Chapter 20: The Heart
advertisement

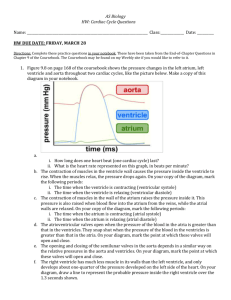
Chapter 20: The Heart Biol 141 A& P R.L. Brashear-Kaulfers How are the cardiovascular system and heart organized? Organization of the Cardiovascular System PLAY The Heart: Anatomy Figure 20–1 The Pulmonary Circuit • Carries blood to and from gas exchange surfaces of lungs The Systemic Circuit • Carries blood to and from the body Alternating Circuits • Blood alternates between pulmonary circuit and systemic circuit 3 Types of Blood Vessels • Arteries: – carry blood away from heart • Veins: – carry blood to heart • Capillaries: – networks between arteries and veins Capillaries • Also called exchange vessels • Exchange materials between blood and tissues • Dissolved gases, nutrients, wastes 4 Chambers of the Heart • 2 for each circuit: – left and right: ventricles and atria • Right atrium: – collects blood from systemic circuit • Right ventricle: – pumps blood to pulmonary circuit 4 Chambers of the Heart • Left atrium: – collects blood from pulmonary circuit • Left ventricle: – pumps blood to systemic circuit Anatomy of the Heart • Located directly behind sternum PLA Y Figure 20–2a Anatomy of the Heart • Great veins and arteries at the base • Pointed tip is apex Figure 20–2c Relation to Thoracic Cavity Surrounded by pericardial sac Between 2 pleural cavities In the mediastinum Figure 20–2b The Pericardium • Double lining of the pericardial cavity Figure 20–2c 2 Layers of Pericardium 1. Parietal pericardium: – – outer layer forms inner layer of pericardial sac 2. Visceral pericardium: – inner layer of pericardium Structures of Pericardium • Pericardial cavity: – Is between parietal and visceral layers – contains pericardial fluid • Pericardial sac: – fibrous tissue – surrounds and stabilizes heart Pericarditis An infection of the pericardium Superficial Anatomy of the Heart • 4 cardiac chambers • Atria - Thin-walled • Expandable outer auricle • Coronary sulcus: – divides atria and ventricles • Anterior and posterior interventricular sulci: – separate left and right ventricles – contain blood vessels of cardiac muscle Figure 20–3 The Heart Wall Figure 20–4 3 Layers of the Heart Wall • Epicardium:- outer layer • Visceral pericardium , Covers the heart • • • • Myocardium: middle layer, Muscular wall Concentric layers of cardiac muscle tissue Atrial myocardium wraps around great vessels 2 divisions of ventricular myocardium • Endocardium: inner layer Cardiac Muscle Cells Intercalated discs: interconnect cardiac muscle cells secured by desmosomes linked by gap junctions convey force of contraction propagate action potentials Figure 20–5 Characteristics of Cardiac Muscle Cells 1. Small size 2. Single, central nucleus 3. Branching interconnections between cells 4. Intercalated discs Cardiac Cells vs. Skeletal Fibers Table 20-1 What is the path of blood flow through the heart, and what are the major blood vessels, chambers, and heart valves? Internal Anatomy PLAY 3D Panorama of the Heart Figure 20–6a Atrioventricular (AV) Valves • Connect right atrium to right ventricle and left atrium to left ventricle • Permit blood flow in 1 direction: – atria to ventricles Septa – • Interatrial septum: – separates atria • Interventricular septum: – separates ventricles The Vena Cava • Delivers systemic circulation to right atrium • Superior vena cava: – receives blood from head, neck, upper limbs, and chest • Inferior vena cava: – receives blood from trunk, and viscera, lower limbs Coronary Sinus • Cardiac veins return blood to coronary sinus • Coronary sinus opens into right atrium Foramen Ovale • Before birth, is an opening through interatrial septum • Connects the 2 atria • Seals off at birth, forming fossa ovalis Cusps - Fibrous flaps that form bicuspid (2) and tricuspid (3) valvesPrevent valve from opening backward Right Atrioventricular (AV) Valve • Also called tricuspid valve • Opening from right atrium to right ventricle • Has 3 cusps • Prevents backflow The Pulmonary Circuit • Conus