratory. • No manipulation of contact lenses or teeth-whitening strips should be done with gloved or potentially infectious hands. • Do not apply lipstick or makeup. 2. All personnel should be familiar with the location and use of eyewash stations and safety showers. Pipetting must be done by mechanical means. Such a device is a bottle top dispenser that can be used to deliver repetitive aliquots of reagents. It is designed bottle mounted system that can dispense selected volumes in an easy, precise manner. • Is usually trouble-free and requires minimal maintenance. • Protective gloves should always be worn for handling any type of biological specimen. • Bio hazards are generally treated with great respect in the clinical laboratory. • the adverse effects of pathogenic substances on the body are well documented. • The presence of pathogenic organisms is not limited to the culture plates in the microbiology laboratory. Airborne infectious particles, or aerosols, can be found in all areas of a laboratory where human specimens are used. 1. In the hematology laboratory, centrifuge accidents or the improper removal of rubber stoppers from test tubes, produce airborne droplets (aerosols) that can result in an occupational exposure. 2. the top should be covered with a disposable gauze pad or a special 32 Hematology PPT Flashcards Unit 1 What can reduce contamination of gloves? How the tube should be held? What happen if snapping off the cap top? When not in place on the tube, what should kept? When specimens are being centrifuged, How the tube caps should kept? Should stopped centrifuge by the worker? What should be taken to control the hazard from aerosols? Where constructed plastic splash shields? What are laboratory safety boxes? The proper handling of blood and body fluids is critical to the accuracy of laboratory results, and the (?) of all individuals who come in contact with specimens must be guaranteed. protective pad. 3. Gauze pads with an impermeable plastic coating on one side 4. The tube should be held away from the body and the cap gently twisted to remove it. 5. Snapping off the cap top can cause some of the contents to aerosolize. 6. Kept in the gauze and not placed directly on the work surface or countertop. 7. the tube caps should always be kept on the tubes. 8. Centrifuge covers must be used and left on until the century stops. Centrifuge should be allowed to stop by itself it should not be manually stopped by the worker is to exercise caution in handling pipettes and other equipment used to transfer human specimens, especially pathogenic materials. 9. These materials should be discarded properly and carefully. • It used in many laboratories for the processing of blood specimens. Are removed behind or under the shield, which acts as a barrier between the person in the specimen to,. • This is designed to prevent aerosols rendering the nose, eyes, or mouth. Laboratory safety boxes are commercially available and can be used to remove stoppers tubes or perform other procedures that might cost spattering. Specials and safety boxes should be periodically decontaminated. safety 33 Hematology PPT Flashcards Unit 1 If a blood specimen is to be transported, the shipping container must meet what organization requirements for shipping clinical specimens. Shipping containers must meet the packaging requirements of major couriers and (?) hazardous materials regulations. Approved re-closable plastic bags for handling what type of specimens does amber bags for analysis of light-sensitive drugs are available. T or F. Some specimens must be analyzed immediately after they reach the laboratory. Blood specimens for hematology studies can be stored in the refrigerator for what amount of time before being used in testing? After storage, anticoagulated blood must be thoroughly mixed after it has reached what temperature? T or F. Plasma and serum often can be frozen and preserved satisfactorily until a determination can be performed. Whole blood cannot be frozen because RBCs ? unfreezing. Freezing preserves (?) sensitive coagulation factors a laboratory determination is best done on a fresh specimen. On the Federal level, the storage and management of medical waste is primarily regulated by who? Laws and statutes are defined by what 2 acts? The assessment of quality results for the various analyses is critical and is an important component of the operation of a high-quality (?) What type of programs monitor the following • • • • • • • • • OSHA Department of Transportation Biohazard True 2 hours room temperature. True rupture heat OSHA. The Occupational Health and Safety Act and The Clean Air Act. laboratory. Quality assessment programs Test request procedures Patient identification Specimen procurement Specimen labeling Specimen transportation and processing procedures Laboratory personnel performance Laboratory instrumentation, reagents, and analytical test procedures Turnaround times Accuracy of the final result 34 Hematology PPT Flashcards Unit 1 In 1988, the U.S. Congress enacted the what amendment in response to concerns about laboratory testing errors? What was published in the Federal Register on January 24, 2003? Clinical Laboratory Improvement Amendments of 1988 ( CLIA' 88) What type of factors support quality testing which include the following: • Qualified personnel • Laboratory policies • Laboratory procedure manual • Test requisitioning • Patient identification and specimen procurement and labeling • Specimen collection, transport, processing, and storage • Preventive maintenance of equipment • Appropriate methodology • Accuracy in reporting results and documentation Nonanalytical The entry-level examination competencies of all validated Laboratory Requirements Relating to Quality Systems and Certain Personnel Qualifications, CLIA established a minimum threshold for all aspects clinical laboratory testing of what type of testing? What also incorporates proficiency testing in the CLIA’88 regulations? A quality assessment system is divided into how Two, nonanalytical factors in the many major components? nonanalytical factors in the analysis of quantitative data (quality analysis of quantitative data (quality control [QC]). control [QC]). What type of assessment is used in the clinical Quality assessment hematology laboratory to ensure excellence in performance? Approach to quality assures that correct laboratory shortest results are obtained in the (?) possible time and a reasonable cost? The total testing process (TTP) is defined by •Preanalytical (preexamination) activities in three distinct phases related to workflow •Analytical (examination) outside and inside the laboratory, which are what? Postanalytical 35 Hematology PPT Flashcards Unit 1 certified persons and hematology must be (?). Validation takes the form of both external certification and new employee orientation to the what type of environment? T or F? Participant patient and continuing education activities is essential to the maintenance of competency and is required in some instances to maintain professional certification. Personnel performance should be