Disclosures
All relevant financial relationships with commercial interests reported by
faculty speakers, steering committee members, non-faculty content
contributors and/or reviewers, or their spouses/partners have been listed
in your program syllabus.
Off-label Discussion Disclosure
This educational activity may contain discussion of published and/or
investigational uses of agents that are not indicated by the Food and Drug
Administration. PCME does not recommend the use of any agent outside of
the labeled indications. Please refer to the official prescribing information
for each product for discussion of approved indications, contraindications
and warnings. The opinions expressed are those of the presenters and are
not to be construed as those of the publisher or grantors.
Educational Objectives
This program is designed to address the following IOM competencies:
provide patient-centered care and employ evidence-based practice. At the
conclusion of this activity, participants should be able to:
• Adopt ischemic risk assessment stratification strategies and
choose the best course of action to manage them
• Accurately diagnose and risk-stratify ACS patients who present
with atypical symptoms
• Make antiplatelet treatment choices based on an understanding of
the different efficacy/safety properties of available agents
• Identify institution and practice-specific lapses and inefficiencies
that increase the risk of recurrent events in ACS patients
Clinical Management of Chest Pain Syndrome
Key Considerations
• Need for differential diagnosis of the spectrum of ACS
• Fundamental aspects of management of acute chest pain
– Elements for optimal early hospital care
• The importance of risk stratification to guide practice decisions
– Options: initial conservative or invasive strategy
– If invasive strategy, rationale for early catheterization
• The expanded field of existing antiplatelet treatment options
– Clopidogrel, prasugrel, ticagrelor
• Emerging antiplatelet/anticoagulant therapies for ACS
– Strong contender: very low dose rivaroxaban
• The need to balance anti-ischemic effects vs bleeding risk
• The growing importance of quality outcomes in ACS
CHEST PAIN CASE
Chest Pain Case
Initial Presentation
• 68-year-old female presents to the Emergency Department at
8:45 am
• Substernal and epigastric discomfort radiating to left shoulder for
two hours; onset was with exertion but continued at rest
• ECG shows prominent ST-segment depression in the lateral
precordial leads (V5, V6)
• Initial troponin-I is 0.02 mg/dL (normal, <0.04)
• CVD History: Suspected CAD with abnormal stress test, but
declined catheterization one year ago; treated with beta-blockers,
aspirin, prn nitroglycerin (has not used).
• Additional Medical History: Significant for positive family history, mild
hypertension, and mild dyslipidemia.
Chest Pain Case
Initial ECG
Chest Pain Case
Diagnosis, Prognosis, and Treatment Stratification Issues
• Which diagnosis: Non-cardiac? UA? NSTEMI? STEMI?
• Risk category: Low? Intermediate? High? (TIMI, GRACE)
• Choice of management strategy for next 24h depends at least in part
on answers to above questions.
• Repeat troponin assay 2 hours later is positive, and patient’s
diagnosis is changed from UA to NSTEMI
• Invasive or conservative strategy?
• Once decided, medical therapy that supports the chosen strategy
should be initiated: Anticoagulant? Which one? What dose?
Oral antiplatelet (beyond aspirin)? Which one? What dose?
GP IIb/IIIa antagonist? Small or large molecule? What dose?
Beta blocker? IV or PO?
Chest Pain Case
Initial Evaluation
• Plan is to take her to cath lab as first case tomorrow morning
if she remains stable and pain free
• What would you choose for anticoagulation, antiplatelet, and
beta-blocker therapy (patient’s creatinine clearance is 45
ml/min)?
• What therapy might you add (or change) in the cath lab?
CLINICAL SPECTRUM
AND PRESENTATION
Hospitalizations in the US Due to ACS
Acute Coronary Syndromes*
1.57 Million Hospital Admissions – ACS
UA/NSTEMI†
STEMI
1.24 million
0.33 million
Admissions per year
Admissions per year
*Primary and secondary diagnoses. †About 0.57 million NSTEMI and 0.67 million UA.