arteriosus (superior right ventricle) leads to pulmonary trunk • Pulmonary trunk divides into left and right pulmonary arteries • Blood flows from right ventricle to pulmonary trunk through pulmonary valve • Pulmonary valve has 3 semilunar cusps Return from Pulmonary Circuit • Blood gathers into left and right pulmonary veins • Pulmonary veins deliver to left atrium • Blood from left atrium passes to left ventricle through left atrioventricular (AV) valve • 2-cusp bicuspid valve or mitral valve The Left Ventricle • Holds same volume as right ventricle • Is larger; muscle is thicker, and more powerful • Similar internally to right ventricle, but does not have moderator band Systemic circulation: – blood leaves left ventricle through aortic valve into ascending aorta – ascending aorta turns (aortic arch) and becomes descending aorta Left and Right Ventricles • Have significant structural differences • Right ventricle wall is thinner, develops less pressure than left ventricle • Right ventricle is pouch-shaped, left ventricle is round Figure 20–7 The Heart Valves • One-way valves prevent backflow during contraction • (AV) Valves- between atria and ventricles • Blood pressure closes valve cusps during ventricular contraction • Papillary muscles tense chordae tendineae: – prevent valves from swinging into atria • Regurgitation -Failure of valves • Causes backflow of blood into atria Figure 20–8 Semilunar Valves • Pulmonary and aortic tricuspid valves • Prevent backflow from pulmonary trunk and aorta into ventricles • Have no muscular support • 3 cusps support like tripod • Aortic Sinuses - at base of ascending aorta • Prevent valve cusps from sticking to aorta • Origin of right and left coronary arteries Carditis - An inflammation of the heart • Can result in valvular heart disease (VHD): e.g., rheumatic fever KEY CONCEPT • The heart has 4 chambers: – 2 for pulmonary circuit: • right atrium and right ventricle – 2 for systemic circuit: • left atrium and left ventricle • Left ventricle has a greater workload • Is much more massive than right ventricle, but the two chambers pump equal amounts of blood • AV valves prevent backflow from ventricles into atria • Semilunar valves prevent backflow from aortic and pulmonary trunks into ventricles Connective Tissue Fibers of the Heart 1. Physically support cardiac muscle fibers 2. Distribute forces of contraction 3. Add strength and prevent overexpansion of heart 4. Elastic fibers return heart to original shape after contraction Blood Supply to the Heart • Coronary circulation Figure 20–9 Coronary Circulation • Coronary arteries-Left and right Originate at aortic sinuses • High blood pressure, elastic rebound force blood through coronary arteries between contractions • cardiac veins • Supplies blood to muscle tissue of heart Right Coronary Artery • Supplies blood to: – right atrium – portions of both ventricles – cells of sinoatrial (SA) and atrioventricular nodes – marginal arteries (surface of right ventricle) – posterior interventricular artery Left Coronary Artery • Supplies blood to: – left ventricle – left atrium – interventricular septum • 2 main branches: – circumflex artery – anterior interventricular artery Cardiac Veins • Great cardiac vein: – drains blood from area of anterior interventricular artery into coronary sinus • Anterior cardiac vein: – empties into right atrium • Posterior cardiac vein, middle cardiac vein, and small cardiac vein: – empty into great cardiac vein or coronary sinus The Cardiac Cycle The Heartbeat A single contraction of the heart The entire heart contracts in series: first the atria then the ventricles Figure 20–11 2 Types of Cardiac Muscle Cells • Conducting system: – controls and coordinates heartbeat • Contractile cells: – produce contractions * The Cardiac Cycle begins with action potential at SA node – transmitted through conducting system – produces action potentials in cardiac muscle cells (contractile cells) • Electrical events in the cardiac cycle can be recorded on an