monitored with 1 and 2. Quality assessment demands that a (?) monitors results of daily work and that all analytical (examination) reports produced during up to go should be evaluated for errors and omissions. Where is the Laboratory policy located? Who has access to the laboratory policy? What must each laboratory have? What must each company’s manuals contain a listing of? What must also be included in manuals? (Think large scale.) Name the 3 other sources that have mandatory and voluntary standards. Laboratory procedures should be contained in a _______ and ________ document. Where can approved policies for the reporting of results be found? Who reviews and updates the manuals? How often are manuals updated? What format of standards do manuals have to comply with? What is CLSI? To support a QC program, of methods to document a laboratory results, will be found where? What does proper documentation ensures? What does the CLSI recommends that the procedure manual follow? True or False. Does each assay done in hematology laboratory must be included in the manual? Name the 11 minimal components that are to be work environment True 1. periodic evaluations and reports reports. • Supervisor • In a laboratory reference manual. • All hospital personnel • An up-to-date safety manual Approved policies Acceptable practices • Precautions, including standard blood and body fluid precautions OSHA regulations Specific regulations that conformed with current state and general requirement JCAHO, CAP, and the CDC. Current | Complete In the laboratory procedures Supervisory staff Regularly, Annually, and as needed CLSI format standards. An internationally recognized group of laboratory professionals who lead quality assessment efforts. Procedure manual. That control specimens have been properly monitored. A specific pattern of organization. True 1. Title of the assay 36 Hematology PPT Flashcards Unit 1 included in the manual. Who can request a laboratory test? Name the 4 factors that have to be on the requisition (either hardcopy or electronic). What information accompanying a specimen must have and match exactly? When physicians need information to assist in ordering test, where will they find it? What is one of the first steps in establishing a quality assessment program for the clinical laboratory? What current information about obtaining appropriate specimens should be included in the database? It is important that patients are? What are the most common source of laboratory errors? What education assessment is an asset to specimen identification? What is a must requirement on a specimen once it has been obtained from the patient? What do computer-generated barcode labels assist in? True or False. Analytical result can only be as good as a specimen received? 2. Principle of the procedure and statement of clinical applications 3. Protocol for specimen collection and storage 4. QC information 5. Reagents, supplies, and equipment 6. Procedural protocol 7. Reference “normal" ranges 8. Technical sources of error 9. Limitations of the procedure 10. Proper procedures for specimen collection in storage Approved policies for the reporting of results • A primary care provider or, in some states, the patient. 1. The patient identification data, 2. The time and date of specimen collection 3. The source of specimen • Analyses to be performed. • Patient identification requisition. • In an online database or printed handbook. • An electronic database or handbook of specimen requirement information. Special collection requirements for various types of tests. Ordering test correctly • Transporting and processing specimen. Carefully identified Pre-analytical (preexamination) errors Computerized barcoded That specimens are properly labeled Making certain that the proper patient identification is noted on each specimen True 37 Hematology PPT Flashcards Unit 1 What is critical to the accuracy of any test? Strict adherence to correct procedures for specimen collection storage. How must specimens be transferred to the laboratory? Efficiently Name an example of special handling conditions that Placing the specimen on ice immediately some assays require? after collection. When should specimens be tested after collection to Within two hours. produce accurate results? What is important aspect of the quality assessment The documentation of specimen arrival process? times the laboratory as well as other specific test request data. What is critical to obtaining accurate results? Correct storage of specimens. What is an important issue when blood is collected at Specimen integrity a site away from the testing facility? Name two test that are samples may need to be drawn Prothrombin time [PT] and activated several hours before testing. partial thromboplastin time [aPTT]) What protocol by CLSI must blood samples collected Collection, Transport, and Processing of for PT and aPTT analysis and tubes with sodium Blood Specimens for Testing Plasmacitrate should be handled using the following when Based Coagulation Assays, 2008 collected off-site? The sample tube should remain ________ before Unopened. testing. Name 2 things that are done to a specimen once it is Centrifuged and testing received by the lab? What is important to the quality of test performance? Monitoring of the temperatures of equipment and refrigerators. What must microscopes, centrifuges, and other pieces Cleaned and checked of equipment need regularly to ensure accuracy? What all automated equipment have regularly? Preventive maintenance schedule How often should equipment such as microscopes, On a regular schedule. centrifuges, and spectrophotometers should be clean and check for accuracy? What can produce inaccurate test results and lead to Failure to monitor equipment regularly expensive repairs? Preventive maintenance of equipment includes: Instrument maintenance, reagent lot change, major component replacement, new software installation How often should labs recalibrate an analytical Every 6 months examination method? Clinical labs must follow which requirements for CLIA or the manufacturer's instrument calibration frequency? requirements How often should labs recalibrate an analytical Every six months examination method? True or False: When new methods are introduced, it's TRUE important to check the procedure for accuracy and variability. True or False: Replicate analyses using control FALSE 38 Hematology PPT Flashcards Unit 1 specimens are recommended to check for: precision and similarities between technologists How do labs monitor individual patient results? Why are delta checks investigated? What are examples of pre-analytical pre exam errors? The ongoing process of making certain that the correct lab result is reported for the right patient in a timely manner and at the correct cost is called? What is evaluated as part of the CQI process? Each lab sets the same indicators When are test results recorded and reported? Documentation is an important aspect of quality assessment What is quality control used for? The purpose of quality control is to detect errors that result from: What are quality control