presentation ( format)
advertisement

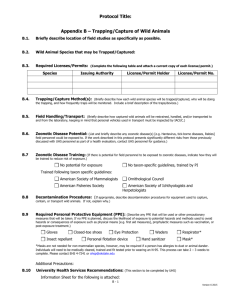
Meaningful Use: Relevance in College Health American College Health Association May 30th 2013 UHS Collaborators • Maria Campanile MD Primary Care Clinic, Chair of Committee on Clinical Informatics • Arnie Jennerman CPA, MBA Director of Administrative Services • Danielle Oakley PhD Director of Counseling and Consultation Services • Theresa Regge MS Information Technology Services Manager • Nancy Ranum MS, NP, RN-BC Informatics Nurse Specialist, NP – Clinical Informatics Manager • Shelia Zweifel RHIT HIM and Privacy Manager AAAHC Coordinator Learning Objectives • Use and Importance of Benchmarking • Meaningful Use Background and Applicability • What we did at UHS at UW Madison • Results of the Project • Usefulness and Recommendations • Questions and Answers Benchmarking Standard • Benchmarking: a systematic comparison of products, services or work processes of similar organizations, departments or practitioners to identify best practices known to date for the purpose of continuous quality improvement. External benchmarking compares performance between different organizations. Internal benchmarking compares performance within an organization, such as by physician or department, or over time. • Performance measure: a clearly defined statement or question describing information to be collected for purposes of improving processes and outcomes of care. • From the Accreditation Association for Ambulatory Health Care (AAAHC) Accreditation Handbook for Ambulatory Health Care: The organization's quality improvement program must include participation in external performance benchmarking activities that will allow for comparison of key performance measures with other similar organizations or with recognized best practices of national or professional targets or goals [Standard 5.II.C]. Benchmarking at UHS • Essential Element of Quality Improvement Program • Process overseen by QMIC Quality Management Improvement Committee • Challenge Finding Appropriate Benchmarks • Challenge Finding External Benchmarks • Incorporating Benchmarking into Daily Activity Systems Challenge Why UHS Considered Meaningful Use • Not a Requirement for UHS • No Reimbursement Incentive • Went to Paperless EMR June 2008 • EMR a Journey with no Destination are we there yet? • Looking for an External Benchmark • Guide our EMR Strategic Planning • Possible Vendor Leverage Review Of Our Process • What is Meaningful Use? • UHS approach to understanding MU • MU alignment in Clinical Services • Reconciling MU criteria with existing Health Information Management requirements • Implications for Information Technology Services other administrative functions • Relevance in Counseling, Psychiatry and Behavioral Health • The larger conversation: conflicts and dilemmas What is Meaningful Use? What is Meaningful Use? Drivers for Incentivizing Health Information Technology • Unprecedented healthcare spending has not resulted in improved quality especially in Medicare and Medicaid populations U.S. Health Care Quality: Stuck in Neutral, Slowdown has Implications for Reform; NCQA Press Release, October 22, 2009 • Quality of healthcare in US ranks low in comparison to other developed countries K. Davis, C. Schoen, and K.Stremikis, Mirror, Mirror on the Wall: How the Performance of the U.S. Health Care System Compares Internationally: 2010 Update (New York: The Commonwealth Fund, June 2010) • Dovetails with other healthcare reform initiatives • e.g. Healthcare Affordability Act, Accountable Care Organizations (ACOs) and Medicare Shared Savings Program Health System In Crisis • Total Healthcare spending 17.9% of GDP in 2011 • Currently at $3 Trillion per year • Expected to grow to 20% of GDP by 2021 • Spend the most of any nation per capita • Spending is 2 an 1/2 times the OECD average per person • According to WHO we rank 50th in life expectance at birth • Growing faster than the economy, a competitiveness issue Origin of “Meaningful Use” ARRA: American Recovery and Reinvestment Act, 2009; the “Stimulus Bill” HITECH: Health Information Technology for Economic and Clinical Health Act Title XIII of ARRA ONC: Office of the National Coordinator for health information technology CMS: Centers for Medicare and Medicaid Services • ONC and CMS worked closely to establish the rules • Multiple committees, sub committees; members included clinicians, IT leaders, public policy experts; public meetings – webcasts, online comments Goals of HITECH • Improve quality, safety and efficiency • Reduce health disparities • Engage patients and families in their health care • Promote public and population health • Improve care coordination • Promote the privacy and security of EHRs HITECH Incentives Federal program to provide financial incentive to providers and hospitals for the adoption AND demonstrated “meaningful use” of certified health information technology (HIT) • $27 Billion over 10 years • Up to $44,000 (Medicare) and $63,750 (Medicaid) per clinician • Eventually, 2015, penalties (cuts in Medicare reimbursement for not adopting) • Numerous deadlines and cutoffs Components of HITECH • Meaningful Use “Rule” – guidelines and requirements for achieving Stage 1 MU • EHR standards and certification criteria that support MU (Certification Commission for Health Information Technology - CCHIT) • New protections to strengthen and expand privacy, security and enforcement of HIPAA • Temporary certification program for HIT Systems MU Stage One Measures Core Measures • 15 required objectives for eligible professionals (EP), 14 for eligible hospitals (EH) and critical access hospitals (CAH) Menu Measures • EPs and hospitals must also