Heart Disease and Stroke Statistics – 2007 Update. Circulation. 2007;115:69-171.
Acute Coronary Syndrome Spectrum
Pathophysiology and Clinical Evaluation
Presentation
Working Dx
ECG
No ST Elevation
Cardiac
Biomarker
NST E-ACS
UA
NSTEMI
Final Dx
Unstable
Angina
ST Elevation
Myocardial Infarction
NQMI
Qw MI
Libby P. Circulation. 2001;104:365. Hamm CW, Bertrand M, Braunwald E. Lancet. 2001;358:1533-1538.
Davies MJ. Heart. 2000;83:361-366. Anderson JL et al. J Am Coll Cardiol. 2007;50:e1-e157, Figure 1. Reprinted with permission.
Acute Chest Pain Presentation
Classifications
Acute Coronary Syndromes
TIMI flow grade 2/3
in culprit artery
TIMI flow grade 0/1
in culprit artery
- Troponin
+ Troponin
+ Troponin
Unstable
angina
NSTEMI
STEMI
Gibson CM et al. Presented at: 2008 AHA Scientific Sessions. New Orleans, LA.
SYMPTOMS SUGGESTIVE OF ACS
Noncardiac Diagnosis
Chronic Stable Angina
Treatment as indicated
by alternative diagnosis
ACC/AHA Chronic Stable
Angina Guidelines
Definite ACS
Possible ACS
No ST-Elevation
Nondiagnostic ECG
Normal initial serum
cardiac biomarkers
ST-Elevation
ST and/or T wave changes
Ongoing pain
Positive cardiac biomarkers
Hemodynamic abnormalities
Observe
≥12 h from symptom onset
No recurrent pain; negative follow-up
studies
Recurrent ischemic pain or positive
follow-up studies
Evaluate for
reperfusion therapy
Diagnosis of ACS confirmed
Stress study to provoke ischemia
ACC/AHA STEMI
Guidelines
Consider evaluation of LV function if ischemia is
present (tests may be performed either prior to
discharge or as outpatient)
Negative
Positive
Admit to hospital
Potential diagnoses: nonischemic
discomfort; low-risk ACS
Diagnosis of ACS confirmed or
highly likely
Manage via acute ischemia pathway
Arrangements for outpatient follow-up
Algorithm for evaluation and management of patients suspected of having ACS.
Anderson JL et al. J Am Coll Cardiol. 2007;50:e1-e157, Figure 2.
Acute Coronary Syndromes
• Common Features of ACS
– Similar pathophysiology
– Similar presentation and early management rules
• Differentiating Features of ACS
–
Unstable Angina
Non-occlusive thrombus
No diagnostic ECG changes, but
ischemic ST-T changes confer
higher risk
Normal cardiac biomarkers
–
NSTEMI
Occluding thrombus sufficient to
cause myocardial damage
No diagnostic ECG changes, but
ischemic ST-T changes: higher risk
Elevated cardiac biomarkers
–
STEMI
Complete thrombus occlusion
ST elevation or new LBBB
Elevated cardiac biomarkers
More severe symptoms
Third Universal Definition of MI
•
•
•
•
Type I: Spontaneous MI (coronary occlusion)
Type 2: MI due to ischemic (supply/demand) imbalance
Type 3: MI causing death w/o biomarkers/ECGs (SCD)
Type 4a: MI related to PCI (cTn >5 x 99%ile URL, or >20%↑
from elevated baseline, & + Sx, ECG, or angiography)
• Type 4b: MI related to stent thrombosis (detected by angio
or autopsy and with cTn rise &/or fall)
• Type 5: MI related to CABG (cTn >10 x 99%ile URL from
normal baseline, & + ECG, angiography, or imaging
evidence of MI)
Thygesen K et al. Circulation. 2012;126:2020-2035.