activities? Documentation of QC includes: Knowledge of statistics is important in hematology for which 2 reasons: What does Accuracy means in Clinical Quality Control ? What term describes comparison of an instrument measurement or reading to a known physical constant? By clinical values or the Delta check system To rule out arrows such as mislabeling of a specimen Obtaining specimens from IV lines, specimen processing error, actual changes in the patient's clinical condition Continuous quality improvement (CQI) Quality assessment indicators FALSE Whenever there is any problem or situation that might affect the outcome of the test result TRUE Monitors the accuracy and precision of a test performance over time Test system failure, adverse environmental conditions, variance: the factors or fluctuations that affect the measurement in operator performance Monitoring the performance of a lab instrument, reagents, other testing products and equipment Preventive maintenance records, temperature charts, and QC charts for specific assets. Application of statistical analyses of results and quality assessment protocols, instrumental applications of statistics to erythrocyte, leukocyte, platelet reports Accuracy is: How close a test result is to the true value. This term implies freedom from error. Reference samples and standards with known values are needed to check accuracy. Calibration 39 Hematology PPT Flashcards Unit 1 What is a Control? What is Precision? What is Proficiency testing? How is Proficiency testing obtained? Describe Standards A specimen that is similar in composition to the patient's whole blood or plasma.The value of the control specimen is known. A control specimen must be carried through the entire test procedure and treated in exactly the same way as any unknown specimen; it is must be a affected by all variables that affect the unknown specimen. Control specimens are tested daily or in conjunction with the unknown patient specimen. Controls are the best measurements of precision and made a recent normal or abnormal test values Precision is how close the test results are to one another when repeated analyses of the same material are performed. Precision reverse the reproducibility of test results. Is important to make a distinction between precision and accuracy. The term accuracy implies freedom from air; the term precision implies freedom from variation. Proficiency testing is incorporated into the CLIA requirements, with each laboratory participating in an external PT program as a means of verification a laboratory accuracy. Periodically, identical samples are sent to a group of laboratories participating in the PT program; it's laboratory analyzes the specimen, reports the results to the agency, and is evaluating grade on this results in comparison to results from other laboratories. In this way, QC between laboratories is monitored. Standards are Highly purified substances of known composition. A standard may differ from a control and it's overall composition and in the way it is handled in the test. Standards of the best way to measure 40 Hematology PPT Flashcards Unit 1 accuracy. Standards are used to establish reference points in the construction of graphs (e.g., manual hemoglobin curve) or to calculate a test result. What is the advantage of having quality controls? Quality control is a process that monitors the accuracy and reproducibility results through the use of control specimens. List some of the functions of a Quality Control Providing a guide to the functioning of Program equipment, reagents, and individual technique Confirming the accuracy of testing when compared with reference values Detecting an increase in the frequency of both high and low minimally acceptable values (dispersion) Detecting any progressive drift of values to one side of the average value for at least 3 days (trends) Demonstrating an abrupt shift or change from the established average value for 3 days in a row (shift) Why do QC testing must be repeated? After the procedure has been reviewed for any indication of error and error has been found and corrected, testing must be repeated until the control value falls within the range. Define terms such as Average, Mean, Median, Mode? Average is the Sum of the test results divided by the number of tests. Arithmetic mean value. Mean is the term used to express the average or arithmetic mean value. The mean value is 13.6 for the following series of values: 10, 11, 14, 16, and 17. •Median is the Middle value of a set of numbers arranged according to their magnitude. If two middle values exist in an even number of mathematical observations, the median is the arithmetic mean of the two middle values. The median value is 14 following five test values arranged in the order of size: 10, 11, 14, 16, 17. •Mode is the number or value that 41 Hematology PPT Flashcards Unit 1 What are the measurements of variation? What is a Standard deviation (SD)? How is Coefficient of variation (CV) obtained? occurs with the greatest frequency is 45 if the following values are obtained for controlled blood test: 45, 48, 35, 39, 51, 42, 45, 39, 45, 44, and 45. •Range: The difference between the highest and lowest measurements in the series. The range is expressed the same units as the raw data. The range is 0.5% to 2% for the following values expressed as percentages: 1, 1.5, 1, 0.5, 2.0, 1.5, and 1.0. •Variance: An expression of the position of each observation or test result in relation to the mean of the values. The variance is determined by examining the deviation from the mean of each individual value. The following test results were obtained: 3, 4, 5, 6, 8, 9, 10, 12, and 15. The variance from the mean (deviance from the mean) of each individual result is -5, -4, -3, -2 Standard deviation (SD) is Expresses degree to which the test data tend to vary about the average value (mean).To obtain a measure of the variation expressed in the same units as the raw data, the square root of the variance or the SD is used. Measure of variability,has meaning only when two or more sets of data having the same units of measurement are compared. Can be used to describe the single-set measurement. Otherwise known as related standard deviation, A statistical tool used to compare variability in non-identical data sets,the CV of each data set allows comparison of two or more test methods, laboratories, or specimen sets. Variability in each data set must be 42 Hematology PPT Flashcards Unit 1 What is the Z score? With the advent of computer technology and computerized instrumentation, many additional systems have been introduced to monitor test results numerically. What are some of those methods? Name 2 traditional approaches in monitoring Quality Control? What is represented by confidence limits from a Levey-Jennings control chart? True/False: Results that fall within the confidence limits are assumed to be accurate. True/False: It is common practice to use +/- 3 SD as the limit of confidence. Under what conditions are test results not reported? What are the 3 types of changes commonly observed in the Levey-Jennings QC approach? How would a systematic drift or trend be determined? Give 2 examples that may result in a drift/ trend. expressed as a relative rather than absolute measure. Express the SD as a percentage of the mean. •The Z score measures how many standard deviations a particular number is from the right or left of the mean. A positive Z score measures the number of standard deviations and observation is above the mean A negative Z score gives the number of standard deviations on observation and observation is below the mean. The Z score is a unit less measure. 