Preliminary findings of ACT workshops for clients and caregivers in
ACT for Recovery:
Preliminary findings of ACT workshops for clients and caregivers in community psychosis services.
L.Butler, E.O’Donoghue, E.Morris, J.Oliver, L.Johns & S.Jolley, South London and Maudsley NHS Foundation Trust.
Introduction & Aims
ACT has shown to be a promising intervention for helping people with psychosis. RCTs have demonstrated lower rehospitalisation rates (Bach
& Hayes, 2002) and advantages in mood, social impairment and overall distress associated with symptoms (Gaudiano & Hayes, 2006). ACT fits in particularly well with the recovery principles of finding and maintaining hope, encouraging self-management, contacting selfawareness and encouraging the development of a positive self-identity.
ACT workshops trialled recently in London & Scotland (referenced in
McArthur et al., 2013) have demonstrated good results, but no randomised controlled design has as yet been conducted with this population.
Informal caregivers play a key role in client care and recovery. The negative impact of the caregiving role on carer physical and mental well-being has been well documented (Awad & Vorgunati, 2008) with as many as 80% of caregivers reporting feelings of distress and burden
(Kuipers & Bebbington, 2005). Intervening with caregivers to reduce distress and improve wellbeing, as well as being helpful in its own right, should also promote recovery for clients.
This project aims to evaluate the effectiveness of the ACT workshops as a means of improving self-reported wellbeing for both clients with psychosis and caregivers of people with psychosis. We also aim to promote recovery and to formally assess the cost-effectiveness of these workshops for psychosis
Design and Method
This is the first Randomised Controlled Trial (RCT) of ACT workshops for people with psychosis and their caregivers.
Recruitment Target: 48 clients and 48 caregivers.
Participants are randomised to either an ACT workshop immediately, or to a waitlist control group. Measures are completed at four timepoints
– baseline, 4 weeks (post therapy), 12 weeks (post booster session) and
36 weeks (6 month follow-up).
Measures
• Time Budget (Jolley et al., 2005; 2006).
• Interference Measure (adapted from Sheehan, 1983).
• Valuing Questionnaire (Smout et al., 2011).
• Acceptance and Action Questionnaire-II (Bond et al., 2011).
• Warwick-Edinburgh Wellbeing Scale (Tennant et al., 2007).
• Southampton Mindfulness Questionnaire (Chadwick et al., 2008).
• CORE-10 (Clinical Outcomes in Routine Evaluation) Barkham et al.,
2008).
• Qualitative Feedback on groups & Satisfaction Questionnaire.
• Clients also complete: Measure of service use to assess costs, adapted PSYRATS (Haddock et al., 1999) & Questionnaire about
Process of Recovery (Neil et al., 2009).
Workshop Protocol
The ‘ACT for Recovery Manual’ (O’Donoghue et al., 2012) is the second edition of the ‘ACT for Life’ Protocol (Oliver et al., 2011), with additions following feedback from previous participants. The protocol is the same for client and caregiver workshops.
The ‘ACT for Recovery’ workshops consist of four 2-hour weekly sessions, followed by two 2-hour booster sessions 8 weeks later.
The intervention is based principally on the ‘Passengers on the Bus’ metaphor (Hayes et al., 2009) which is reiterated throughout the four sessions..
Recruitment target allows for 6 participants per workshop.
Each workshop is facilitated by the lead ACT therapist, a mental health staff member and a service user co-facilitator.
Session format:
• Warm-up exercise
• Noticing exercises (mindfulness)
• Defusion exercises
• Discussions of committed action from previous session
• Values-driven goal setting
• Group discussion/activity (including role play/experiential exercises)
• Setting out of session committed actions.
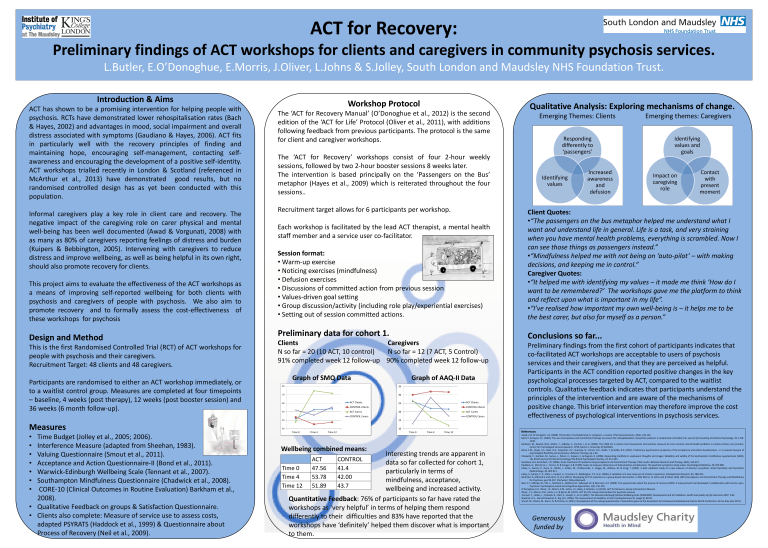
Preliminary data for cohort 1.
Clients Caregivers
N so far = 20 (10 ACT, 10 control) N so far = 12 (7 ACT, 5 Control)
91% completed week 12 follow-up 90% completed week 12 follow-up
Graph of SMQ Data
60
50
40
30
80
70
Time 0 Time 4 Time 12
ACT Clients
CONTROL Clients
ACT Carers
CONTROL Carers
Graph of AAQ-II Data
15
10
25
20
35
30
Time 0 Time 4 Time 12
ACT Clients
CONTROL Clients
ACT Carers
CONTROL Carers
Wellbeing combined means:
ACT CONTROL
Time 0 47.56
41.4
Time 4 53.78
42.00
Time 12 51.89
43.7
Interesting trends are apparent in data so far collected for cohort 1, particularly in terms of mindfulness, acceptance, wellbeing and increased activity.
