(RDM) Provider Manual - Home Page for MHMRTC
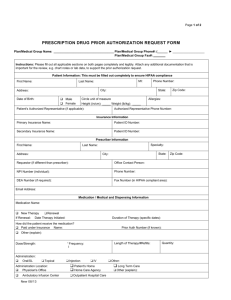
advertisement

Mental Health Mental Retardation of Tarrant County Mental Health Resiliency and disease management clinic Provider Manual SEPTEMBER,2010 Table of Contents INTRODUCTION…………………………………………………………………………….….1 MISSION STATEMENT& VALUES…………………………………………………………..2 ORGANIZATIONAL STRUCTURE………………………….……………………………….3 IMPORTANT POINTS TO REMEMBER………………………………………………….....3 REFERRAL AND AUTHORIZATION PROCESSES…………………………………….….4 SERVICES………………………………………………………..………………….…………...5 DOCUMENTATION .................................................................................................................... 8 CLAIMS & BILLING ................................................................................................................ 15 REPORTING REQUIREMENTS ............................................................................................ 32 MONTHLY REPORT ................................................................................................................ 33 STAFF TRAINING .................................................................................................................... 37 CREDENTIALING AND CLINICAL SUPERVISION ......................................................... 40 MEDICATIONS ......................................................................................................................... 43 LA QUALITY MANAGEMENT/CONTRACT MONITORING ......................................... 44 PROVIDER PROFILE .............................................................................................................. 46 COMPLAINTS ........................................................................................................................... 47 SANCTIONS, APPEALS AND CONTRACT TERMINATION ........................................... 48 REFERENCES ............................................................................................................................ 49 Introduction W elcome to Mental Health Mental Retardation of Tarrant County (MHMRTC). We are pleased to recognize you as a member of our Provider Network and look forward to enjoying a long and mutually satisfying contractual relationship with you. The purpose of this Provider Manual is to educate you about the policies and procedures of MHMRTC. We ask that you read this material carefully and discuss any questions you may have with our Director of Contracts Management/Provider Relations, Kevin McClean, at (817) 569-4456. MHMRTC is staffed by a team of highly dedicated professionals experienced in managed care and the provision of services for persons who are diagnosed with mental illness. MHMRTC is dedicated to providing high quality, innovative, and cost-effective management of mental health services. Our philosophy is propelled by a strong commitment to service excellence supported by management flexibility and accountability. Our on-going objective is to continually refine our system so that we can excel in the delivery of quality services as we balance the best interests of our consumers, providers, and employees. MHMRTC clearly understands that open communication must exist between our service providers and our organization in order for us to be able to provide individuals in our community with the best possible care. We, therefore, invite you to share your perceptions, needs, and suggestions with our Director of Contracts Management/Provider Relations, who will also, from time to time, ask you to respond to surveys to help us identify other opportunities to improve our services and to assess your satisfaction as a member of our provider network. We will do all that we can to support your entry into our system and assure that your continued participation in our network will be beneficial for all concerned. In this Provider Manual, references may be made to consumers, clients, and covered individuals. All of these terms are to be considered interchangeable. Other references that are used interchangeably are MHMRTC and Local Authority (LA), and DSHS and State Authority (SA). 1 Mission Statement & Values Mission Statement of MHMR of Tarrant County: To enhance the mental health and intellectual development of people in our community. Values Each person is respected and valued. Services are developed around the individual needs, values, and opinions of each person served. Families are valued and respected for their critical importance in a person’s support system and are given the opportunity to have an active role in treatment planning and the delivery of services. Success is demonstrated in terms of outcome for each person served. Services enhance dignity through participation and choice. Services encourage and support growth, independence, and integration into the community. Quality services are provided in a safe, ethical, and cost effective manner, and provide the best value to the person served. Programmatic and administrative best practices are recognized and valued. A seamless system of services is realized through the coordination and collaboration of providers in the community. 2 Organizational Structure The organizational structure of MHMRTC includes the Mental Health and Mental Retardation Community Advisory Committees. These two committees are composed of individuals from the community, including consumers, who have a vested interest in assuring that quality services are readily available to our consumers. The committees are empowered to provide input into the planning process that will lead our organization into the future. Both of the committees report to our Board of Trustees. Our Chief Executive Officer is accountable to our Board of Trustees. The Deputy Chief Executive Officer directs the Authority component of our organization and is accountable to our Chief Executive Officer. Chiefs who report directly to the Deputy Chief Executive Officer direct both Mental Health and Mental Retardation Services. There are three Chiefs who oversee the administrative duties of our organization, which includes Information Systems, Finance, and Human Resources and are accountable to our Chief Executive Officer. These areas provide support services to the Authority and to MHMRTC providers. Currently, MHMRTC has providers in the areas of Mental Health Services, Mental Retardation Services, Addiction Services, and Early Childhood Intervention Services. We anticipate continued growth in expanding our service providers from the community. Important Points to Remember Provider’s Responsibilities It is the provider’s responsibility to render services to MHMRTC consumers in accordance with the terms of the contract. The provider is required to render these services to MHMRTC consumers in the same manner, adhering to the same standards, and within the same time availability as offered to all other consumers. MHMRTC does not guarantee that a MHMRTC consumer or any number of MHMRTC consumers will utilize any particular provider. Each consumer is given information regarding all providers in the provider network and then makes the choice of provider(s). Providers are required to immediately call MHMRTC’s Risk Management Department at (817) 335-3022 and to contact each consumer’s MHMRTC Designated Staff Liaison to report occurrences of the following: Client deaths Suicide attempts Serious injuries – injuries which require medical care Serious medication errors Adverse Drug Reactions Allegations of homicide, attempted homicide, threat of homicide with a plan 3 Incidents of restraint or seclusion Confirmed abuse, neglect, or exploitation Discovered pharmacy errors Providers are required to inform consumers that they have the right to report any complaints about the services they are receiving to the Consumer Complaint Reporting Line at: (817) 569-4367 or 1-888-636-6344 (toll free) All provider complaints and/or suggestions are to be communicated to the Director of Contracts Management/Provider Relations at (817) 569-4456. All suspicions of client abuse are to be reported to the Texas Department of Family and Protective Services at 1-800-252-5400 or www.txabusehotline.org. Referral and Authorization Processes Referral Process All referrals to Provider will come from the MHMRTC Licensed Practioner of the Healing Arts (LPHA) after the LPHA determines that a Covered Individual meets medical necessity criteria for the delivery of Resiliency and Disease Management services and authorizes the delivery of those services. Authorization for services may only be made by an LPHA from MHMRTC. 412.322 (c )(2) 419.455 (2) 419.453 (30) Determination that there is a medical necessity for Medicaid MH rehabilitative services for the individual has been made by an LPHA. Medical necessity--evidenced by LPHA signature on the DMN form E-019 or the LOC-A printed from WebCARE. There is no guarantee that Provider will be used by a Covered Individual or any number of Covered Individuals. The LPHA will offer the Covered Individual a choice of providers from the list of contracted Providers. Covered Individuals will document their choice and are allowed to change Providers. Provider will not engage in case finding or otherwise locating individuals to receive rehabilitative services and is prohibited from offering any gift with a value in excess of $10 to potential clients and from soliciting potential clients through direct-mail or by telephone. 4 Authorization of Services When a client is identified as needing Resiliency and Disease Management services and agrees to participate, the MHMRTC LPHA, will authorize the type and amount of service to be provided during the first 90 days. Once a Provider has been selected by the client, an Authorization letter will be generated and sent (typically faxed) to the selected Provider along with the client’s diagnosis and a copy of the Rehabilitative Service Plan. The Authorization Letter will include the Covered Individual’s name, the date services are authorized to begin, the type and quantity of services authorized, the lapse date for the Authorization (by when the services must be provided or will no longer be authorized), and the Authorization Number. Provider will not be reimbursed for services not pre-authorized with an Authorization Number. The LPHA is responsible for following up with the Provider within 5 to 15 working days from the referral to confirm the Provider was able to contact the client. The Provider must develop a Treatment Plan for the Rehab services and begin services. The treatment plan needs to be completed within 10 days of the auth. The plan needs to meet the following requirements: 419.456 Treatment plan (Present) developed within 10 day after authorization is 412.322( e ) a (2) obtained (TP signed within 10 days of LOC-A) At a minimum a staff member credentialed as a QMHP-CS must complete 412.322( e )(1) and sign the plan 412.322 (e) (1) Description of A presenting problem, B needs related to MI, C strengths, D (A)-(G) preferences, E assessment , Physical health, G COPSD complete 412.322 (e) (1) A description of the presenting problem section A (A) 412.322 (e) (1) A description of the individuals strengths C (B) 412.322 (e) (1) A description of the individuals needs arising from the mental illness section (C) B/ E related needs 412.322 (e) (1) A description of the /physical health issue/COPSD section G and F (D) 412.322 (e) (1) A description of the expected outcomes (E 412.322 (e) (1) An expected date for recovery goals to be achieved (F) 412.322 (e) (1) List of resources for recovery ( last section of plan after signatures or (G) brochure) 419.465 List of types of services (services to be delivered must be checked or written 412.322 (e) (1) (a) (3) out code or name of service) (H) (A) 412.322 (e) (1) List of strategies to be implemented by staff to achieve goals (Strategy (H)(i) statement listed) 412.322 (e) (1) The frequency, number of units, and duration of each service to be provided (H)(ii) is present. 