1. Levy Jennings chart 2. The cumulative sum (Cusum) method 3. Trend line analysis 4. Power function's Instrument calibration 3. Lot-to-lot reagent changes 3. A set of mathematically established limits into which the majority of values or results will fall. 4. True 5. False; the common limit of confidence is +/- 2 SD 6. If the control assay value is outside the confidence limits, the control value and the patient's values are considered to be out of control and cannot be reported. Systematic drift or trend Increased dispersion of results 7. Shift or abrupt change in results • When the control value direction moves progressively in one direction from the mean for at least 3 days. Deterioration or expiration of a 43 Hematology PPT Flashcards Unit 1 • What are some disadvantages to the Cumulative sum (Cusum) method? Frequency distribution: Histogram: What is the term used to describe values that fall outside the confidence limits? The Gaussian distribution is also known as? Errors occurring within the process of phlebotomy may cause serious harm to patients either directly or indirectly. What are the included critical areas? True or False. The accuracy of laboratory testing begins with the quality of the specimen received by the laboratory. True or False In phlebotomy, quality does not depend on how a specimen was collected, transported, and processed. True or False Quality assessment, as it applies to phlebotomy, includes preparation of a patient for any specimens to be collected. True or False Collection of valid samples and proper specimen transport are not included in the Quality Assessment in phlebotomy. When collecting blood specimens, it is important that reagent used Diluent contamination affects erythrocyte and leukocyte controls with an upward trend as bacterial growth increases. Too many out-of-control results are obtained Does not readily control for random error (precision). In any large series of measurements (test results) of a normal population, the results are evenly distributed about the average value. 10. Grouping of data in classes and determining the number of observations that fall in each of the classes 1. Bar chart that provides immediate information about a set of data in a condensed form 2. Out-of-control 3. The bell-shaped curve Appropriateness of the test request. Patient and sample identification. Criteria for acceptance and rejection of specimens. Communication and interpretation of results. True False (quality DEPENDS on how a specimen was collected, transported, and processed.) True False (Collection of valid samples and proper specimen transport are included in the Quality Assessment in phlebotomy.) The rights of the patient at all times. 44 Hematology PPT Flashcards Unit 1 the phlebotomist considers what? True or False The professional image of the laboratory is solely represented by the phlebotomist. True or False It is important to be gentle and treat pediatric patients with compassion, empathy and kindness True or False Phlebotomists must be relaxed and perceptive about any anxiety that adolescent patients may have. True or False It is okay to demean geriatric patients because they are really old and they cannot understand anything. A __________collected blood specimen is essential to quality performance in the laboratory Strict adherence to the rules of specimen collection is critical to the _______ of any test. In hematological tests/studies, what is the type of specimen most frequently used? What do you call the substance that prevents clotting when mixed with fresh whole blood? What do you call the straw-colored fluid from an anticoagulated blood? True (Because phlebotomist is the only laboratory staff member that a patient sees.) True True False Properly Accuracy Anticoagulated blood Anticoagulant Plasma White blood cells and platelets. What composes the BUFFY COAT? What type of additive/anticoagulant can be found in a green top tube? A vacutainer/tube with a purple top contains what Heparin Tripotassium 45 Hematology PPT Flashcards Unit 1 type of anti-coagulant? A vacutainer/tube with a lightblue top contains what type of anti-coagulant? Additives can alter the constituents and can have ________ amounts. A. Correct B. Incorrect C. Non-consequential None of the above All employees should learn to use engineering tools. They also must: A. Evaluate B. Select C. Document All of the above Can needles be removed in rare circumstances? Must usage of all needles be covered by the Exposure Control Plan? Name some factors that impact the quality of blood collection. Choose two. A. Ambient Temperature, Altitude B. Humidity, Sunlight C. All of the above D. None of the Above Most evacuated tubes have shelf lives of: A. 2 months B. 4 months C. 8 months 12 months Blood tubes can use several types of Anticoagulants. List three. A. Sodium Citrate B. Heparine C. K2, EDTA All are blood tube Anticoagulants. True or False. Is the correct order of draw? Yellow, Light Blue,Gold, Red, Red, Orange, Green, Lavender, White, Gray For general protocol a phlebotomist should.. A. Introduce themselves B. Clearly explain the procedure C. Friendly courtesy in the patient’s native language. All of the above Wristbands can be a major source of preanalytical error. Name several error that can ethylenediaminetetraacetate (EDTA) Sodium citrate B D Yes Yes C D D True D D 46 Hematology PPT Flashcards Unit 1 occur. A. Wrong wristband B. Wearing more than one or none C. Wristband ink is smudged or old All if the above are errors What needs to be checked, assembled before blood collection and what needs to be labeled after blood collection? Test requisitions should be checked and the appropriate evacuate tubes assembled. All specimens should be properly labeled immediately after the specimen is drawn. What is usually found on the label of the specimens during blood collection? The patient’s name, unique identification number and room number or clinic, and date and time of collection are usually found on the label. What type of disposable needles are required during blood collection? Sterile disposable needles (doublepointed or syringe type) What emergency equipment is necessary to prevent fainting during blood collection? Spirits of ammonia breakable capsule. During initiation of the venous blood collection what is the first step after introducing one’s self? What PPE is required to be worn prior to blood collection? How does the syringe/needle and evacuated tube/needle differ in their preparation prior to blood collection? Identifying the patient. What the person collecting