electrocardiogram (ECG) The Conducting System Figure 20–12 The Conducting System • A system of specialized cardiac muscle cells: – initiates and distributes electrical impulses that stimulate contraction • Automaticity: – cardiac muscle tissue contracts automatically Structures of the Conducting System • Sinoatrial (SA) node • Atrioventricular (AV) node • Conducting cells Conducting Cells • Interconnect SA and AV nodes • Distribute stimulus through myocardium • In the atrium: – internodal pathways • In the ventricles: – AV bundle and bundle branches Prepotential • Also called pacemaker potential • Resting potential of conducting cells: – gradually depolarizes toward threshold • SA node depolarizes first, establishing heart rate Heart Rate • SA node generates 80–100 action potentials per minute • Parasympathetic stimulation slows heart rate • AV node generates 40–60 action potentials per minute Impulse Conduction through the Heart Figure 20–13 The Sinoatrial (SA) Node • In posterior wall of right atrium • Contains pacemaker cells • Connected to AV node by internodal pathways • Begins atrial activation (Step 1) The Atrioventricular (AV) Node • • • • In floor of right atrium Receives impulse from SA node (Step 2) Delays impulse (Step 3) Atrial contraction begins The AV Bundle • In the septum • Carries impulse to left and right bundle branches: – which conduct to Purkinje fibers (Step 4) • And to the moderator band: – which conducts to papillary muscles 4. The Purkinje Fibers • Distribute impulse through ventricles (Step 5) • Atrial contraction is completed • Ventricular contraction begins Abnormal Pacemaker Function • Bradycardia: – abnormally slow heart rate • Tachycardia: – abnormally fast heart rate Ectopic Pacemaker: • • • • Abnormal cells Generate high rate of action potentials Bypass conducting system Disrupt ventricular contractions The Electrocardiogram Figure 20–14b Electrocardiogram (ECG or EKG) • A recording of electrical events in the heart • Obtained by electrodes at specific body locations • Abnormal patterns diagnose damage Features of an ECG : • P wave: atria depolarize • QRS complex: ventricles depolarize • T wave: ventricles repolarize Time Intervals • P–R interval: – from start of atrial depolarization – to start of QRS complex • Q–T interval: – from ventricular depolarization – to ventricular repolarization Cardiac Arrhythmias – Abnormal patterns of cardiac electrical activity KEY CONCEPT • Heart rate is normally established by cells of SA node • Rate can be modified by autonomic activity, hormones, and other factors • From the SA node, stimulus is conducted to AV node, AV bundle, bundle branches, and Purkinje fibers before reaching ventricular muscle cells • Electrical events associated with the heartbeat can be monitored in an electrocardiogram (ECG) What events take place during an action potential in cardiac muscle? Action Potentials in Skeletal and Cardiac Muscle Figure 20–15 Resting Potential • Of a ventricular cell: – about —90 mV • Of an atrial cell: – about —80 mV 3 Steps of Cardiac Action Potential 1. Rapid depolarization: – voltage-regulated sodium channels (fast channels) open 3 Steps of Cardiac Action Potential 2. As sodium channels close: – – – voltage-regulated calcium channels (slow channels) open balance Na+ ions pumped out hold membrane at 0 mV plateau 3 Steps of Cardiac Action Potential 3. Repolarization: – – – – plateau continues slow calcium channels close slow potassium channels open rapid repolarization restores resting potential The Refractory Periods • Absolute refractory period: – long – cardiac muscle cells cannot respond • Relative refractory period: – short – response depends on degree of stimulus Timing of Refractory Periods • Length of cardiac action potential in ventricular cell: – 250–300 msecs • 30 times longer than skeletal muscle fiber • long refractory period prevents summation and tetany Contraction of a cardiac muscle cell is produced by an increase in calcium ion concentration around myofibrils 1. 