412.322 (e) (1) The credentials of staff providing the service are present. (H)(iii) 412.322 (e) (2) Goals address individual s needs, preferences, experiences, and cultural (A) background. 412.322 (e) (2) Goals must address the individuals COPSD issue and or physical health (B) disorder. 412.322 (e) (2) Goals are expressed in overt, observable actions of the individual. (C ) 412.322 (e) Goals must be objective and measurable - using quantifiable criteria. 5 (2)(D) 412.322 (e) (2)(E) 412.322 (e) (2) (A) 412.322 (e) (2) (B) 412.322 (e) (2) (C ) 412.322 (e) (2)(D) 412.322 (e) (2)(E) 412.322 (e) (3) 412.322 (f) (1) (A) 412.322 (f) (1) (B) 412.322 (f) (1) (C) Goals reflect individual autonomy, self direction, and desired outcomes. Objectives address individual’s needs, preferences, experiences, and cultural background. Objectives address the individuals COPSD issue or physical health disorder. Objectives are expressed in overt, observable actions of the individual. Objectives are objective and measurable using quantifiable criteria. Objectives reflect individual autonomy, self direction, and desired outcomes. Copy of plan provided to the individual or explanation of reason why copy is not given. REVIEW Review plan prior to requesting authorization for the continuation of services. 3403 documented before 475/473 Review plan in its entirety, at least every 90 days. Determine if the plan is addressing needs of individual. Narrative comments by staff and client. 419.456 Document progress on all goals and objectives and any recommendation for 412.322 (f) (1) (d) (1) continuing services, change for services, discharge from services. Check (D) (A) box's marked. Record documentation must be legible to others (other than author) Record must have Medicaid # and client's name on each page of significant documents, effective 11/1/99 6 Reauthorization of Services Local Authority LPHA is responsible for reauthorization and determination of medical necessity. As part of the Determination of Medical Necessity (DMN) oversight required by the Medicaid Rehab guidelines, the Local Authority LPHA will determine medical necessity of services outlined in the Provider’s Treatment Plan which is then reviewed at least every ninety (90) days. To ensure rehab services maintain a valid authorization status, at least two (2) weeks prior to the lapse of the Treatment Plan, Provider should review the client’s Treatment Plan, reassess the client, and request reauthorization of the current Service Package or authorization of a Service Package that will meet the client’s needs. The Provider will receive an Authorization Letter for continued services which will include an Authorization Number specific to the Covered Individual, the type and amount of service authorized, and the dates during which the services are authorized. Services must be authorized in this manner prior to delivery of services for the Provider to be paid. Providers can confirm authorized status in WebCARE Report Screen #251 for adults. Occasionally, a Covered Individual will drop out of services or cannot be located by the LPHA to reauthorize services. If such an individual presents with the Provider for services, Provider must reassess the client and request authorization the same day via entry in WebCARE. When the Level of Care Recommended (LOCR) equals the Level of Care Authorized (LOCA), the assessment date is used as the effective date of authorization. When the LOCR does not equal the LOCA, the WebCARE data entry or ‘add’ date is used as the effective date of authorization. Thus, when the LOCA is different from the LOCR, the date the assessment is entered into WebCARE is the earliest that billable services will be covered unless being reasssed during the already authorized period prior to assessment and authorization expiration. If a change in level of service is subject to Fair Hearing procedures, (reductions and terminations of level of care), the authorization date is delayed 10-14 days from the assessment date. (See Automatic Authorization Agreement and TAC 357, Subchapter A Uniform Fair Hearing Rules.) NOTE: Review of Plans and reauth- we currently as the provider complete a new plan when a client is new, autoclosed, or changes packages. Reviews are to be done at least every 90 days. Additionally the review occurs prior to request of authorization. The rule explicitly requires this. REVIEW 412.322 Review plan prior to requesting authorization for the continuation of services. (f) (1) (A) 3403 documented before 475/473 412.322 Review plan in its entirety, at least every 90 days. (f) (1) (B) 412.322 Determine if the plan is addressing needs of individual. Narrative comments by (f) (1) (C) staff and client. 419.456 Document progress on all goals and objectives and any recommendation for 412.322 (d) (1) continuing services, change for services, discharge from services. Check box's (f) (1) (D) (A) marked. Discharge from ServicesProvider must consult with the LPHA and obtain approval prior to discharging a Covered Individual from rehabilitative services. Discharge requests will comply with MH014, Mental Health Services Discharge Process. 7 Services Covered Services Covered Services are those services which are determined by Local Authority to be Medically Necessary Services when authorized as part of the current UA-RDM assessment and treatment plan of the Covered Individual approved by a Licensed Practitioner of the Healing Arts. Provider is prohibited from providing more than one rehabilitative service to an individual at the same time and on the same day. The services proposed to serve any individual in the authorized level of care of Service Package are: reasonable and necessary for the diagnosis or treatment of a mental health disorder or a cooccurring psychiatric and substance use disorder (COPSD) in order to improve or maintain the individual’s level of functioning; in accordance with professionally accepted clinical guidelines and standards of practice in behavioral health care; furnished in the most clinically appropriate available setting in which the service can be safely provided; provided at a level that is safe and appropriate for the individual’s needs and facilitates the individual’s recovery; and could not be omitted without adversely affecting the individual’s mental or physical health or the quality of care rendered (Reference: Texas Administrative Code §412.303 Definitions, (39) Medical necessity). Diagnosis- 412.322(b) 419.455 1 ( c) Client is an adult with severe and persistent mental illness or a child or adolescent with a serious emotional disturbance. MI documented covering the time services were rendered. Diagnosis should be completed at least one time annually by licensed staff acting within the scope of their license- all 5 axis should be addressed and should meet DSHS contract requirement. Primary axis must be indicated. The diagnosis is batched to CARE along with the registration information as it is entered into CMHC. If new generation medication is prescribed the data must be recorded and provided so that it can be reported to the DSHS in the weekly batch. Data must be entered in a timely manner according to the attached procedure. Documentation 8 Provider must maintain records necessary to verify services delivered and billed to MHMR of Tarrant County. Provider must additionally maintain records including the following: 1. 2. 3. 4. 5. 6. 7. Names of all Covered Individuals enrolled with Provider Evidence of licensure, certification or accreditation, as required Evidence of Life Safety Code or ADA inspection and compliance, if applicable Evidence of insurance coverage Evidence of criminal history checks of staff Evidence of required staff training If Covered Individuals are paid by Provider, evidence of compliance with Department of Labor (DOL) regulations regarding salaries and pay 8. Doctor’s orders and medication records if medications are administered by Provider staff 9. Fire Marshall inspection and results of fire drills 10. Evidence of annual health department inspection for day programs which serve or prepare food for 10 or more Covered Individuals. Provider will retain records for a minimum of seven (7) years. Provider will receive, store, process, or otherwise deal with client information, if any, accessed or generated during services in compliance with Chapter 414, Subchapter A, Client Identifying Information, of Title 25 of the Texas Administrative Code. Service Documentation The Provider is responsible for documenting all services. All service documentation must meet all Mental Health Community Services Standards, and Medicaid Rehabilitation documentation requirements. Registration: client must be registered in CARE. Diagnosis: All 5 axes completed, signed and dated by LPHA at least annually and primary axis indicator identified. Assessments The Provider is responsible for ongoing assessments of the Covered Individual’s need for and response to specific rehabilitative services. These assessments occur in collaboration with the Covered Individual and, minimally, identify the following: the Covered Individual’s recovery goals; the Covered Individual’s changing clinical needs the Covered Individual’s natural supports and current use and benefit from those supports; and the demands and adaptability of the Covered Individual’s chosen environments. 412.322 (a) (2) 412.322 (d) (1)(A) Obtain authorization from the department (DSHS) (doc in CMHC or WebCARE) 419.456 a 1 (A) 9 419.456, 419.465 (b) (2) (B) Services delivered must be within service package authorized. Assessments must meet DSHS contract reqs for frequency and content by properly credentialed staff. QMHP every 90 days – must be entered in a timely manner. Treatment Plan Requirements The Provider is responsible for developing a Treatment Plan with goals and objectives for the client which must conform to the standards of the Mental Health Community Services Standards, Texas Administrative Code 412 G, section 412.322 and must be developed within ten (10) working days from the initial authorization. Treatment Plans must be signed by the assigned Provider staff and the client and a copy provided to the LPHA upon request. Treatment Plans must, at a minimum, be reviewed and updated every ninety (90) days, or more often if clinically indicated. Treatment plan (Present) developed within 10 day after authorization is obtained (TP signed within 10 days of LOC-A) At a minimum a staff member credentialed as a QMHP-CS must complete and sign the plan Description of A, B, C, D, E, F, G complete A description of the presenting problem section A A description of the individuals strengths C A description of the individuals needs arising from the mental illness section B/ E related needs A description of the /physical health issue/COPSD section G and F A description of the expected outcomes An expected date for recovery goals to be achieved List of resources for recovery ( last section of plan after signatures or brochure) List of types of services (services to be delivered must be checked or written out code or name of service) List of strategies to be implemented by staff to achieve goals (Strategy statement listed) The frequency, number of units, and duration of each service to be provided is present. The credentials of staff providing the service are present. Goals address individual s needs, preferences, experiences, and cultural background. Goals must address the individuals COPSD issue and or physical health disorder. 