the blood do prior to selecting the vein for venipuncture? Gloves (Nitrile) If a needle and syringe are to be used, firmly secure the hub of the needle with its shield in place on the syringe. If an evacuated tube is to be used, the plastic shield is to remain on the needle until immediately before the venipuncture. Visually inspect both arms. In the arm, what are the three veins to be used for venipuncture? Cephalic, basilic, and median cubital. How does one apply the tourniquet? First one must place the tourniquet under the arm and adjust the tourniquet evenly then place tension on the tourniquet, cross one side over the other, and slip a small loop under one side of 47 Hematology PPT Flashcards Unit 1 How does one find a suitable vein for venipuncture? What are the possible sources of pre-analytical error in venipuntures? Prior to puncturing the vein, what must one do in order to prevent bacterial contamination/infection? After the needle is inserted in the puncture site and the tube is placed what is next? After all the tubes are filled, how does one terminate the procedure? How does one respond when the patient refuse to have his/her blood drawn? How does one minimize the movement of the vein during venipuncture? Why does a lack of blood volume obtained during venipuncture or a “short draw” cause problems? When performing phlebotomy and collecting a blood sample, can you use any anticoagulant tube for any given test ? Can sudden movement of the patient or phlebotomist affect the factor for analyze of the blood sample obtain? the tourniquet. By palpitating it. Edema of the extremities IV lines Scarring or burn patients Dialysis patients Postmastectomy patients 3) The puncture site must first be After the site is prepared with an alcohol sterile wipe. 4) Remove the tourniquet. 5) The procedure is terminated by covering the venipuncture site with a square of sterile gauze and applying pressure. A sterile adhesive bandage is then placed on the site. 6) Politely excuse yourself from the patient’s room, note the refusal on the requisition, and notify the hematology supervisor 7) Always have firm pressure on the arm below the intended venipuncture site. The needle can be moved to reach the vein, but excessive probing in the tissues must be avoided. 8) An excessive amount of EDTA in the evacuation tubes will produce shrinkage of erythrocytes, and an insufficient amount of blood in a sodium citrate tube will introduce a dilutional problem if the specimen is tested for coagulation studies. No, improper anticoagulant for blood smears cannot be prepared from a heparinized blood sample will give a false diagnosing using the wrong anticoagulant tube Yes, sudden movement by patient or phlebotomist will cause the needle to come out prematurely and cause a false 48 Hematology PPT Flashcards Unit 1 What does it mean to take quick action and void the phlebotomy procedure? What causes a hematoma ? True or false It is correct to apply firm pressure until bleeding has stop or for about 2min? True or false any tubes containing an anticoagulant should be gently inverted several times to mix the specimen What causes a blood clot formation in a anticoagulated tube? When a patient tells you verbally she or he is a fainter when drawing their blood what is the next step you should take ? Of the following personnel, only a high school diploma is required of which one? Which one of the following is a hematology test? Which lab department would perform a hemogram ? This department examines specimens microscopically for the presence of crystals, casts, bacteria, and blood cells There times where you will get patients where their veins are much more smaller or hidden veins, what are steps you can take for difficult blood draws ? what are some special to considered when havins a pediatric patient you should consider as a professional phlebotomist ? Is is okay to slap the arm to dilate the vein because factor for analyze. To immediately remove the tourniquet and place a gauze pad on the venipuncture site and apply pressure until bleeding has completely stopped. When there is not enough pressure apply to the site of venipuncture. True True Have the patient lay down in a appropriate room given by facility or hospital Phlebotomist CBC complete blood count Hematology Urinalysis Adjust the position of the arm elbow out Use a smaller gauge needle Use a small syringe Use a butterfly neddle and multiple small syringes Tighten the tourniquet Loosen the tourniquet Apply hot packs to the arm Use a second tourniquet below the site Use a hand or wrist vein or veins on the underside of the arm work quickly on premature infants warm the blood collection site for 5 min this will increase blood flow check potential blood collection sites for redness or bruising Do not attempt venipuncture unless obtaining enough blood collection for all ordered tests in one attempt is certain No, you shouldn’t slap the vein when 49 Hematology PPT Flashcards Unit 1 you cant feel it enough when performing performing venipuncture venipuncture ? What is a good practice to take when you have a Carefully identify the patient check the elderly patient that may be confused and disoriented ? requisite make sure you have the right patient What some considerations for geriatric patients to Warm up the skin consider if the patients limb feels cold and clammy True or false when the skin is fragile it is okay True placing the tourniquet over the clothing for more comfort for the patient What will you consider when prepping the vein and Consider using a smaller gauge needle you feel it being a small or fragile vein? Is it okay when performing venipuncture to have a No, you shouldn’t have a shaky hand shaky hand and inserting the needle in this form ? should use one quick swiff motion when inserting the needle After you have finish your blood collection tubes You should pay special attention to the you are getting ready to but a bandage or tape on the fragility of the skin skin sight you have puncture what is something you should pay attention too before determining what gauze to use ? What is the preferred site for the collection of Lateral and medial side of the capillary blood from the finger ? fingerprint What is the preferred site for a infant heel stick? Medial and lateral site What is the correct way to prepare a blood smear? Once a small drop of blood has spread by capillary action between the coverslips they should be pulled apart smoothly in a horizontal plane. The proper angle of the pusher slide is approximately 45 angle Why is it important to smear the blood as soon as the A delay in a smear preparation will be drop is placed on the slide? larger cells such as neutrophils and monocytes will be disproportionately located at the feathered edge when examined microscopically Why is important to have the appropriate size of Too large a drop of blood will produce blood droplet in a smear sample? a think, long smear. And to small drop of blood will produce a thin short smear True or false slides should be free of dust and grease True spots? What 3 things determine the thickness of the smear ? Angle