20% of calcium ions required for a contraction: – calcium ions enter cell membrane during plateau phase 2. Arrival of extracellular Ca2+: – triggers release of calcium ion reserves from sarcoplasmic reticulum Intracellular and Extracellular Calcium • As slow calcium channels close: – intracellular Ca2+ is absorbed by the SR – or pumped out of cell • Cardiac muscle tissue: – very sensitive to extracellular Ca2+ concentrations The Cardiac Cycle • The period between the start of 1 heartbeat and the beginning of the next • Includes both contraction and relaxation 2 Phases of the Cardiac Cycle: • Within any 1 chamber: – systole (contraction) – diastole (relaxation) Blood Pressure • In any chamber: – rises during systole – falls during diastole • Blood flows from high to low pressure: – controlled by timing of contractions – directed by one-way valves Phases of the Cardiac Cycle Figure 20–16 4 Phases of the Cardiac Cycle 1. 2. 3. 4. Atrial systole Atrial diastole Ventricular systole Ventricular diastole Cardiac Cycle and Heart Rate • At 75 beats per minute: – cardiac cycle lasts about 800 msecs • When heart rate increases: – all phases of cardiac cycle shorten, particularly diastole Pressure and Volume in the Cardiac Cycle • 8 steps in the cardiac cycle Figure 20–17 8 Steps in the Cardiac Cycle 1. Atrial systole: – – atrial contraction begins right and left AV valves are open 2. Atria eject blood into ventricles: – filling ventricles 3. Atrial systole ends: – – – AV valves close ventricles contain maximum volume end-diastolic volume (EDV) 4. Ventricular systole: – – – isovolemic ventricular contraction pressure in ventricles rises AV valves shut 8 Steps in the Cardiac Cycle 5. Ventricular ejection: – – semilunar valves open blood flows into pulmonary and aortic trunks • Stroke volume (SV) = 60% of end-diastolic volume 6. Ventricular pressure falls: – – semilunar valves close ventricles contain end-systolic volume (ESV), about 40% of end-diastolic volume 8 Steps in the Cardiac Cycle 7. Ventricular diastole: – – – ventricular pressure is higher than atrial pressure all heart valves are closed ventricles relax (isovolumetric relaxation) 8. Atrial pressure is higher than ventricular pressure: – – – – AV valves open passive atrial filling passive ventricular filling cardiac cycle ends Heart Failure • Lack of adequate blood flow to peripheral tissues and organs due to ventricular damage How do heart sounds relate to specific events in the cardiac cycle? Heart Sounds Figure 20–18b 4 Heart Sounds • S1: – loud sounds – produced by AV valves • S2: – loud sounds – produced by semilunar valves • S3, S4: – soft sounds – blood flow into ventricles and atrial contraction Positioning the Stethoscope • To detect sounds of each valve • Heart Murmur• Sounds produced by regurgitation through valves Figure 20–18a Aerobic Energy of Heart • From mitochondrial breakdown of fatty acids and glucose • Oxygen from circulating hemoglobin • Cardiac muscles store oxygen in myoglobin Stroke Volume • Volume (ml) of blood ejected per beat Figure 20–19 Cardiac Output • Cardiac output (CO) ml/min = • Heart rate (HR) beats/min • Stroke volume (SV) ml/beat Overview: Control of Cardiac Output Figure 20–20 (Navigator) Adjusting to Conditions • Cardiac output: – adjusted by changes in heart rate or stroke volume • Heart rate: – adjusted by autonomic nervous system or hormones • Stroke volume: – adjusted by changing EDV or ESV What variables influence heart rate? Autonomic Innervation Figure 20–21 (Navigator) Autonomic Pacemaker Regulation Figure 20–22 Autonomic Pacemaker Regulation • Sympathetic and parasympathetic stimulation: – greatest at SA node (heart rate) • Membrane potential of pacemaker cells:lower than other cardiac cells • Rate of spontaneous depolarization depends on: – resting membrane potential – rate of depolarization • ACh (parasympathetic stimulation): – slows the heart • NE (sympathetic stimulation): – speeds the heart Atrial Reflex • Also called Bainbridge reflex • Adjusts heart rate in response to venous return • Stretch receptors in right atrium: – trigger increase in heart rate – through increased sympathetic activity Hormonal Effects on Heart Rate • Increase heart rate (by sympathetic stimulation of SA node): – epinephrine (E) – norepinephrine (NE) – thyroid hormone What variables influence stroke volume? Factors Affecting Stroke Volume • Changes in EDV or ESV 2 Factors Affect EDV1. Filling time: duration of ventricular diastole 2. Venous return: rate of blood flow during ventricular diastole Figure 20–23 (Navigator) Preload • The degree of ventricular stretching during ventricular diastole • Directly proportional to EDV • Affects ability of muscle cells to produce tension EDV, Preload, and Stroke Volume • At rest: – EDV is low – myocardium stretches less – stroke volume is low • With exercise: – EDV increases – myocardium stretches more – stroke volume increases • As EDV increases, stroke volume increases Physical Limits • Ventricular expansion is limited by: – myocardial connective tissue – the fibrous skeleton – the pericardial sac End-Systolic Volume (ESV) • The amount of blood that remains in the ventricle at the end of ventricular systole is the ESV 3 Factors that Affect ESV 1. Preload: – ventricular stretching during diastole 2. Contractility: – force produced during contraction, at a given preload 3. Afterload: – tension the ventricle produces to open the semilunar valve and eject blood Contractility is affected by: autonomic activity & hormones : • Sympathetic stimulation: – NE released by postganglionic fibers of cardiac nerves – epinephrine and NE released by adrenal medullae – causes ventricles to contract with more force – increases ejection fraction and decreases ESV • Parasympathetic activity: – acetylcholine released by vagus nerves – reduces force of cardiac contractions Hormones and Contractility • Many hormones affect heart contraction • Pharmaceutical drugs mimic hormone actions: – stimulate or block beta receptors – affect calcium ions e.g., calcium channel blockers Afterload • Is increased by any factor that restricts arterial blood flow • As afterload increases, stroke volume decreases Factors Affecting Heart Rate and Stroke Volume Autonomic nervous system: sympathetic and parasymp athetic Circulating hormones Venous return and stretch receptors Figure 20–24 Stroke Volume Control Factors • EDV: – filling time – rate of venous return • ESV: – preload – contractility – Afterload Cardiac Reserve• The difference between resting and maximal cardiac output KEY CONCEPT • Cardiac output: – the amount of blood pumped by the left ventricle each minute – adjusted by the ANS in response to: • circulating hormones • changes in blood volume • alterations in venous return • Most healthy people can increase cardiac output by 300–500% The Heart and Cardiovascular System • Cardiovascular regulation: – ensures adequate circulation to body tissues • Cardiovascular centers: – control heart and peripheral blood vessels • Cardiovascular system responds to: – changing activity patterns – circulatory emergencies SUMMARY (1) • Organization of cardiovascular system: – pulmonary and systemic circuits • 3 types of blood vessels: – arteries, veins, and capillaries • 4 chambers of the heart: – left and right atria – left and right ventricles • Pericardium, mediastinum, and pericardial sac • Coronary sulcus and superficial anatomy of the heart • Structures and cells of the heart wall SUMMARY (2) • Internal anatomy and structures of the heart: – septa, muscles, and blood vessels • Valves of the heart and direction of blood flow • Connective tissues of the heart • Coronary blood supply • Contractile cells and the conducting system: – pacemaker calls, nodes, bundles, and Purkinje fibers SUMMARY (3) • Electrocardiogram and its wave forms • Refractory period of cardiac cells • Cardiac cycle: – atrial and ventricular – systole and diastole • Cardiodynamics: – stroke volume and cardiac output • Control of cardiac output