10 Goals are expressed in overt, observable actions of the individual. Goals must be objective and measurable - using quantifiable criteria. Goals reflect individual autonomy, self direction, and desired outcomes. Objectives address individual’s needs, preferences, experiences, and cultural background. Objectives address the individuals COPSD issue or physical health disorder. Objectives are expressed in overt, observable actions of the individual. Objectives are objective and measurable using quantifiable criteria. Objectives reflect individual autonomy, self direction, and desired outcomes. Copy of plan provided to the individual or explanation of reason why copy is not given. Treatment Plans must, at a minimum, be reviewed and updated every ninety (90) days, or more often if clinically indicated. Review plan prior to requesting authorization for the continuation of services. 3403 documented before 475/473 Review plan in its entirety, at least every 90 days. Determine if the plan is addressing needs of individual. Narrative comments by staff and client. Document progress on all goals and objectives and any recommendation for continuing services, change for services, discharge from services. Check box's marked. Record documentation must be legible to others (other than author) Record must have Medicaid # and client's name on each page of significant documents, effective 11/1/99 Progress Notes Progress Notes must be completed for all services delivered, and must reflect the service that took place, client behaviors, situational stressors, needs, issues that arise, and the individual’s progress or lack of progress towards the anticipated service outcome. Progress notes should convey clinically relevant detail about the client by documenting: 1. 2. 3. 4. 5. 6. the affect, attitude, and behaviors of the individual’s participation positive or negative symptoms of their mental illness observed, (or when asked) positive or negative side effects of their medication taken as observed, (or when asked) any clinically relevant issues that arise during the course of service delivery progress (or lack of progress) toward the desired objectives or goal; and in terms that documents evidence of medical necessity by a. maintaining or improving client functioning; b. in the clinically most appropriate setting services can be safely provided; 11 c. provided at a safe and appropriate level for the individual’s needs and facilitates the individual’s recovery; and d. cannot be omitted without adversely affecting the individual’s mental or physical health or the quality of care rendered (TAC §412.303 (39) Medical Necessity). Progress notes must conform to the Medicaid billing requirements and the standard of the MH Community Services Standards, in §412.326: It is against the rules to reimburse for travel. REQUIRED IN EVERY REHAB NOTE: Progress note present 412.326 (2) 419.463 a (1) 419.463 (a) (4) 419.463 (a) (5) 419.463 (a) (6) 419.465 (I) 419.463 a (2) 412.326 (9) 419.463 (a) (3) 412.326 (8) 412.326(13) 412.326(13) 419.465 (a) (1) 419.463 (a) (7) 419.463 (a) (7) Client's name/ recipient Service date Duration (Stop/Start Time) Location/Setting Client present and awake Type of service provided is supported by sac used The specific skill trained on and method used to provide the training is documented Service is face to face to individual or primary care giver of child adolescent Provider signature and date Credentials of provider 412.326 (6) 419.463 (b) (4) (A) A summary of the activities that occurred; 412.326 (7) 419.463 (b) (4) (B) 412.326 (1) 412.326 (3) 412.326 (4) 412.326 (5) 419.463 (b) (4) © 412.326 (11) 412.326 (14) 412.326 (120 419.463 (b) (4) (D) 419.315 (d) 419.456 (a) (1) 412.326 (10) The modality of service provision (i.e. one-to-one or group); The treatment plan goal's that was the focus of the service; and The treatment plan objective's that was the focus of the service listed on note or written out. Any pertinent event or behavior relating to the individuals treatment which occurs during the provision of service is documented within the note. Status/progress toward treatment Goals Service Provided was provided in excess of LOC-A The title of curriculum being used associated with rehab services only. Additionally per service type 419.463 (b) (1) (A) The outcome of the individual's crisis; 12 419.456 b (1) (A) If the service is a crisis - Medical necessity must be determined within 2 business days after the provision of crisis services 419.463 (b) (2) Medication Training & Support Services Applies to Children For medication training and support services and skills training and development services, the name of the primary caregiver or LAR to whom the service was provided, if applicable; 419.459 (b) (3) Medication Related/Psychosocial services must be provided by licensed medical personnel ( Dr, PA, RN, LVN, pharmacist) Psychosocial rehabilitative coordination services 419.463 (b) (3) (A) A description of the coordination service provided; 419.463 (b) (3) (B) If the service involves face-to-face or telephone contact, the person with whom the contact was made; and 419.463 (b) (3) (C) The outcome of the service. NON REIMBURSABLE ACTIVITIES 419.453 (16) 419.465 (2) (B) 416.456 (1) 419.465 (2) (A-D) A B C D If group service code, Adult group size must be more than 1 and less than 9 clients Children's groups 2 staff up to 6 kids A Medicaid MH rehab service that is not auto's in accordance with 419.456 Service code used is upcoding Service is a duplicate service Service is provided in excess of amount auth'd Department will not reimburse for more then: 2 hrs per day med training (2515,2516) 4 hrs per day psychosocial rehab (2919) 4 hrs per day rehab counseling/therapy (2921) 4 hrs per day skills train/dev (2923, 2924) The cost of the following activities are included in the Medicaid MH rehabilitative services reimbursement rate(s) and may not be directly billed by the Medicaid provider: 419.465 (a) (2) (A) Developing and revising the treatment plan and interventions that are appropriate to an individual's needs (3403) 419.465 (a) (2) (B) Staffing and team meetings to discuss the provision of Medicaid MH rehabilitative services to a specific individual; 419.465 (a) (2) (C) Monitoring and evaluating outcomes of interventions, including contacts with a person other than the individual 419.465 (a) (2) (D) Documenting the provision of Medicaid MH rehabilitative services (44) 419.465 (a) (2) (E) A staff member traveling to and from a location to provide Medicaid MH rehabilitative services (7) 419.465 (a) (2) (G) Administering the uniform assessment (405,406) 13 419.465 (2) (B) Services incidental to another service If group service code, group size must be more than 1 and less than 9 clients A Medicaid MH rehab service that is not auth'd in accordance with 419.4556 14 Claims & Billing Gateway Portal User’s Manual Using the Web Interface 1. Access to the website can only be granted by going through the MHMRTC IT department. To obtain a user ID and password contact the MHMRTC Director of Contracts Management/Provider Relations at 817.569.4456 or providerrelations@mhmrtc.org 2. Finding the Website Go to web address https://gateway.mhmrtc.org/ 3. User Login Enter your assigned user ID and password. Click on the “Log In” button. 15 4. If you have logged in incorrectly, it will display the message “Null User” and refresh the page until you enter the correct username and password. Please contact IT if you do not have the correct log in information. 5. If you have logged in correctly, the following service entry screen will display. 6. Understanding Data Entry Requirements A grid of text fields is displayed to represent data for one encounter. All fields are required unless otherwise specified. a. Prov ID Enter the 4 character provider identifier assigned by MHMR. If you logged in as a provider, this field will automatically default to your ID. If you have two provider IDs, make 16 sure this matches the one you want to use. It can be edited. b. Service Date Enter the date of service. Formats accepted o mm/dd/yy o or mmddyy o mm/dd/yyyy For example, a service date of October 5, 2005 can be entered as 100505 or 10/05/05 or 10/05/2005. c. Time In / Time Out Enter the start time for the service. Enter the end time for the service. Formats accepted (Time In, Time Out displayed for threethirty pm to five pm example) o o o o hh:mm (military) hh.mm (military) hh:mm AM/PM hh.mm AM/PM 15:30, 17:00 15.30, 17.00 03:30 AM, 05:00 PM 03.30 AM, 05.00 PM Note: Must use leading zeros where necessary when using a decimal to replace colon. d. Service Code Enter the code used to bill or report the service. It is the service code on the claim It is also located on the letter of authorization. e. Diagnosis Code * (Required for MH providers only) Format is XXXXX or XXXXXX These are the standard DSM IV codes without the decimal points. f. Staff Id * (Required for MH providers only) Enter a unique staff id of the person who provided the service. g. License Type Enter the server type of the person who provided the service. Format is a 2-digit code. Specific values are accepted based on the codes below. Please contact Pam Nash at 817-569-4436 for further questions regarding which codes to use. 17 Code 01 03 05 07 09 11 13 16 17 19 21 23 25 27 29 31 33 35 37 39 43 44 45 47 49 50 51 52 53 98 Description Physician Psychologist/PhD. APN/Prescript Authority Only LMSW-ACP LMFT LMFT Temporary License LPC LMSW Dietician Occupational Therapist Physical Therapist Speech Therapist Music Therapist Cert Recreational Therapist RN LVN Cert. Medication Aide QMHP-CS QMRP Psychological Associate CSSP LCDC Counselor in Training (C.I.T) Dentist Other Prof/NOT LPHA Other EIS-EL EIS-FQ Residential Staff h. Location Enter the location where the service took place. Value must be one of the 2-character codes below. Code HM OF GH JA SC SF OT SH SR CS NF Description Home Office/clinic General Medical Hospital Jail or juvenile detention center School Service facility, e.g. nursing home, detox center, sheltered workshop Other State mental health facility State mental retardation facility Community Setting not otherwise described Nursing Facility 18 CI Community IMD State funded community hospital, Lubbock, Houston, and Galveston only. CH i. Client ID Enter the 9 digit MHMR client ID. Must have leading zeros if less than 9 digits. j. Provider Client ID (optional) Provider may choose to enter their own client ID for tracking services No specific format. k. Encounter Type – Choose from the following codes that describe the encounter (or intended encounter type if no-show). Defaults to “F”, if not modified. Code F E T Description Face to face Video telehealth or telemedicine Telephone l. Appointment Type Please choose from the following codes that describe the nature of the appointment. Code 1 2 3 4 Description Scheduled appointment for service kept Unscheduled service Scheduled appointment canceled by provider Consumer cancellation or no show If a no-show is reported, the service must be marked as non-billable and the time in/out should be the same to indicate zero client time. Defaults to “1” if not modified. m. Recipient Code Choose from the following codes to indicate the recipient (or intended recipient) of the service. Code 1 Description Consumer 19 2 3 U Collateral Consumer and family member/LAR simultaneously Unknown Defaults to “1”, if not modified. n. Billable Check Box Automatically defaults to billable. Uncheck this box, only if you want to report encounter data that is not billable. No-shows are considered nonbillable. 