of the spreader slide angles thinkness Size of blood drop Speed of spreading Explain how to adjust the thickness of the smear with Decrease angle of spreader slide a high hematocrit Explain how to adjust the thickness of the smear with Increase angle of spreader slide 50 Hematology PPT Flashcards Unit 1 a low hematocrit List 4 technical causes of a poor blood smear What are some stains that are alcoholic solutions with basic and acidic components The wrigh’s stain is a _________stain. What is used to wash off stain ? What is a source of error when failure to filter the stain daily or before use ? If the precipitated sediment is very ____ it will be impossible to view the blood cell microscopic examination True or false improper timing of the stainining or buffering can produce faded staining or altered colors of the blood smears and too short a staininh time produce a blood smear that is too red on microscopic examination and if the staining time is too long the blood smear will be to dark on microscopic examination. Spreader slide is pushed in a jerky manner Failure to keep entire edge of spread slide against the slide while making smear Failure to push spreader slide completely across Romanowsky based stains such as wright, giemsa or may-grunwald stains Romanowsky Distilled water Failure to filter the stain daily or before use can produce sediment on blood films Heavy True A. Microtubules B. Centriole C. Membrane D. Nucleus E. Nuclear membrane F. DNA G. Golgi apparatus H. Mitochondrion I. Lysosome J. Cytoplasm K. Nucleoli L. Rough ER M. Smooth ER 51 Hematology PPT Flashcards Unit 1 A. Phospholipids B. Protein A. Normal B. Hypotonic C. Hypertonic Diffusion is: Active transport is: Active transport requires: Na/K pump is active or passive? Maintenance of a constant volume despite extracellular and intracellular osmotic challenges is critical to the integrity of a cell In order to return cell volume to its normal resting state, how do cells respond? What is essential for the normal function and survival of cells? What is highly pleomorphic and has bizarre cytologic features associated with malignant tumors? What is atrophy? What has abnormal cytologic features and tissue organization What is hyperplasia What is hypertrophy What is metaplasia Organelles are functional units of a cell What are the two central spots inside of the centrosomes. What is the extensive lace-like network composed of membranes enclosing interconnecting cavities or A passive process whereby fluid moves through a semipermeable membrane Movement of a molecule against the concentration gradiant. ATP Active True by swelling or shrinking by activating specific metabolic or membranetransport processes Cell volume homeostasis Anaplasia decrease in the number or size of cells Dysplasia The increase in the number of cells in a tissue The increase in the size of cells It is the change from one adult cell type to another True Centrioles Endoplasmic reticulum 52 Hematology PPT Flashcards Unit 1 cisterns called? What are the 2 classifications of the endoplasmic reticulum? Which part of the ER can the ribosomes be found? What appears as a horseshoe-shaped or hook-shaped organelle with an associated stack of vesicles or sacs. What do lysosomes contain? What are microbodies? What are microfilaments? What are microtubules? What is composed of an outer smooth membrane and an inner folded membrane? What is the function of the mitochondria? What are small dense granules, that show a lack of membrane and are found both on the surface of the rough ER and free in the cytoplasm? Ribosomes contain a significant portion of RNA and are composed of unequally sized subunits. The presence of many ribosomes produces cytoplasmic basophilia (blue color) when a cell is stained with Wright stain. Where is the site of protein synthesis? What is a long-chain polysaccharide that is detectable with the PAS stain? What is the PAS stain? Ferritin is a common storage form of iron. Ferritin is often found in iron-rich dense bodies called _______. What term is used to refer to iron-saturated telolysosomes? Histologists refer to granular, iron-rich pigment as ________. The nucleus is surrounded by a _______ ______, which consists of an inner and outer membrane. Inside the nucleus, within the inner nucleoplasm, are the _______ and _______. Chromatin dictates the nature of ________ that can be synthesized, thereby controlling the function of the cell. Rough and smooth Rough sections Golgi apparatus Hydrolytic enzymes small, intracytoplasmic organelles, limited by a single membrane that is thinner than the lysosome. solid structures, consisting of the protein actin and the larger myosin filaments small, hollow fibers composed of polymerized, macromolecular protein subunits, tubulin. mitochondria carry out the energy-producing reactions of the cell Ribosomes True True The complex of the messenger RNA and a ribosome Glycogen Periodic acid-Schiff stain True Telolysosomes Siderosome Hemosiderin Nuclear envelope Nucleoli, chromatin Protein 53 Hematology PPT Flashcards Unit 1 Chromatin transmits information for cellular control from one generation to the next. Proteins associated with the nucleic acids are divided into basic, positively charged ______, and less positively charged ______. Histones are believed to be essential to the structural integrity of ______. Histones are important in facilitating the conversion of the thin chromatin fibers seen during ______ into the highly condensed chromosomes seen in _______. Nonhistones are thought to play other roles, including ________ _________. What is the general model of the organization of DNA and histones? What is the complete unit, consisting of a string of DNA wrapped around a histone core, called? What is deletion? What is translocation? What is trisomy? What is clinical use of cytogenetics? What are three sub-phases of interphase? What are four phases of mitotic division? What is M phase? What is Prophase? What is metaphase? True Histones, nonhistones Chromatin Interphase, mitosis Genetic regulation A regular spacing arrangement Nucleosome is defined as the loss of a segment of chromosome. is the process in which a segment of one chromosome breaks away (is deleted) from its normal location. is the failure of a homologous chromosome to separate from its sister chromatid. This leads to a set of three chromosomes in place of the normal pair. Clinical cytogenetic contributes to understanding inborn or acquired genetic problems by providing a lowpower screening method for detecting isolated or missing chunks of chromosomes. – G1, first gap – S phase G2, second gap M phase Prophase Metaphase Anaphase a. Telophase is the period of actual cell division. is the period of replicated strands of chromatin that become tightly coiled, distinctive structures. is the period when identical sister chromatids move to the center of the 54 Hematology PPT Flashcards Unit 1 What is Anaphase? What is Telophase? What is karyokinesis? What is cytokinesis? What are the activities of the nucleus? What is a means of distinguishing a morphologically distinctive form of programmed