Chapter 20 - Martini
advertisement
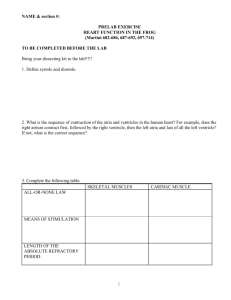
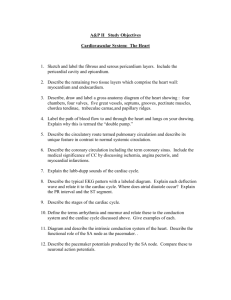
The Heart Chapter 20 Function of the Heart • Pumping the red stuff Anatomy of the Heart • Location – mediastinum, slightly to the left of center • Size – about that of your fist • Mass – 250 – 300 g Organization of the Cardiovascular System Location Tissues of the Heart Coverings of the Heart: Anatomy • Pericardium – a double-walled sac around the heart composed of: – A superficial fibrous pericardium – A deep two-layer serous pericardium • The parietal layer lines the internal surface of the fibrous pericardium • The visceral layer or epicardium lines the surface of the heart • They are separated by the fluid-filled pericardial cavity Coverings of the Heart: Physiology • The pericardium: – Protects and anchors the heart – Prevents overfilling of the heart with blood – Allows for the heart to work in a relatively friction-free environment Serous pericardium General Anatomy • Epicardium – visceral layer of the serous pericardium • Myocardium – cardiac muscle layer forming the bulk of the heart • Fibrous skeleton of the heart – crisscrossing, interlacing layer of connective tissue • Endocardium – endothelial layer of the inner myocardial surface Heart Wall • Vessels returning blood to the heart include: – Superior and inferior venae cavae – Right and left pulmonary veins • Vessels conveying blood away from the heart include: – Pulmonary trunk, which splits into right and left pulmonary arteries – Ascending aorta (three branches) – brachiocephalic, left common carotid, and subclavian arteries External Heart: Major Vessels of the Heart (Anterior View) • Arteries – right and left coronary (in atrioventricular groove), marginal, circumflex, and anterior interventricular arteries • Veins – small cardiac, anterior cardiac, and great cardiac veins External Heart: Vessels that Supply/Drain the Heart (Anterior View) Surface features of the heart Cardiac Muscle Cells Figure 20–5 • Vessels returning blood to the heart include: – Right and left pulmonary veins – Superior and inferior venae cavae • Vessels conveying blood away from the heart include: – Aorta – Right and left pulmonary arteries External Heart: Major Vessels of the Heart (Posterior View) Posterior view Atria of the Heart • Atria are the receiving chambers of the heart • Each atrium has a protruding auricle • Pectinate muscles mark atrial walls • Blood enters right atria from superior and inferior venae cavae and coronary sinus • Blood enters left atria from pulmonary veins Deep in your heart of hearts… Ventricles of the Heart • Ventricles are the discharging chambers of the heart • Papillary muscles and trabeculae carneae muscles mark ventricular walls • Right ventricle pumps blood into the pulmonary trunk • Left ventricle pumps blood into the aorta Note the differences in wall thickness • Heart valves ensure unidirectional blood flow through the heart • Atrioventricular (AV) valves lie between the atria and the ventricles • AV valves prevent backflow into the atria when ventricles contract • Chordae tendineae anchor AV valves to papillary muscles Heart Valves Heart Valves • Aortic semilunar valve lies between the left ventricle and the aorta • Pulmonary semilunar valve lies between the right ventricle and pulmonary trunk • Semilunar valves prevent backflow of blood into the ventricles The heart valves Function of the bicuspid valve Valve functions Heart Sounds Where to go to listen to heart sounds Some heart valve disorders • Stenosis (narrowing) – the inability of a valve to open fully • Insufficiency (incompetence) – failure of the valve to prevent back flow or close properly – Mitral valve prolapse – one or both of the flaps blows back into the atrium during systole (contraction) of the ventricle allowing backflow into the atrium. – The aortic semilunar valves can also suffer from stenosis or insufficiency, allowing backflow into the ventricle. • Right atrium tricuspid valve right ventricle • Right ventricle pulmonary semilunar valve pulmonary arteries lungs • Lungs pulmonary veins left atrium • Left atrium bicuspid valve left ventricle • Left ventricle aortic semilunar valve aorta • Aorta systemic circulation Pathway of Blood Through the Heart and Lungs Systemic & pulmonary circuits Blood flow Coronary Circulation • Coronary circulation is the functional blood supply to the heart muscle itself • Collateral routes ensure blood delivery to heart even if major vessels are occluded Coronary Circulation (arterial) Coronary Circulation (venous) Cardiac histology & physiology • Cardiac muscle is made of short, branched fibers • Striated • Uninucleate • There is now some evidence that it has limited mitotic capability (it is likely that regeneration is from migration of stem cells from the blood) • 99% are contractile • 1% are “autorhythmic” or “pacemaker” cells Cardiac Muscle Tissue Cardiac Muscle Cells • Intercalated discs: – – – – – interconnect cardiac muscle cells secured by desmosomes linked by gap junctions convey force of contraction propagate action potentials Characteristics of Cardiac Muscle Cells 1. 2. 3. 4. Small size Single, central nucleus Branching interconnections between cells Intercalated discs Cardiac Cells vs. Skeletal Fibers Table 20-1 The intrinsic conduction system • Sinoatrial node: the primary pacemaker – has an intrinsic firing rate of about 100 bpm but kept at 60 – 80 by parasympathetic tone • Generates pacemaker potentials from leakage of Ca++ • Depolarization spreads via gap junctions in intercalated disks • Rate can be adjusted by ANS Intrinsic conduction system • Signals from SA node travel to the Atrioventricular Node via the internodal pathway • The AV node has its own intrinsic firing rate of 40 – 60 bpm. In absence of SA node function it can establish a “junctional rhythm” that keeps the ventricles working The conducting pathways • The signal is delayed about 0.1 s and then transmitted down the … • Bundle of His or AV bundle and the left & right bundle branches to the apex • And from there the depolarization is distributed by the Purkinje fibers Fig. 20.10a Contraction of cardiac muscle fibers and the cardiac cycle The Electrocardiogram Figure 20–14b NSR: Normal Sinus Rhythm Prolonged contraction of cardiac muscle Features of an ECG • P wave: – atria depolarize • QRS complex: – ventricles depolarize • T wave: – ventricles repolarize Resting Potential • Of a ventricular cell: –about —90 mV • Of an atrial cell: –about —80 mV 3 Steps of Cardiac Action Potential 1.Rapid depolarization: » voltage-regulated sodium channels (fast channels) open 3 Steps of Cardiac Action Potential 2. As sodium channels close: – voltage-regulated calcium channels (slow channels) open + – balance Na ions pumped out – hold membrane at 0 mV plateau 3 Steps of Cardiac Action Potential 3. Repolarization: – plateau continues – slow calcium channels close – slow potassium channels open – rapid repolarization restores resting potential The Refractory Periods • Absolute refractory period: – long – cardiac muscle cells cannot respond • Relative refractory period: – short – response depends on degree of stimulus Timing of Refractory Periods • Length of cardiac action potential in ventricular cell: – 250–300 msecs • 30 times longer than skeletal muscle fiber • long refractory period prevents summation and tetany Electrical Activity and the Cardiac Cycle Calcium and Contraction • Contraction of a cardiac muscle cell is produced by an increase in calcium ion concentration around myofibrils 2 Steps of Calcium Ion Concentration 1. 