6. After you enter the data for one claim, hit the “Done” button on the right side of the screen. A grid will display below showing the data that has been added to the batch. The grid displays the duration calculated in hours for the Time In and Time Out entered. Be sure to verify this is correct. 20 The data in the text-fields defaults to what the user entered previously to reduce the amount of entry. Only changes need to be made before submitting another service to the batch. As services are added they are displayed in the grid for review before submission. The system will not allow a duplicate entry and will display an error message in red at the top of the screen as follows. Client ID, Date/Time, or Service Code must be different in each line. The system also does some validation on the date and time format where possible. Error messages will display in red to address these issues. Please contact Steven Forrester of Information Technology if assistance is needed interpreting the error messages. Claim Dollar Amount will be entered. 7. Editing/Deleting Data from the Batch Before Submission Edits can be done within the grid during review before submission. To make an edit hit the “Edit” button on the left side of the claim that needs to be updated. The fields become editable in text fields as displayed below (in line 3 of the grid) and two buttons appear to the left of the data. “Update” and “Delete” buttons. 21 You can make the necessary changes and hit the “Update” button. To delete the entire entry, hit the “Delete” button and the grid will display an empty line to confirm there was a deletion. 8. Submitting a Batch Once you have entered the amount of claims/encounter data that you choose to batch together, the data can be submitted for validation. Hit the “Submit” button in the top left corner of the page. The grid will be cleared and you will receive a batch reference code filename with a .xml extension. It will display at the top of the page above the “Submit” button. You must record this code in case there are any issues you need to bring to the attention of IT. It is the way the batch is tracked. This reference code will also be used by you to check if any errors were caught in the validation process before any claims are processed. 22 9. Checking Errors In order to catch errors early in the process, the batch data will be validated for errors so that they can be resubmitted and processed in a timely manner before the claim gets denied. Some of the error checks include: o Valid client ID o Valid provider ID o Valid service code o Valid location code o Valid license type o Gateway portal will also search for the correct authorization number for billable services. This does not have to be entered. If the authorization number is not found and it is marked as billable, then that will also generate an error. Fund source is also looked up for billable services that have an authorization. Within a few seconds after you have submitted a batch, your response file will be available. You must hit the “Check Responses” button located in the upper left hand corner of the page. The number of responses available is displayed under the button. You must refresh the page in order for this number to be updated as you submit any batches. 23 When you hit the “Check Responses” button, the following screen will be displayed. This will display a list of batches submitted under your log in. Choose the one that matches the reference code displayed after you submitted the batch. The text area will display the response for the batch that you choose. You may also choose to print the response by hitting the “Print Response” button. If the batch had no errors you will receive the message: Starting processing on file: <path name to xml reference file name> Finished processing Successfully wrote to CMHC file <CMHC filename with date stamp> If the file contained errors the response will display an error message with the data submitted that caused the error. Errors need to be researched and resubmitted in another batch. Good “claims” in the batch will go on to be processed. They do not need to be resubmitted. The response should also display a message with the CMHC filename and date stamp to be processed with the claims that went through. If there is a message stating no output was sent to CMHC or there is no CMHC file name at the end of the response file, 24 then none of the claims submitted within the batch went through. Please contact the MHMR IT Dept. if you believe it is a mistake. 10. Correcting Errors Once you have researched the errors, the data can be resubmitted via the web page in another batch. Data in the first batch that was accepted will go on to be processed. 11. Processing Claims For MHMR staff, you will find the batch in MCO waiting to be processed. The name of the file will match the CMHC file name in the response file for the batch. You can run the Edit/Check claims process to find any claim files that need to be processed. Using the SFTP file transfer Method 1. In this method, providers are allowed to transfer a file to MHMR instead of manually entering the data. The file must be in a specific format. 2. File Format The file format for the input file will be an XML document. The root element will be <Services>. <Provider> will be the next element with ID as an attribute. All billable/non-billable services are child elements within the Provider element. All service details are attributes of the service element. See below for details. XML Schema <?xml version="1.0" encoding="UTF-8" ?> <Services> <Provider ID=""> <Service MHMRClientID="" ProviderClientID="" LocationCode="" ServerType="" StaffID="" ServiceDate="" ServiceTime="" ServiceDuration="" ServiceCode="" TotalAmountBilled="" DiagnosisCode="" Billable="" AppointmentTypeCode="" EncounterTypeCode="" RecipientCode="" ProgressNotes="" /> </Provider> </Services> Provider element Supplies information related to a particular provider Attributes 1. ID (4 chars) Service element Supplies information about each service Attributes 25 1. MHMRClientID (9 chars) Insert leading zeros if <9 chars 2. ProviderClientID (10 chars max) (optional field) 3. LocationCode (state defined codes, must be one of the following) Possible Values Descriptions HM Home OF Office/clinic GH General Medical Hospital JA Jail or juvenile detention center SC SF School Service facility, e.g. nursing home, detox center, sheltered workshop OT Other SH SR CS NF CI State mental health facility State mental retardation facility Community Setting not otherwise described Nursing Facility Community IMD State funded community hospital, Lubbock, Houston, and Galveston only. CH 4. ServerType The CMHC license type codes will be used and converted to the state codes by us. Code Description 01 Physician 03 Psychologist/PhD. 05 APN/Prescrip Authority Only 07 LMSW-ACP 09 LMFT 11 LMFT Temporary License 13 LPC 16 LMSW 17 Dietician 19 Occupational Therapist 21 Physical Therapist 23 Speech Therapist 25 Music Therapist 27 Cert Recreational Therapist 29 RN 31 LVN 33 Cert. Medication Aide 35 QMHP/QMHP-CS 37 QMRP 39 Psychological Associate 43 QMHP-P/CSSP Para Prof/NOT QMHPP or 44 QMRPP 26 45 47 49 50 51 52 53 98 LCDC Counselor in Training (C.I.T) Dentist Other Prof/NOT LPHA Other EIS-EL EIS-FQ Residential Staff 5. StaffID – provider’s staff ID 6. ServiceDate - mmddyyyy is format required 7. ServiceTime - hh:mm AM/PM is format required 8. ServiceDuration – hh:mm 9. ServiceCode (8 chars max) 10. TotalAmountBilled (dollar format with two decimal places ex. 5.00) 11. DiagnosisCode (6 digit numeric field without decimal. The diagnosis code cannot be more than 6 characters. 12. Billable (The value can either be “True” or “False”) Optional Fields 13. AppointmentTypeCode Code 1 2 3 4 Description Scheduled appointment for service kept Unscheduled service Scheduled appointment canceled by provider Consumer cancellation or no show **Values 3 and 4 must have “00:00” for service duration field** 14. EncounterTypeCode Code F E T Description Face to face Video telehealth or telemedicine Telephone 15. RecipientCode Code 1 2 3 U Description Consumer Collateral Consumer and family member/LAR simultaneously Unknown 16. ProgressNotes – free text 27 Note: Non-billable encounters must be reported in this file. encounters all rules apply with the following requirements. Billable = “False” AmountBilled= “0.00” For non-billable 3. Once the file is in the correct format and tests have been run for verification, a file can be transferred. 4. To transfer the file An SFTP client must be downloaded on the machine of the person who will transfer the file. This is only done once. The client is an executable file that can be sent to the provider via email. Open the SFTP client Enter the assigned username and password Enter “email.mhmrtc.org” for the host name without the quotes. Hit the “Log In” button A screen displays with file navigation on the left side and two directories for the provider on the right side—an inbound and outbound. 28 You can drag the xml input file from the left side into the inbound directory on the right side. Note: The xml file name is not restricted so a provider is allowed to name it anything. Be sure to use a file naming convention that is easy to track and ensures each file has a unique name so that no files are overwritten. 