Quantitative Feedback: 76% of participants so far have rated the
workshops as ‘very helpful’ in terms of helping them respond differently to their difficulties and 83% have reported that the workshops have ‘definitely’ helped them discover what is important to them.
Qualitative Analysis: Exploring mechanisms of change.
Emerging Themes: Clients Emerging themes: Caregivers
Responding differently to
‘passengers’
Identifying values and goals
Identifying values
Increased awareness and defusion
Impact on caregiving role
Contact with present moment
Client Quotes:
• “The passengers on the bus metaphor helped me understand what I want and understand life in general. Life is a task, and very straining when you have mental health problems, everything is scrambled. Now I can see those things as passengers instead.”
• “Mindfulness helped me with not being on ‘auto-pilot’ – with making decisions, and keeping me in control.”
Caregiver Quotes:
• “It helped me with identifying my values – it made me think ‘How do I want to be remembered?’ The workshops gave me the platform to think and reflect upon what is important in my life”.
• “I’ve realised how important my own well-being is – it helps me to be the best carer, but also for myself as a person.”
Conclusions so far...
Preliminary findings from the first cohort of participants indicates that co-facilitated ACT workshops are acceptable to users of psychosis services and their caregivers, and that they are perceived as helpful.
Participants in the ACT condition reported positive changes in the key psychological processes targeted by ACT, compared to the waitlist controls. Qualitative feedback indicates that participants understand the principles of the intervention and are aware of the mechanisms of positive change. This brief intervention may therefore improve the cost effectiveness of psychological interventions in psychosis services.
References
Awad, A.G. & Voruganti, L.N. (2008). The burden of schizophrenia on caregivers: a review. Pharmacoeconomics, 26(2), 149-162.
Bach, P. & Hayes, S.C. (2002). The use of acceptance and commitment therapy to prevent the rehospitalisation of psychotic patients: A randomized controlled trial. Journal of Consulting and Clinical Psychology, 70, 1129-
1139.
Barkham, M., Bewick, B.M., Mullin, T., Gilbody, S., Connell, J. et al. (2008). The CORE-10: A routine short assessment and outcome measure for core common mental health problems in routine primary care practice.
Centre for Psychological Services Research, CPSR, Memo 2, University of Sheffield.
Bond, F.W., Hayes, S.C., Baer, R.A., Carpenter, K.C., Guenole, N., Orcutt, H.K., Waltz, T. & Zettle, R.D. (2011). Preliminary psychometric properties of the Acceptance and Action Questionnaire – II: A revised measure of psychological flexibility and acceptance. Behavior Therapy, pp.1-38.
Chadwick, P., Hember, M., Symes, J., Peters, E., Kuipers, E. & Dagnan, D. (2008). Responding mindfully to unpleasant thoughts and images: Reliability and validity of the Southampton mindfulness questionnaire (SMQ).
The British Journal of Clinical Psychology/The British Psychological Society, 47, 451-455.
Gaudiano, B.A. & Herbert, J.D. (2006). Acute treatment of inpatients using Acceptance and Commitment Therapy: Pilot results. Behavior Research and Therapy, 44(3), 415-437.
Haddock, G., McCarron, J., Tarrier, N. & Farager, E.B. (1999). Scales to measures dimensions of hallucinations and delusions: The psychotic symptoms rating scales. Psychological Medicine, 29, 879-889.
Jolley, S., Garety, P., Dunn, G., White, J., Aitken, M., Challacombe, F., Griggs, M., Wallace, M. & Craig, T. (2005). A pilot validation study of a new measure of activity in psychosis. Social Psychiatry and Psychiatric
Epidemiology, 40, 905-911.
Jolley, S., Garety, P. A., Ellet, L., Kuipers, E., Freeman, D., Bebbington, P.E. et al. (2006). A validation of a new measures of activity in psychosis. Schizophrenia Research, 85, 288-295.
McArthur A, Mitchell G and Johns LC et al (2013). Developing ACT for psychosis as a group-based intervention. In EMJ Morris, LC Johns and JE Oliver (Eds) (2013) Acceptance and Commitment Therapy and Mindfulness for Psychosis, pp.219-237. Chichester: Wiley-Blackwell.
Neil, S.T., Kilbride, M., Pitt, L., Nothard, S., Welford, M., Sellwood, W. & Morrison, A.P. (2009). The questionnaire about the process of recovery (QPR): A measurement tool developed in collaboration with service users.
Psychosis: Psychological, Social and Integrative Approaches, 1(2), 145-155.
O’Donoghue, E.K., Oliver, J.E., Morris, E.M., Johns, L.C, Jolley, S. & Butler, L.E (2013). ACT for Recovery: Group Interventions Manual.
Oliver, J. E., Morris, E.M., Johns, L.C. & Byrne, M. (2011). ACT for Life: Group interventions for psychosis manual.
Tennant, T., Hillier, L., Fishwick, R., Platt, S., Joseph, S., et al. (2007). The Warwick-Edinburgh Mental Wellbeing Scale (WEMWBS): Development and UK Validation. Health and quality of Life Outcomes 2007. 5:63.
Sheehan, D.V., Harnett-Sheehan K., Raj, B.A. (1996). The measurement of disability. Int Clin Psychopharmacol 11 (suppl 3), 89-95.
Smout, M., Davies, M., Burns, N. & Christie, A. (2011). Development of the valuing questionnaire. Presentation given at the Association for Contextual and Behavioral Science World Conference, Parma Italy (July 2011).
Generously funded by