20% of calcium ions required for a contraction: – calcium ions enter cell membrane during plateau phase 2 Steps of Calcium Ion Concentration 2. Arrival of extracellular Ca2+: – triggers release of calcium ion reserves from sarcoplasmic reticulum Intracellular and Extracellular Calcium • As slow calcium channels close: – intracellular Ca2+ is absorbed by the SR – or pumped out of cell • Cardiac muscle tissue: – very sensitive to extracellular Ca2+ concentrations • CO is the amount of blood pumped by each ventricle in one minute • CO is the product of heart rate (HR) and stroke volume (SV) • HR is the number of heart beats per minute • SV is the amount of blood pumped out by a ventricle with each beat • Cardiac reserve is the difference between resting and maximal CO The Cardiac Cycle Phases of the Cardiac Cycle Figure 20–16 Cardiac output • CO (ml/min) = HR (75 beats/min) x SV (70 ml/beat) • CO = 5250 ml/min (5.25 L/min) Cardiac output • SV = end diastolic volume (EDV) minus end systolic volume (ESV) • EDV = amount of blood collected in a ventricle during diastole • ESV = amount of blood remaining in a ventricle after contraction Pressure and Volume in the Cardiac Cycle Figure 20–17 Factors Affecting Stroke Volume • Preload – amount ventricles are stretched by contained blood • Contractility – cardiac cell contractile force due to factors other than EDV • Afterload – back pressure exerted by blood in the large arteries leaving the heart • Changes in EDV or ESV Factors Affecting Stroke Volume Figure 20–23 (Navigator) Frank-Starling Law of the Heart • Preload, or degree of stretch, of cardiac muscle cells before they contract is the critical factor controlling stroke volume • Slow heartbeat and exercise increase venous return to the heart, increasing SV • Blood loss and extremely rapid heartbeat decrease SV Extrinsic Factors Influencing Stroke Volume • Contractility is the increase in contractile strength, independent of stretch and EDV • Increase in contractility comes from: – Increased sympathetic stimuli – Certain hormones – Ca2+ and some drugs Factors Affecting Heart Rate and Stroke Volume Extrinsic Factors Influencing Stroke Volume • Agents/factors that decrease contractility include: – Acidosis – Increased extracellular K+ – Calcium channel blockers Contractility and Norepinephrine • Sympathetic stimulation releases norepinephrin e and initiates a cyclic AMP secondmessenger system Figure 18.22 Regulation of Heart Rate • Positive chronotropic factors increase heart rate • Negative chronotropic factors decrease heart rate • Sympathetic nervous system (SNS) stimulation is activated by stress, anxiety, excitement, or exercise • Parasympathetic nervous system (PNS) stimulation is mediated by acetylcholine and opposes the SNS • PNS dominates the autonomic stimulation, slowing heart rate and causing vagal tone Regulation of Heart Rate: Autonomic Nervous System Autonomic Innervation Autonomic Pacemaker Regulation Autonomic Pacemaker Regulation (1 of 3) • Sympathetic and parasympathetic stimulation: – greatest at SA node (heart rate) • Membrane potential of pacemaker cells: – lower than other cardiac cells Autonomic Pacemaker Regulation (2 of 3) • Rate of spontaneous depolarization depends on: – resting membrane potential – rate of depolarization Autonomic Pacemaker Regulation (3 of 3) • ACh (parasympathetic stimulation): – slows the heart • NE (sympathetic stimulation): – speeds the heart Atrial (Bainbridge) Reflex • Atrial (Bainbridge) reflex – a sympathetic reflex initiated by increased blood in the atria – Causes stimulation of the SA node – Stimulates baroreceptors in the atria, causing increased SNS stimulation CNS and ANS controls of Cardiac output Chemical Regulation of the Heart • The hormones epinephrine and thyroxine increase heart rate • Intra- and extracellular ion concentrations must be maintained for normal heart function PLAY InterActive Physiology®: Cardiovascular System: Cardiac Output Factors Involved in Regulation of Cardiac Output How the heart starts Examples of Congenital Heart Defects Congestive Heart Failure (CHF) • Congestive heart failure (CHF) is caused by: – – – – Coronary atherosclerosis Persistent high blood pressure Multiple myocardial infarcts Dilated cardiomyopathy (DCM) Arteriosclerosis Fig. 20.20 Age-Related Changes Affecting the Heart • • • • Sclerosis and thickening of valve flaps Decline in cardiac reserve Fibrosis of cardiac muscle Atherosclerosis