29 The above message displays after a file is dropped into the directory. Hit the “Copy” button to copy the file to the Inbound directory. The outbound directory is where you will find any error responses for the file you transfer. It will be available within an hour after transfer. Only service data for those that have errors need to be resubmitted after corrections are made. Do not resubmit the whole batch. Open the response file that matched the name of the input file with the word “response” in front of it. 30 Please contact the MHMR IT department for help understanding the error messages or for any questions. in Contact Information MHMR of Tarrant County Help Desk ITAutomated.Helpdesk@mhmrtc.org 817-569-4357 Appeal of Denial If a claim is denied and Provider feels the claim should be paid, Provider must resubmit the claim and appeal the decision within 30 days of denial. Appeals or resubmission after the 90-day window for filing with Medicaid will not be paid. Appeals of claim denials must be made in writing to: Kevin McClean, Director of Contracts Management/Provider Relations MHMR of Tarrant County P.O. Box 2603 Fort Worth, Texas 76113 31 Reporting Requirements 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. Critical Incidents Providers are required to call (817) 335-3022 with information regarding the occurrence of any of the following critical incidents immediately: Deaths Suicide Attempts Serious Injuries – injuries which require medical care Serious Medication Errors – the incorrect or wrongful administration of a medication (such as a mistake in dosage, route of administration or intended individual), a failure to prescribe or administer the correct drug, medication omission, failure to observe the correct time for administration, or lack of awareness of adverse effects of drug combinations which place the Covered Individual’s health at risk so that immediate medical intervention or enhanced surveillance on behalf of the Covered Individual is required. Adverse Drug Reaction (ADR) – those responses which are above and beyond the common side effects usually encountered with each medication (unless they are extreme cases). They are undesired and unintended, possibly harmful responses to a drug administered at a normal dosage. Responses may include problems related to cumulative effects, tolerances, and dependency for single-drug administered and drug-drug interactions or multiple drugs administered. Reportable ADRs require some change in the clinician’s care of the client, including the option of discontinuing the medication, modifying the dose, prolonging hospitalization, or taking action to initiate supportive care. Allegations of Homicide, Attempted Homicide, Threat of Homicide with a Plan Confirmed Abuse, Neglect, or Exploitation Discovered Pharmacy Errors – a pharmacy dispensing error including one or more of the following: a. Incorrect Label or Directions for Use b. Failure To Place Warning Label on Container as appropriate c. Incorrect Medication d. Incorrect Strength e. Incorrect Quantity f. Expired Medication g. Contraindicated Drug Hospitalizations 911 Called Physical Aggression Auto Accident Fire DNR Order (Do Not Resuscitate) Elopement (Missing Person) Infectious Diseases Criminal Activity Litigation Threat 32 Reports Provider will submit the information on the following forms. It is recommended that Provider use the attached report forms provided by the Local Authority. At a minimum, the following must be reported: a. Discharges from services during the month (list of names). b.Critical Incidents c. Staff added, with credentialing status d.Results of internal reviews of risk incidents, quality, and billing audits e. Results of audits by any external licensing or accrediting bodies f. New Generation Medication data Provider will submit Report(s) in writing to: MHMR of Tarrant County Provider Relations P.O. Box 2603 Fort Worth, Texas 76113 Information may also be submitted by fax to (817) 569-4491. 33 MHMRTC Report FAX to Provider Relations at 817-569-4491 Provider: ________________________________ Data for the month of ___________ 1. Staff added since last report: Name QMHP LPHA ____________________________________________________________________________________ ____________________________________________________________________________________ ____________________________________________________________________________________ ____________________________________________________________________________________ ____________________________________________________________________________________ ____________________________________________________________________________________ 2. Number of Covered Individuals with the following incidents: ________ Deaths ________ Suicide attempts/threat with a plan ________ Serious injuries ________ Serious medication errors -- Attach a written report for each ________ Adverse Drug reactions -- Attach a written report for each ________ Alleged homicides/attempted homicides/threat of homicide with a plan ________ Confirmed Abuse, neglect, exploitation ________ Discovered Pharmacy errors ________ Complaints -- Attach a description of each and indicate when and how resolved 3. Attach the results of any internal review of the above risk incidents and describe any action planned or taken to reduce future occurrences. 4. Attach the results of any internal quality review of the services provided under this contract. Include any action planned or taken to resolve identified areas of concern. 5. Attach the results of internal billing audits, showing number of records reviewed and percentage of compliance with Medicaid documentation requirements. Note: Provider is expected to review at least 10% of all records. 1. Number of RN or LVN peer reviews conducted regarding services to Covered Individuals and whether findings were reported to the licensing boards. 7. Attach a copy of or summary of findings from any external audit of Provider related to services provided under this contract. Indicate any corrective action that is required of Provider from the external review. 8. Attach a list of enrollments and discharges from covered services during the month (list by name) Report completed by: _________________________ _________________________ ________________________ Printed name Signature Date completed/submitted _________________________________ Provider Relations _____________________________ Date received MHMRTC 34 Adverse Drug reaction(s)/Clinical Follow-up Report Provider: _______________________________ Prescribing Physician: ___________________________________ Covered Individual Name: ________________________________________________ MHMRTC ID Number: _____________ Name of drug(s) involved: ___________________________________________________________ Date drug started: _________________________ Date adverse reaction noted: _______________ List all drugs prescribed at time of adverse reaction: ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ __________________________________________________________ Description of adverse reaction: ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________ Impressions/Clinical response to incident (actions taken): ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________ _________________________________________ Provider signature/title _______________________________________ Date submitted _________________________________________ MHMRTC Provider Relations _______________________________________ Date received _________________________________________ MHMRTC Nursing Director _______________________________________ Date reviewed This report must be submitted to MHMRTC by the fifth working day of each month. Report may be faxed to Provider Relations at (817) 569-4491. 35 MHMRTC Serious Medication Error(s)/Clinical Follow-up Report Provider: __________________________________ Prescribing physician: ______________________________ Covered Individual Name: ________________________________________________ MHMRTC ID Number: _________________ Name of drug(s) involved: ________________________________________________________________ Date drug started: _________________________ Date adverse reaction noted: ___________________ Description of the error: ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ________________________________________________________ Clinical response to incident (actions taken): ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ________________________________________________________ Overall trends/patterns related to medication error(s) identified: ____________________________________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________________ ____________________________________________________________ _________________________________________ Provider signature/title _______________________________________ Date submitted _________________________________________ MHMRTC Provider Relations _______________________________________ Date received _________________________________________ MHMRTC Nursing Director _______________________________________ Date reviewed This report must be submitted to MHMRTC by the fifth working day of each month. Report may be faxed to Provider Relations at (817) 569-4491. (Additional forms may be found in Attachment 1) 36 Staff Training Overview If Provider is licensed or accredited by a state or federal regulatory agency, some training requirements may be waived. In such cases, the Provider is required to provide external audit reports related to accreditation, licensure or certification. If Provider is not licensed or accredited, the Provider is required to provide training to all staff working with Local Authority clients. Training noted as such on the following training grid must be completed on-line except for 3 courses that will be provided through the MHMRTC Training Center or obtained from another entity. Training obtained from other entities must be related to the required job competencies as determined by the Texas Administrative Code and the Texas Department of State Health Services. Providers may submit training policies, procedures and materials to verify that training requirements are met. Providers may receive assistance, upon request, from the Local Authority with regard to training. The Local Authority will charge for training provided to Provider staff in the classroom. Scheduling Training with MHMRTC Provider is responsible for ensuring all staff receives the required training prior to contact with Local Authority clients. Provider may register staff for classes by email to at least one week prior to class scheduled to training.request@mhmrtc.org or calling 817-569-4342. When scheduling training please provide a list of the names of those who will attend and which classes they will be attending. A confirmation will be sent when class is scheduled, Provider will be billed for any persons registered for classes who do not attend unless The Training Center receives a cancellation notice by fax at least twentyfour (24) hours prior to the scheduled class MHMRTC Training also offers several online courses through Essential Learning. Required Training Elements Provider, its employees and agents who routinely perform any job duty in proximity to persons served must demonstrate competency in the safe management of verbally and physically aggressive behavior before contact with persons served and annually thereafter. Provider, its employees and agents must demonstrate a thorough understanding of the relevant elements of reporting, investigating, and preventing abuse, neglect, and exploitation (Client Rights) before contact with persons served and annually