implement 5 of 10 additional criteria (their choice) Quality Reporting-Clinical Quality Measures • For stage 1, EPs must report on 3 core measures: blood-pressure level, tobacco status, adult weight screening and follow-up • EPs also need to report on 3 additional measures from a list of 38 metrics ready for incorporation into EHRs • Hospitals must report on 15 required quality metrics Stage 1: 15 Core Measures for EPs 1. CPOE (ComputerizedProvider Order Entry) for medication orders 2. Implement drug-drug and drug-allergy interaction checks 3. Generate and transmit permissible prescriptions electronically (eRx) 4. Record demographics: preferred language, gender, race ethnicity, DOB 5. Maintain up to date electronic problem list of current/active diagnosis Stage 1: 15 Core Measures cont. 6. Maintain active medication list 7. Maintain active medication allergy list 8. Record and chart changes in vital signs including BMI and growth charts for age 2-20 yrs. 9. Record smoking status for patients 13 yrs or older 10. Implement one clinical decision support rule relevant to specialty or of high clinical priority along with the ability to track compliance 11. Report ambulatory clinical quality measures to CMS or State Stage 1: 15 Core Measures cont. 12. Provide patients with electronic copy of their health information upon request (test results, problem list, medication and allergy lists) 13. Provide clinical summaries for each office visit 14. Capability to exchange key clinical information among providers of care and patientauthorized entities electronically 15. Protect electronic health information created or maintained by the certified EHR technology through the implementation of appropriate technical capabilities Stage 1: Menu Set for EPs 1. Implement drug-formulary checks 2. Incorporate clinical lab-test results into certified EHR technology as structured data 3. Generate lists of patients by specific conditions to use for quality improvement, reduction of disparities, research or outreach 4. Send reminders for preventive/follow-up care 5. Provide patients with timely electronic access to their health information (lab results, problem list, medication/allergy lists) Stage 1: Menu Set Continued 6. Use certified EHR technology to identify and provide patient-specific educational resources 7. Medication reconciliation as relevant 8. Provide summary of care record for transitions of care/referral 9. Capability to submit electronic data to immunization registries/systems 10. Capability to provide electronic syndromic surveillance data to public health Attestation • Incremental approach – 3 stages • Stage 1 (2011-12) - baseline for electronic data capture and information sharing; very specific numerator and denominator parameters • Stage 2 rules not yet finalized by ONC, delayed to 2014 • Stage 3 – Proposal to support New Care Models now 2016 at the earliest, industry push back • • • • Over 291,325 providers received incentives $5.7 B $8.7 Billion in incentives to 3,880 hospitals Demanding data-driven process Will influence industry benchmarks and consumer expectations Getting Buy-in for MU at UHS Leadership Interest In Benchmarking Point and Click Steering Committee Committee on Clinical Informatics Quality Management and Improvement Committee Process Used in COCI Educated committee on background of MU Blumenthal, D., M.D., M.P.P., and Tavenner, M, R.N., M.H.A. (2010); The “Meaningful Use” Regulation for Electronic Health Records, New England Journal of Medicine; August 5, 2010, pg. 501-504 Evaluated various critiques of MU rules • CHIME-College of Healthcare Information Management Executives • AHIMA-American Health Information Management Association • HIMSS-Health Information Systems Society – distributed this to committee Evaluating MU Criteria Reviewed & rated Core Criteria for importance/relevance to college health • Classified Highly Important, Important, Not Important • Focus on EP Eligible Professionals not Hospital • Focused on finalized Stage 1 rules • Noted that Measures designed to drive $ • Stage 2 discussion provided a “heads-up” of where MU is headed, basically more demanding measures more Participation and integration How UHS Aligns with MU Core Requirements • 1 Medication CPOE • 2 Drug-drug/allergy interaction checks • 3 E-Prescribing, and formulary checks, E-fax migrating to E-Rx • 4 Demographics – yes no field for preferred language • 5 Electronic Problem List meets MU criteria but some issues with functionality e.g. patient entered data • 5, 6 and 7 Medication List, Allergy List, Problem List, but not available to patients via MyUHS portal (not available in our EMR) • 8 Vitals, Not using growth charts How UHS Aligns with MU Core Requirements (continued) • 9 Documentation of smoking status: PnC does not support but UHS has customized risk screening that includes documentation at all visits and embedded health maintenance alerts • 10 Clinical Decision Support • Primary and Secondary Risk assessment for tobacco use, alcohol use, depression • Asthma template includes prompts for influenza and pneumonia vaccine • “Disease” Management programs for Employee Health and Occupational Medicine populations • 11 Immunization Registry – Separate Interface WIR • Challenge in college health is that population is mobile and comes from all over the world How UHS Aligns with MU Core Requirements (continued) • 12 Patient portal for messaging, access to diagnostic reports, Problem List, Medication and Allergy Lists etc. Electronic Problem List meets MU criteria but some issues with functionality e.g. patient entered data one time • 13 Visit Summary – EMR has capability but not using currently, cannot customize format/content • 14 Laboratory, Radiology Interfaces, referral not electronic results via EPIC Carelink • 15 Data security for PHI fully compliant How UHS Aligns with MU Menu Set Requirements • 1 Drug formulary check • 2 Lab results as structured data • 3 Generate patient lists for quality improvement • 4 Reminders for preventive/follow-up care • 5 Visit summary • 6 Education: mechanisms in place using customized template triggers and mechanisms for sending links via secure message • 7 Medication reconciliation few referrals in where relevant How UHS aligns with Menu Set Requirements • 8 Ability to receive and send patient health records with providers and ERs in Madison and beyond Many gaps from Health Information Exchange (HIE)-IT perspective • 9 Submission to immunization registries and systems custom interface • 10 Ability to submit electronic syndromic surveillance data to public health agencies not automatic Observations of UHS MU Evaluation • Overall pretty good compliance with Core Measures and Menu Set, only need 5 of 10 • Followed multidisciplinary process, important dialogue • Focused on gaps between our processes and MU criteria • Evaluated capabilities of our EHR • Realization this will impact community standards/expectations and benchmarks • Provided direction for future IT and Quality initiatives • Implementing an EHR a journey not a destination Existing Standards, Regulations and Laws How will MU impact accrediting bodies? • JCAHO: Joint Commission on Accreditation of Healthcare Organizations • AAAHC: Accreditation Association for Ambulatory Health Care • NCQA: National Committee for Quality Assurance State and Federal Law? • HIPAA, FERPA Health Information Management Processes • Recording • Storing • Ordering • Retrieving • Releasing • Modifying Entries Policy and Procedures Organizations have existing policies, procedures and workflows • Review and align with Meaningful Use Chart audits and compliance • Drug allergy reviews • Problem list audits • Medication audits • Appropriate Access/Confidentiality • Templates have “hard stops” Privacy and Security of PHI • Existing standards, rules, law • Ensure integrity of information not been altered as it moves around • Accounting of disclosures and access • Current state and federal laws • Patient /consumer anxiety Request for Records • Existing state and federal laws • Possible conflicts with HIPAA, FERPA • Visit summary making it useful? • “Human readable format” • Consumer health literacy HIE: Health Information Exchange • Need for unique patient identifier • Electronic transmittal of records to other providers • EMR versus EHR Interface vs Integrate • Patients have ability to opt out and apply restrictions limit usefulness • Conflicts with state or federal laws • WISHIN Implications for Information Technology Services Getting disparate systems to communicate effectively, efficiently and legally • Evaluate systems capability “as is” and determine what future requirements will be • Work with EHR vendor • CHITT certified – changes embedded in future releases • Implications for upgrades • Implementation and upgrade costs – hardware, software, IT staff, downtime, training Relevance in Counseling, Psychiatry, and Behavioral Health Implications of the exclusion of Mental Health providers from the HITECH act. • No access to the incentive funding • Excludes some of the most underserved groups • Barrier to coordinated care Relevance in Counseling, Psychiatry and Behavioral Health • Status of the Health Information Technology Extension for Behavioral Health Services Act of 2010 (HR5040) • To amend the Public Health Service Act and the Social Security Act to extend health information technology assistance eligibility to behavioral health, mental health, and substance abuse professionals and facilities, and for other purposes. The bill never became law Relevance in Counseling, Psychiatry, and Behavioral Health Mental Health considerations in the MU conversation at UHS • Integrated model Behavioral Health mental health issues as “brain diseases” • Medical vs. mental health summary privacy issues • What goes on Problem List? Presentation Objectives • Use and Importance of Benchmarking • Meaningful Use Background and Applicability • What we did at UHS at UW Madison • Results of the Project • Usefulness and Recommendations Meaningful Use: Conflicts and Dilemmas • Lack of universal patient ID and issues with SSN • Who “owns” health information; Shared lifetime EHR/PHR • Transparency and how to assure that shared information is “meaningful/understandable” to the range of users/consumers of the health information • “Technological divide” – disparity of electronic access and literacy • Vendor co-opting standards proprietary use of HL7 CommonWell announcement at HIMSS Meaningful Use: Conflicts and Dilemmas, cont. • EMR versus EHR, Interface versus Interoperate • Role of cloud technology • Second generation EMR versus third generation “we have an app for that” • Clinical Quality measures – aligning clinical guidelines, evidenced based medicine and local quality initiatives with MU…. or visa versa? • Constraints of EMR products, EMR certification, CCHIT…. Instances of “the tail wagging the dog”? • ROI – What if it does not improve outcomes or it costs more than it saves? • Currently heavy industry lobbying against penalties “regulatory capture” • Political Uncertainty….. Thank You!!! Questions??? Web Links • Centers for Medicare and Medicaid Services http://www.cms.gov • http://www.cms.gov/EHRIncentivePrograms • HIMSS Meaningful Use information www.himss.org/ASP/topicsmeaningfuluse.asp • Federal Register, see pages 44370-443780 for summary www.gpo.gov/fdsys/pkg/FR-2010-07-28/pdf/2010-17207.pdf