cell death that is associated with normal physiology? spindle (the equatorial plate). begins as soon as the chromatids are pulled apart and lasts until the newly formed chromosomes reach the opposite poles of the spindle. is the period when the chromosomes arrive at opposite poles of the cell in early telophase. Nuclear division Division of cytoplasm Apoptosis 55 Hematology PPT Flashcards Unit 1 What is Meiosis division? What is a segment of DNA that is arranged along the chromosome at a specific position called a locus? What is the coding sequences of a gene? A gene What is the intervening sequences of a gene? What is the term that causes a change in the gene? What is sickle cell mutation? Introns Mutation Figure 3.11 Sickle cell trait and anemia. When two persons with sickle cell trait (genotype: A/S) produce offspring, the expected genotypic ratio is 1:2:1, or a 25% chance of offspring with a normal hemoglobin (A/A), a 50% chance of offspring with sickle cell trait (A/S), and a 25% chance of offspring with sickle cell anemia (S/S). Hgb, hemoglobin. Exons 56 Hematology PPT Flashcards Unit 1 The hemoglobin S amino acid sequence differs from hemoglobin A amino acid sequence. This difference is due to one amino acid residue on the _____ chain of the hemoglobin molecule. On this chain, ____ is substituted for ____ at the sixth position of the chain. a. alpha, glutamic acid (Glu), valine (Val) b. beta, valine (Val), glutamine (Gln) c. alpha, aspartic acid (Asp), Alanine (Ala) d. beta, valine (Val), glutamic acid (Glu) True or False If parent '1' has type A hemoglobin (genotype: A/A) and parent '2' has sickle cell trait (genotype: A/S) the probability of the offspring receiving sickle cell trait is 25%. a.True b.False Alterations in oncogenes, tumor-suppressor genes and microRNA genes can result in? a. tumor reduction b. cancer formation c. neither a or b The gene important in regulation of the cell cycle and also functions as a tumor suppressor is.. a. p24 b. p53 c. p63 d. none of the above D B B B 57 Hematology PPT Flashcards Unit 1 Tumor protein p53 does many things to help our cells repair themselves. Which of the following is incorrect? a. activate the repair of DNA when damaged. b. initiate apoptosis if the DNA is damaged beyond repair. c. prevents the division of cells with mutated or damaged DNA. d. None of the above are incorrect. This list of analytical assays are of what type tests. Polymerase chain reaction (PCR) Ligase chain reaction nucleic acid amplification (LCR) Branched DNA (bDNA) amplification Probe-hybridization assays Integrated PCR and probe-hybridization assays Microarrays A. Chemistry B. Immunological C. Molecular Technique D. Serological The term for the low level of disease, such as, leukemic cells, in a patient who appears to be in a state of clinical remission is. A. Minimal disease state B. Minimal residual disease C. Minimal reduced disease D. Residual disease minimum What does heating the DNA in accomplish in Polymerase chain reaction (PCR) A. Denatures it so it is destroyed. B. To separate the strands of DNA C. Recombine the pieces of DNA D. There isn't a heating stage in Polymerase chain reaction (PCR) True or False The stages of PCR are generally: - Target DNA is first melted using heat. - added primers bind to specific sequences within the target DNA as it cools. - New DNA strands are amplified - This is repeated over many cycles to create a surplus of target DNA - These copies are detected using electrophoresis and staining. a.True D C B B 58 Hematology PPT Flashcards Unit 1 b.False What is a depiction of Polymerase Chain Reaction? Polymerase Chain Reaction continued What are three important application of PCR? What is considered to be the “Gold Standard” method to which other molecular methods are compared? What hybridization methods are used for the detection of disorder in which the DNA sequence of the mutated region has been identified (sickle cell) This hybridization method is used to detect singlebase mutations using allele-specific oligonucleotides (ASOs) Unlike other assays, the dot blot does not require which two parts of the procedure? What are the basic steps of the procedure? 1) Amplification of DNA 2) Identification of a target sequence Synthesis of a labeled antisense probe 9) DNA Sequencing 10) Dot blot and reverse dot blot 11) Dot Blot 1) Enzyme digestion 12) Electrophoretic separation of DNA fragments 1) Labeled oligonucleotide probes of 15-19 base pairs are added. 59 Hematology PPT Flashcards Unit 1 • What is a Reverse Dot Blot? How is the Reverse Dot Blot different? DNA is amplified in the region of the known mutations, denatured and applied to areas of membrane or filter. 3) Variation of Dot Blot procedure 4) The ASO probes are bound to a filter and denatured DNA from the patient is added to the immobilized ASO. Hybridization occurs when base sequences are 100% complementary to the probe What is an example of a southern blot? This procedure is used for analysis of the proximal product of gene expression, mRNA. Cloned DNA probes can determine whether a given gene is expressed and, of so, how vigorously. This is a tissue-based molecular diagnostic assay. Common in situ hybridization (ISH), including fluorescent ISH (FISH), probes are used in the diagnosis of hematological malignancies in clouding CMLA, AML, Burkitt lymphoma and other lymphomas. This gene expression profiling uses _____ analysis. A surface (in this example, a glass microscope slide) contains thousands of spots. Each spot contains a large number of DNA fragments. For each spot, the DNA fragments are derived from one specific gene. Clinical applications include hematopathology diagnosis and monitoring. The distinct advantages of molecular testing include the following: -Faster turn around time -Smaller required sample volumes Northern Blot Blotting Protocol In Situ Hybridization Microarrays Hematopathology 60 Hematology PPT Flashcards Unit 1 -Increased specificity and sensitivity This type of molecular technique monitors patient following bone marrow transplants, discovers and early relapses in patients treated for a hematological malignancy and detects minimal residual disease in hematological malignancies. Important in diagnostic hematopathology as indicator of clonality and as aids in determining the cellular lineage of a particular malignant proliferation. This categorization is aided by the use of cluster designation (CD) for specific lineages of cells. What is Hematopoiesis? What consists of the hematopoietic system? What are the three types of human stem cells? Which type of human stem cell is present in the first few hours after an ovum is fertilized? Which type of human stem cell is the most versatile type? Which type of human stem cell can develop into any human cell type? Which type of stem cell can develop into a fetus? Which type of human stem cell is present several days after fertilization? Which type of hum stem cell can develop into any cell type with the exception of developing into a fetus? Which type of human stem cell is derived from pluripotent stem cells? Which type of human stem