thereafter. Provider, its employees and agents must receive, read, and understand the MHMRTC Compliance Plan. Provider will agree to abide by the principles contained in the Compliance Plan, including its responsibility to report any known or suspected violations of the Plan. 37 Per the Texas Administrative Code (TAC) Title 25, Part 1, Chapters 404, 412, 414, 419 and the Fidelity Toolkit provided by the Texas Department of State Health Services, the following training is required for all staff who provide rehabilitative and case management services to Local Authority consumers. Description All Employees (1 Time) All Employees (1 Time) All Employees (1 Time) All Employees (1 Time) All Employees (1 Time) All Employees (Annual) All Employees (Annual) All Employees (Annual) All Employees (Annual) All Employees (Annual) All Employees (Annual) All Employees (Annual) Client Rights (1 Time) COPSD CPR (2 years) Defensive Driving (3 years) MH Adult Rehab (1 Time) MH Adult Rehab (1 Time) MH Adult Rehab (1 Time) MH Adult Rehab (1 Time) CourseTitle Computer Access Customer Relations Hazardous Chemicals New Employee Orientation OJT Checklist Abuse Client/Patient Rights Confidentiality and HIPAA Deficit Reduction Act Compliance Environmental Safety for Individuals with Developmental Disabilities Infection Control Part 1 Sexual Harassment and Workplace Harassment Rights & Abuse/Neglect COPSD/Dual Diagnosis CPR/First Aid/Seizures Defensive Driving Adult CM/Rehab Privileging Case Management Basics Overview of 412I, MH Case Management Services Overview of 419L, MH Rehab 38 Location of Training available MHMRTC training center MHMRTC training center MHMRTC online course through Essential Learning MHMRTC training center On-job site MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC link computer based MHMRTC training center MHMRTC training center MHMRTC training center MHMRTC training center MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MH Adult Rehab (1 Time) MH Adult Rehab (1 Time) MH Adult Rehab Specialty (3 years) MH Adult Rehab Specialty (3 years) MH Adult Rehab Specialty (3 years) MH Contact (1 Time) MH Contact (1 Time) MH Contact (1 Time) MH Contact (1 Time) MH Contact Specialty (3 years) MH Contact Specialty (3 years) MH Contact Specialty (3 years) MH Contact Specialty (3 years) MH Contact Specialty (3 years) MH Contact Specialty (3 years) MH Contact Specialty (3 years) MH Contact Specialty (3 years) MH Employees (1 Time) MH Employees (1 Time) MH Employees (1 Time) Services Skills Curriculum Mental Health Pharmacology/ SAM Checklist Medicaid-Adult MHMRTC training center MHMRTC online course through Essential Learning MHMRTC training center Patient/Family Ed TIMA/TRAG Age-Specific Care Bipolar Disorder Overview of Personality Disorders Understanding Schizophrenia Documenting the Treatment Planning Process Intentional Peer Support: About Peer Support Medication Management for Individuals with Developmental Disabilities Part 1 Motivational Interviewing Overview of 412G MH Community Standards Overview of Psychopharma cology Overview of Suicide Prevention Psychosocial Rehabilitation and Recovery MHMRTC Service Activity Logs--The Basics Rights & Abuse/Neglect Unit Specific 39 MHMRTC training center MHMRTC training center MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MHMRTC training center MH Employees (3 years) MH Employees (3 years) SAL Code Accessing Local and HHSC Benefits & Supports Bioterrorism MHMRTC online course through Essential Learning MHMRTC online course through Essential Learning MH Employees (3 years) Communicating with People who have MHMRTC online course through Disabilities Essential Learning MH Employees (3 years) Crisis MHMRTC online course through Management Essential Learning MH Employees (3 years) Cultural Issues in Mental Health MHMRTC online course through Treatment Essential Learning MH Employees (3 years) Guidelines for MHMRTC online course through Documentation Essential Learning MH Employees (3 years) Infection MHMRTC online course through Control Part 2 Essential Learning MH Employees (3 years) Overview of Severe Persistent MHMRTC online course through Mental Illness Essential Learning MH Employees (3 years) Recovery and Severe Persistent MHMRTC online course through Mental Illness Essential Learning MH Employees (3 years) Resilience and MHMRTC online course through SPMI Essential Learning SAMA Protection SAMA Assisting MHMRTC Training Center SAMA Protection SAMA Protection MHMRTC Training Center While all training is offered through the MHMRTC Training Center, Providers may take many of the required courses elsewhere. If the Provider elects to complete the training elsewhere, the Provider is responsible for the following: A) Ensuring the training meets the requirements set forth in the TAC codes B) Keeping a record of the training for each individual staff including but not limited to 1) The date of the training 2) The name and credentials of the person who provided the training 3) A roster of persons who attended the training 4) Materials that describe the content of the training 5) A certificate of course completion and an attestation of competency in course materials *MHMRTC Contract Monitoring department may request training records at any time for any staff to verify compliance with the Provider’s contract. Credentialing and Clinical Supervision All staff must complete credentialing process. LPHA and QMHP staff may not provide professional services until credentialed. Provider Qualifications All service providers must have a high school education (or GED), be 18 years of age, and not have been convicted of a crime relevant to a person’s duties including any sexual offense, drug-related offense, homicide, theft, assault, battery, or any crime involving personal injury or threat to another person. Provider 40 is required to provide external audit reports, if any, related to accreditation, licensure or certification. Programs must meet the requirements of those licenses, certifications or accreditations with regard to medication storage, handling, administration and documentation. Providers holding professional licenses and/or certifications must maintain those licenses and/or certifications in good standing with their respective licensing/certifying bodies. Credentialing LPHA -- Provider must submit an Application for Credentialing as MHMRTC Outpatient Provider form on each LPHA person. Local Authority will then credential these individuals. Licensed Practitioner of the Healing Arts (LPHA). An individual who is: a. a physician (M.D. or D.O.) licensed to practice medicine in Texas; b.a licensed or certified doctoral-level psychologist as defined in Texas Civil Statues §4495b; c. a licensed clinical social worker (LCSW)--as defined in the Human Resources Code, Chapter 50; or d.a licensed professional counselor (LPC) as defined in Texas Civil Statues §4512g e. a licensed Advanced Practice Nurse (APN) as defined in Title 22 TAC, Part II, Chapter 219; or f. a licensed marriage and family therapist (LMFT) as defined in Title 22 TAC, Chapter 801. QMHP - As there is no certification or credentialing process for QMHPs outside the MHMR system, Local Authority will credential all Provider staff at the QMHP level. Provider will submit an Application for Certification as MHMRTC QMHP and original college transcripts for persons wishing to serve as QMHPs to Local Authority as part of the credentialing process. QMHP-CS or qualified mental health professional-community services--A staff member who is credentialed as a QMHP-CS who has demonstrated and documented competency in the work to be performed and: (A) has a bachelor's degree from an accredited college or university with a minimum number of hours that is equivalent to a major (as determined by the LMHA or MCO in accordance with §412.316(d) of this title (relating to Competency and Credentialing)) in psychology, social work, medicine, nursing, rehabilitation, counseling, sociology, human growth and development, physician assistant, gerontology, special education, educational psychology, early childhood education, or early childhood intervention; (B) is a registered nurse; or (C) completes an alternative credentialing process identified by the department. CSSP or community services specialist--A staff member who, as of August 31, 2004: (A) received: (i) a high school diploma; or (ii) a high school equivalency certificate issued in accordance with the law of the issuing state; (B) had three continuous years of documented full-time experience in the provision of mental health rehabilitative services or case management services; and (C) demonstrated competency in the provision and documentation of mental health rehabilitative or case management services in accordance with Chapter 419, Subchapter L of this title (relating to Mental Health Rehabilitative Services) and Chapter 412, Subchapter I of this title (relating to Mental Health Case Management Services). 41 Clinical Supervision Provider is responsible for ensuring all Provider staff receive appropriate and needed clinical supervision. The requirements shown below are minimum requirements. It is expected that a staff needing additional supervision would receive it as necessary to ensure the quality of the services provided. Supervision meetings, training and chart reviews must be documented and available for review. (a) Clinical supervision for the QMHP, CSSP, FP or PP must be accomplished by an LPHA or a QMHP-CS as follows: (b) Clinical Supervision Requirement Summary: Supervision: 12 hours per year for each QMHP/CSSP, PP and FP; 4 of which must be one-on-one. The remaining 8 hours may be provided in a group format. Additional 12 hours per year for each PP and FP of in vivo observation. Training: Clinical supervisor participation; 4 hours/year, at least 1 hour in area of professional ethics and therapeutic boundaries. Clinical Chart review: 4 chart reviews per year (1 per quarter): First chart review must be submitted to the Credentialing Department within 90 days of QMHP/CSSP, PP or FP being hired. Subsequent chart reviews must be submitted to the Credentialing Department on a quarterly basis. (a) Licensed staff member supervision. All licensed staff members must be supervised in accordance with their practice act and applicable rules. (b) QMHP-CS supervision. A QMHP-CS's designated clinical duties must be clinically supervised by: (1) a QMHP-CS; or (2) an LPHA if the QMHP-CS is clinically supervising the provision of mental health community services. (c) CSSP supervision. A CSSP's designated clinical duties must be clinically supervised by a QMHP-CS. The CSSP must have access to clinical consultation with an LPHA when necessary. (d) Family partner supervision. A family partner is supervised by the mental health children's director, clinic director, case management supervisor, or wraparound supervisor. (e) Peer provider supervision. A peer provider's designated clinical duties must be clinically supervised by an LPHA. (f) Peer review. The LMHA, MCO, and provider must implement a peer review process for licensed staff members that: (1) promotes sound clinical practice; (2) promotes professional growth; and (3) complies with applicable state laws (e.g., Medical Practice Act, Nursing Practice Act, Vocational Nurse Act) and rules. (g) Documentation. All clinical supervision must be documented using the forms included with the QMHP application. 42 Medications Each Covered Individual’s medications (both prescription and over the counter) must be stored separately from other Covered Individuals’ medications. Medications for internal use must be stored separately from those intended for external use. A locked storage container must be available for medication storage and if a medication requires refrigeration, it must be separated from food in a clearly labeled, designated locked container. Avoid storing medication in locations with extreme heat, cold, or moisture. Prescription medications must be in the original container, labeled with the individual’s name, date, instructions, name of medication, dosage, and physician’s name. Programs which are licensed must meet the requirements of those licenses with regard to medication storage, handling, administration and documentation. For programs which are not licensed, medications may be administered only by persons licensed under state law to administer medication or in accordance with rules of the Board of Nurse Examiners that permit delegation of the administration of medication to unlicensed care givers. Programs which are not licensed but which supervise Covered Individuals who self-administer must minimally have staff trained in MHMRTC’s Supervising the Self-Administration of Medication classes, or equivalent, and provide on site verification of staff competency, by RN, Physician or pharmacist. Provider retains liability for handling, storage, and documentation of medications in its possession. It is recommended that Provider have a Consulting RN who performs medication counts (to verify accurate self-administration), verifies physician orders and verifies staff competency with regard to self-administration and documentation. In all training programs in which medications are administered or in which self-administration is supervised, a copy of the physician’s orders for all current medications must be kept in the Covered Individual’s record on site. Provider agrees to supply to the LMHA details of any New Generation medication prescriptions in order to track data for DSHS contractual requirements. 43 LA Quality Management/Contract Monitoring Medicaid Billing Audits Local Authority’s Billing Department will conduct quarterly billing audits of claims from the Provider. These audits will focus on the Provider’s compliance with Medicaid required documentation and record keeping. Providers are required to meet 100% compliance with the standards. Since audits will occur after Provider has billed Local Authority and been paid for services, any findings that services were not provided or documented within Medicaid Guidelines will result in recoupment for payment of such services from Provider by Local Authority who will return the funds to Medicaid. The Local Authority contact person for Medicaid Billing Department is Dave Farrell, Director of Client Accounting, 817 569- 4396 (See Attachment 2). Contract Monitoring Local Authority’s Quality Management Department will conduct a variety of reviews, including but not limited to: Site Assessments, Infection Control, Safety, and Environmental Reviews Clinically focused chart and program reviews Verification of required staff training Verification of credentialing of staff Verification of documentation of clinical supervision Special reviews based on complaints or other client related incidents The Local Authority contact person for Quality Management Reviews is: Tim Wells, MH Quality Management Manager, (817) 569-4458 44 Provider Quality Management Trends and Patterns Provider is required to have a mechanism or system in place to monitor the quality of the services provided. This includes a clinical review of records (separate from Clinical Supervision by an LPHA or QMHP) to determine any patterns or trends, implement corrective action or training and monitor for correction. Reports including this information must be provided to Local Authority at least quarterly. External Survey Reports If Provider is certified, accredited or licensed by any external agency (such as JCAHO), any findings from that external agency, relevant to the quality of services provided under this contract must be reported to Local Authority. Provider should send a copy or summary of the external report to Local Authority with documentation of corrective action required. Billing Audits Provider is required to audit minimally 10% of all claims submitted for payment prior to billing Local Authority. The following elements must be included in the audits: 1. Treatment Plan with goals and objectives for the client which must conform to the standards of the Mental Health Community Services Standards, Texas Administrative Code 412 G, section 412.322 Content and timeframe of treatment plan. Each provider must develop a written treatment plan, in consultation with the individual and their LAR (if applicable), within 10 business days after the date of receipt of notification from the department or its designee that the individual is eligible and has been authorized for routine care services. At minimum, a staff member credentialed as a QMHP-CS is responsible for completing and signing the treatment plan. The treatment plan must reflect input from each of the disciplines of treatment to be provided to the individual based upon the assessment. 2. Progress notes will conform to the following: (1) the name of the individual to whom the service was provided, including the LAR or primary caregiver, if applicable; (2) the type of service provided; (3) the date the service was provided; (4) the begin and end time of the service; (5) the location where the service was provided; (6) a summary of the activities that occurred; (7) the modality of the service provision (e.g., individual, group); (8) the method of service provision (e.g., face-to-face, phone, telemedicine); (9) the training methods used, if applicable (e.g., instructions, modeling, role play, feedback, repetition); (10) the title of the curriculum being used, if applicable; (11) the treatment plan objective(s) that was the focus of the service; (12) the progress or lack of progress in achieving treatment plan goals; (13) the signature of the staff member providing the service and a notation as to whether the staff member is an LPHA, a QMHP-CS, a pharmacist, a CSSP, an LVN, a peer provider or otherwise credentialed, as required for that service; and (14) any pertinent event or behavior relating to the individual's treatment which occurs during the provision of the service. In addition, a Medicaid members ID must be on all Medicaid billable progress notes. Results of audits must be provided to Local Authority. 45 Provider Profile MHMR of Tarrant County will collect and maintain information about each Provider’s performance. Such information is reviewed by the Quality Management Committee, the MH Community Advisory Committee, and the Network Advisory Committee and will include, but is not limited to: Number of individuals referred for services Number of individuals declined Numbers of individuals currently in services Number of confirmed abuse, neglect, or exploitation events Number of consumer complaints and percentage resolved in thirty (30) days Number of critical incidents (medication errors, serious injuries, etc.) Consumer satisfaction rating Percentage compliance with documentation, Medicaid billing standards, TDMHMR standards outcomes, and health/safety standards Provider profile information may be made available to Covered Individuals seeking services to assist them in choosing a provider. 46 Complaints Complaints from Covered Individuals Provider must inform Covered Individuals that they may file a complaint with MHMRTC regarding the Provider by calling: (817) 569-4429 or 1-888-636-6344 MHMR of Tarrant County will provide notepads to Provider containing this information. Covered Individuals may also call MHMR of Tarrant County with suspicions of rights violations, abuse, neglect or exploitation at (817) 569-4429. Covered Individuals may also call the Texas Department of Family and Protective Services Hotline at 1-800-252-5400 or www.txabusehotline.org. Complaints from Provider MHMR of Tarrant County desires a successful partnership with Provider to best serve the Covered Individuals. To this end, MHMRTC encourages Provider to call with concerns, problems and complaints regarding MHMRTC’s operations and interactions with Provider. Complaints should be directed to the Director of Contracts Management/Provider Relations at (817) 569-4456. Every effort will be made to address the issues involved. 47 Sanctions, Appeals and Contract Termination MHMR of Tarrant County will take punitive action for actions that pose a hazard to Covered Individuals or potentially violate Service guidelines. Sanctions a. b. c. d. e. f. MHMR of Tarrant County will impose sanctions if Provider does not maintain quality services in compliance with state and federal standards. Decisions regarding sanctions are reviewed by the Quality Management Committee. Notice of Default or Notice of Termination will be sent by certified mail to the Provider. Sanctions may include, but are not limited to: Immediate termination of contract Withholding of new referrals Withholding of outstanding payments, in whole or in part Request for recoupment of funds paid to Provider for services Fines, charge backs or offsets against future payments Suspension of contract and referral of existing Covered Individuals elsewhere, pending appeal Appeal Process If Provider wishes to appeal a decision by MHMR of Tarrant County to impose a sanction, Provider must notify the Director of Contracts Management/Provider Relations in writing within seven (7) days of receipt of a Notice of Default or Notice of Termination of the request for appeal. If Provider has additional information, not taken into consideration at the time the Sanction was imposed, documentation must be submitted with the request for appeal. Correspondence must be sent to: Kevin McClean, Director of Contracts Management/Provider Relations MHMR of Tarrant County P.O. Box 2603 Fort Worth, Texas 76113 Appeals of Sanctions will be reviewed by the Network Advisory Committee. Provider may be present at the meeting at which the appeal is discussed. Contract Termination If the contract is terminated, Provider is expected to cooperate with MHMRTC in the transfer of Covered Individuals to other providers. 48 References Texas Administrative Code: Rules of the Texas Department of Mental Health and Mental Retardation Title 25, Part II ........................................................... Relevant Rules Grid ........................................................... Chapter 404, Subchapter E………….Rights of Persons Receiving Mental Health Services ........................................................... Chapter 414, Subchapter A Client-Identifying Information ........................................................... Chapter 403, Subchapter B Charges for Community-Based Services Chapter 405, Subchapter K ............... Deaths of Persons Served by TDMHMR Facilities or Community Mental Health and Mental Retardation Centers (rev.6/95) Chapter 414, Subchapter L ................ Abuse, Neglect, and Exploitation in Local Authorities and Community Centers Chapter 411, Subchapter G ............... Community MHMR Centers Chapter 412, Subchapter C………….Charges for Community Services Chapter 412, Subchapter G ............... Mental Health Community Services Standards Chapter 412, Subchapter I…… ….…Mental Health Case Management Services Chapter 414, Subchapter K ............... Criminal History Clearances Chapter 419, Subchapter L………….Medicaid Rehabilitative Services 49 ATTACHMENT 1 ADDITIONAL FORMS NEW GEN MED TRACKING FORM 050710.pdf CLIENT NAME UPDATE FORM.pdf ...... CLIENT ADDRESS UPDATE FORM.pdf CLIENT REGISTRATION FORM.pdf 50 CLIENT DIAGNOSTIC TRACKING FORM.pdf MH ADULT UNIFORM ASSMENT FOR RDM.pdf ATTACHMENT 2 MEDICAID AUDIT CRITERION FOR REHABILITATION AND CARD SERVICES ITEM A Other 1 2 3 Com Stand 412.322(b) Rehab Rule 419.455 1 ( c) 1.4.10 Medicaid Provider Manual 1.4.10 Medicaid Provider Manual 412.322 (a) (2) 412.322 (d) (1)(A) 2 3 4 419.456 a 1 (A) 419.456, 419.465 (b) (2) (B) 1.4.10 Medicaid Provider Manual 1.4.10 Medicaid Provider Manual C 3 UNIFORM ASSESSMENT FOR RESILIENCY & DISEASE MANAGEMENT Adult & Children Obtain authorization from the department (DSHS) (doc in CMHC or WebCARE) Pending Review 23502499 Refund 2500-2900 2500 1015 1020 1025 2324 Services delivered must be within service package authorized. 2525 2540 Record documentation must be legible to others (other than author) 1060 Record must have Medicaid # and client's name on each page of significant documents, effective 11/1/99 1065 Medical Necessity 1 2 Client is an adult with severe and persistent mental illness or a child or adolescent with a serious emotional disturbance. MI documented covering the time services were rendered. Record documentation must be legible to others (other than author) Record must have Medicaid # and client's name on each page of significant documents, effective 11/1/99 B 1 DIAGNOSIS Trainin g Issue 10002310 1000 412.322 (c )(2) 419.455 (2) 419.453 (30) 1.4.10 Medicaid Provider Manual 1.4.10 Medicaid Provider Manual D Determination that there is a medical necessity for Medicaid MH rehabilitative services for the individual has been made by an LPHA. Medical necessity-evidenced by LPHA signature on the DMN form E-019 or the LOC-A printed from WebCARE. Record documentation must be legible to others (other than author) 1170 Record must have Medicaid # and client's name on each page of significant documents, effective 11/1/99 1180 2270 2570 2320 2620 1175 TREATMENT PLAN 1 412.322( e ) 419.456 a (2) 2 3 4 5 6 412.322( e )(1) 412.322 (e) (1) (A)-(G) 412.322 (e) (1) (A) 412.322 (e) (1) (B) 412.322 (e) (1) (C) 7 8 9 10 11 412.322 (e) (1) (D) 412.322 (e) (1) (E 412.322 (e) (1) (F) 412.322 (e) (1) (G) 412.32 419.465 (a) (3) 2 (e) (A) (1) Treatment plan (Present) developed within 10 day after authorization is 1220 obtained (TP signed within 10 days of LOC-A) At a minimum a staff member credentialed as a QMHP-CS must complete and sign the plan Description of A, B, C, D, E, F, G complete 1235 A description of the presenting problem section A 1235 A description of the individuals strengths C 1235 A description of the individuals needs arising from the mental illness section 1235 B/ E related needs A description of the /physical health issue/COPSD section G and F 1235 A description of the expected outcomes 1235 An expected date for recovery goals to be achieved 1235 List of resources for recovery ( last section of plan after signatures or brochure) 1235 List of types of services (services to be delivered must be checked or written 1245 out code or name of service) 51 2625 2344 2645 12 (H) 412.322 (e) (1) (H)(i) 13 412.322 (e) (1) (H)(ii) 14 15 412.322 (e) (1) (H)(iii) 412.322 (e) (2) (A) 16 412.322 (e) (2) (B) 17 18 19 20 412.322 (e) (2) (C ) 412.322 (e) (2)(D) 412.322 (e) (2)(E) 412.322 (e) (2) (A) 21 22 23 24 25 412.322 (e) (2) (B) 412.322 (e) (2) (C ) 412.322 (e) (2)(D) 412.322 (e) (2)(E) 412.322 (e) (3) 26 412.322 (f) (1) (A) 27 28 412.322 (f) (1) (B) 412.322 (f) (1) (C) 29 412.32 2 (f) (1) (D) 30 31 E 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 419.456 (d) (1) (A) 1.4.10 Medicaid Provider Manual 1.4.10 Medicaid Provider Manual 412.32 6 (2) 412.32 6 (9) 412.32 6 (8) 412.32 6(13) 412.32 6(13) 412.32 6 (6) 412.32 6 (7) 1250 Record documentation must be legible to others (other than author) 1345 Record must have Medicaid # and client's name on each page of significant documents, effective 11/1/99 1350 1255 1260 1265 1270 1275 1280 1285 1290 1300 1305 1310 1315 1320 1325 1330 1335 2530 2730 1340 PROGRESS NOTES MUST INCLUDE: Progress note present 2045 2345 2645 419.463 a (1) Client's name/ recipient 2050 2350 2650 419.463 (a) (4) Service date 2055 2355 2655 419.463 (a) (5) Duration (Stop/Start Time) 2060 2360 2660 419.463 (a) (6) Location/Setting 2065 2365 2665 419.465 (I) 419.463 a (2) Client present and awake Type of service provided is supported by sac used 2070 2075 2370 2375 2670 2675 419.463 (a) (3) 2080 2380 2680 419.465 (a) (1) The specific skill trained on and method used to provide the training is documented Service is face to face to individual or primary care giver of child adolescent 2085 2385 2685 419.463 (a) (7) Provider signature and date 2090 2390 2690 419.463 (a) (7) Credentials of provider 2095 2395 2695 A summary of the activities that occurred; 2100 2400 2700 The modality of service provision (i.e. one-to-one or group); 2105 2405 2705 The treatment plan goal's that was the focus of the service; and The treatment plan objective's that was the focus of the service listed on note or 2110 2111 2410 2710 1.4.10 Medicaid Provider Manual 412.32 6 (1) 412.32 6 (3) 412.32 6 (4) 412.32 6 (5) List of strategies to be implemented by staff to achieve goals (Strategy statement listed) The frequency, number of units, and duration of each service to be provided is present. The credentials of staff providing the service are present. Goals address individual s needs, preferences, experiences, and cultural background. Goals must address the individuals COPSD issue and or physical health disorder. Goals are expressed in overt, observable actions of the individual. Goals must be objective and measurable - using quantifiable criteria. Goals reflect individual autonomy, self direction, and desired outcomes. Objectives address individuals needs, preferences, experiences, and cultural background. Objectives address the individuals COPSD issue or physical health disorder. Objectives are expressed in overt, observable actions of the individual. Objectives are objective and measurable using quantifiable criteria. Objectives reflect individual autonomy, self direction, and desired outcomes. Copy of plan provided to the individual or explanation of reason why copy is not given. REVIEW Review plan prior to requesting authorization for the continuation of services. 3403 documented before 475/473 Review plan in its entirety, at least every 90 days. Determine if the plan is addressing needs of individual. Narrative comments by staff and client. Document progress on all goals and objectives and any recommendation for continuing services, change for services, discharge from services. Check box's marked. 419.463 (b) (4) (A) 419.463 (b) (4) (B) 419.463 (b) (4) © 412.326 (11) 52 16 412.326 (14) 17 412.32 6 (120 18 19 20 21 419.463 (b) (4) (D) 419.315 (d) 419.456 (a) (1) 412.326 (10) Agency Additionally 1 2 419.463 (b) (1) (A) 419.456 b (1) (A) 3 419.463 (b) (2) 4 419.459 (b) (3) 5 419.463 (b) (3) (A) 419.463 (b) (3) (B) 419.463 (b) (3) (C) 6 7 8 419.453 (16) 9 10 11 12 419.465 (2) (B) 14 15 16 17 18 19 20 21 22 23 25 26 27 28 29 416.456 (1) 419.465 (2) (A-D) A B C D 419.465 (a) (2) (A) 419.465 (a) (2) (B) 419.465 (a) (2) (C) 419.465 (a) (2) (D) 419.465 (a) (2) (E) 419.465 (a) (2) (G) 419.465 (2) (B) 1.4.10 Medicaid Provider Manual 1.4.10 Medicaid Provider Manual written out. Any pertinent event or behavior relating to the individuals treatment which occurs during the provision of service is documented within the note. Status/progress toward treatment Goals 2112 2115 2415 2715 2116 2117 2119 2125 2416 2716 2419 2719 2130 2425 2725 If the service is a crisis - Medical necessity must be determined within 2 business days after the provision of crisis services Medication Training & Support Services Applies to Children 2916 For medication training and support services and skills training and 2135 2435 development services, the name of the primary caregiver or LAR to whom the service was provided, if applicable; Medication Related/Psychosocial services must be provided by licensed 2140 2440 medical personnel ( Dr, PA, RN, LVN, pharmacist) Psychosocial rehabilitative coordination services Adult 2919 A description of the coordination service provided; 2145 2445 2730 If the service involves face-to-face or telephone contact, the person with whom the contact was made; and The outcome of the service. Service Provided was provided in excess of LOC-A The title of curriculum being used associated with rehab services only. Services are rounded off to 15 minutes Incorrect project code used/does not match srv described Additional Requirements by service type Crisis Services Adults 2913 Child 2914 The outcome of the individual's crisis; 2735 2740 2745 2150 2450 2750 2155 2455 2755 Non reimbursable activity If group service code, Adult group size must be more than 1 and less than 9 clients Children's groups 2 2760 staff up to 6 kids A Medicaid MH rehab service that is not auto's in accordance with 419.456 2770 Service code used is upcoding 2775 Service is a duplicate service 2780 Service is provided in excess of amount auth'd 2782 Department will not reimburse for more then: 2 hrs per day med training (2515,2516) 2785 4 hrs per day psychosocial rehab (2919) 2790 4 hrs per day rehab counseling/therapy (2921) 2795 4 hrs per day skills train/dev (2923, 2924) 2800 The cost of the following activities are included in the Medicaid MH rehabilitative services reimbursement rate(s) and may not be directly billed by the Medicaid provider: Developing and revising the treatment plan and interventions that are appropriate to an individual's 2805 needs (3403) Staffing and team meetings to discuss the provision of Medicaid MH rehabilitative services to a specific 2810 individual; Monitoring and evaluating outcomes of interventions, including contacts with a person other than the 2815 individual Documenting the provision of Medicaid MH rehabilitative services (44) 2820 A staff member traveling to and from a location to provide Medicaid MH rehabilitative services (7) 2825 Administering the uniform assessment (405,406) 2830 Services incidental to another service (project codes 11,12,16, 26) If group service code, group size must be more than 1 and less than 9 clients A Medicaid MH rehab service that is not auth'd in accordance with 419.4556 Record documentation must be legible to others (other than author) Record must have Medicaid # and client's name on each page of significant documents, effective 11/1/99 2835 2840 2850 53 2305 2310