cell can be found in adults but are limited to specific types of cells to form tissues? Below are images depicting a (normal/abnormal) bone marrow biopsy. Molecular techniques provided my Hematopathology Gene Rearrangement Studies Immunophenotyping categorization The process of blood cell production, differentiation, and development. Bone Marrow, Liver, Spleen, Lymph Nodes, and Thymus Totipotential, Pluripotential and Multipotential stem cells. Totipotential stem cell Totipotential stem cell Totipotential stem cell Totipotential stem cell Pluripotential stem cell Pluripotential stem cell Multipotential stem cell Multipotential stem cell Normal 61 Hematology PPT Flashcards Unit 1 Below is an image depicting a bone marros biopsy of (normal/abnormal) cellularity Normal Name the type of WBC’s labeled A. Lymphocyte B. Basophil C.Eosinophil D. Segmented neutrophil E. Band form neutrophil 62 Hematology PPT Flashcards Unit 1 Figure (A) is an image depicting a child with red bone marrow. Figure (B) is an image depicting an adult. What major changes happen to the bone marrow as a child develops into an adult? (A) (B) Using the Figure below, describe the size of the HSC population over a lifetime. (Only use once: Increase, Decrease, or remains the same) (a) __________ (b) __________ (c) __________ In an adult, yellow marrow replaces red marrow. Red marrow activity occurs in the central portion of the skeleton (a) Decrease (b) Remains the same (c) Increase 63 Hematology PPT Flashcards Unit 1 Hematopoietic cells can be divided into how many phases? What is the Primitive, multipotential cells? What are Intermediate cells? What are Mature cells? Where does erythropoiesis occur? What is granulopoiesis? Granulopoiesis can be recognized as what? Where does Lymphopoiesis take place? Where does Megakaryopoiesis take place? What are two cells found in the bone marrow? What are Marrow stromal cells? What are Mast cells? What is a macrophage? three phases according to cell maturity The most immature group capable of self-renewal and differentiation into all blood cell lines This group consists of committed progenitor cells destined to develop into distinct cell lines. The most developed group with specific functions in distinct anatomical sites called erythropoietic islands, specialized niches in which erythroid precursors proliferate, differentiate, and enucleate Myeloid cells account for 23% to 85% of the nucleated cells in normal bone marrow a maturational unit. in lymphoid follicles. adjacent to the sinus endothelium Mast cells and marrow stromal cells The meshwork of stromal cells is composed of reticulum cells, histiocytes, adipose cells, and endothelial cells Tissue mast cells, a connective tissue cell of mesenchymal origin, are normally observed in bone marrow It is also called reticulum cell or histiocyte, appear as large cell in the 64 Hematology PPT Flashcards Unit 1 What are bone cells called? What are interleukins? What do interleukins do? How to describe the function of interleukins? What are the roles of interleukins? How many types and function of interleukins in the immune system? What are the three types of hematopoietic growth factors? What is an examination of maturing blood cells? What can be guided by a variety of systematic features? What are the two importatant charateristics to observe initially in caell identification? What is the important feature of the bone marrow. They are called Osteoblasts that are bone matrix–synthesizing cells that resemble plasma cells and are usually observed in groups. Protein molecules that work in conjunction with hematopoietic growth factors to stimulate proliferation and differentiation of specific cell lines Interleukins are cytokines that act independently or in conjunction with other interleukins to encourage hematopoietic growth. Interleukins are cell signaling molecules and a part of the cytokine super family of signaling molecules The interleukins were first described as signals for communication between Interleukins are basically the method of immune cross talk and communication. Interleukins are the primary messengers and directors of the immune system. There are currently 35 well-known interleukins; however, there are many more to be found and characterized. Hematopoietic growth factor is encoded by a single gene - G-CSF and GM-CSF predominantly affect myeloid cells -IL-7 stimulates T and B lymphocytes -IL-12 targets natural killer cells It is a comprehensive examination of bone marrow involves examination of both bone marrow smears and histological tissue sections. The identification and stage of maturation of stained blood cells can be guided by a variety of systematic features. • Overall cell size Nuclear-cytoplasmic ratio • Nuclear characteristics 65 Hematology PPT Flashcards Unit 1 nucleus of the cell? What are the nuclear characteristics of the Chromatin pattern? What are the different nuclear shapes of the cell? play an important role in cell identification. Important features of the nucleus include the following: • Chromatin pattern • Nuclear shape 8. The presence of nucleoli • Chromatin patterns • Lymphocytes exhibit a smooth or homogeneous pattern of chromatin throughout development until the mature stage, when clumped heterochromatin is more obvious. • Granulocytes progress from having a fine to a highly clumped pattern. • Monocytes have a lacy pattern, which becomes finer as the cell matures. • Erythrocytes continue to develop a more clumped pattern as maturation progresses, until the extremely dense (pyknotic) nucleus is lost (extruded) from the mature cell. • Nuclear shape • Lymphocytes usually continue to have a round or oval nucleus. Some cells may have a small cleft in the nucleus. • Monocytes have a kidney bean–shaped nucleus, but folded or horseshoe shapes are common. 11. Mature neutrophils, eosinophils, and basophils have segmented 66 Hematology PPT Flashcards Unit 1 How does the pressence or absense of nucleoli is important in the identification in the cell? • What are the nuclear characteristics of the cell? 5. How can we identify Cytoplasmic Characteristics? nuclei attached to one another by fine filaments. The number of distinctive lobes ranges from two to five depending on the cell type. • Presence of nucleoli • The presence or absence of nucleoli is important in the identification of cells. • The three cell lines of erythrocytes, leukocytes, and megakaryocytes all have nucleoli in the earliest cell stages. As cells mature, nucleoli are usually not visible. These changes in the appearance of the nucleoli are related to the rate of synthesis of ribosomal RNA. • Lymphoblasts have one or two nucleoli. • Myeloblasts have one to five nucleoli. • Monoblasts usually have one or two nucleoli but occasionally may have three or four. • Erythroblasts may not have any nucleoli or may have up to two nucleoli that may stain darker than in other types of blast cells. 4. Megakaryoblasts typically have one to five nucleoli. • Staining color and intensity • Granulation • Shape • Quantity of cytoplasm • Vacuolization 6. Inclusion bodies 67 Hematology PPT Flashcards Unit 1 68