Non-ACS Causes of Elevated Troponin
•
•
•
•
•
•
•
•
•
•
Heart failure
Shock: septic, hypovolemic, cardiogenic
Injury: cardiac contusion, surgery, ablation, shocks
Inflammation: myocarditis, pericarditis
Cardiomyopathies: infiltrative, stress, hypertensive,
hypertrophic
Aortic dissection, severe aortic stenosis
Tachycardias
Pulmonary: embolism/hypertension, respiratory failure
Neurologic: stroke, intracranial hemorrhage
Renal failure
Mortality in Acute Coronary Syndromes
Death from Hospital Admission to 6 Months
% Mortality
16
12
STEMI
8
NSTEMI
UA
4
0
0
30
60
90
120
150
180
Days
Fox KA et al. BMJ. 2006;333:1091.
GRACE n=43,810
RISK STRATIFICATION AND
EMERGENT HOSPITAL CARE
“Dynamic Risk Stratification” Tools
• History and physical
• Standard ECG and non-standard ECG leads
– 15-lead ECGs should perhaps become “standard” in all but very-low-risk patients
• Biomarkers
– Troponins I and T, CK-MB
– High-sensitivity troponin
– Brain natriuretic peptide (BNP)
• Non-invasive imaging
– Echocardiogram
– Stress testing
– Technetium-99m-sestamibi
• Invasive imaging
– Cardiac computed tomography angiography (CCTA)
• Predictive indices/schemes
– Better as research tools than for real-time clinical decision-making
Chest Pain Syndrome Suggestive of Ischemia
Immediate Assessment within 10 Minutes
Initial Labs
and Tests
Emergent
Care
• 12 lead ECG
• IV access
• Obtain initial cardiac
biomarkers
• Cardiac
monitoring
• Electrolytes, CBC
lipids, BUN/
creatinine, glucose,
coags
• Oxygen
• Chest x-ray
• Nitrates
• Aspirin
History &
Physical
• Establish
diagnosis
• Read ECG
• Identify
complications
• Assess for
reperfusion
Risk Scores
History
Presentation
TIMI
GRACE
Age
Hypertension
Diabetes
Smoking
↑ Cholesterol
Family history
History of CAD
Severe angina
Aspirin within 7 days
Elevated markers
ST-segment deviation
Age
Heart rate
Systolic BP
Elevated creatinine
Heart failure
Cardiac arrest
Elevated markers
ST-segment deviation
GRACE = Global Registry of Acute Coronary Events; TIMI = Thrombolysis in Myocardial Infarction
Antman EM et al. JAMA. 2000;284:835-842. Eagle KA et al. JAMA. 2004;291:2727-2733.
TIMI Risk Score
All-Cause Mortality, New or Recurrent MI, or Severe Recurrent Ischemia
Requiring Urgent Revascularization Through 14 Days After Randomization
0.45
40.9%
0.4
0.35
0.3
26.2%
0.25
19.9%
0.2
13.2%
0.15
0.1
0.05
4.7%
8.3%
0
0-1
2
3
4
5
TIMI Risk Score
6-7
TIMI = Thrombolysis in Myocardial Infarction
Reprinted with permission from Antman EM et al. JAMA. 2000;284:835-842. Copyright © 2000, American Medical Association. All
Rights reserved. The TIMI risk calculator is available at www.timi.org.
Anderson JL et al. J Am Coll Cardiol. 2007;50:e1-e157, Table 8.
Troponin Levels Predict Risk of Mortality
in UA/NSTEMI
7.5 %
Mortality at 42 days; % of patients
8
7
6.0 %
6
5
4
3
2
1
0
1.0 %
831
0 to <0.4
3.4 %
3.7 %
148
134
1.7 %
174
50
0.4 to <1.0 1.0 to <2.0 2.0 to <5.0 5.0 to <9.0
Cardiac troponin I (ng/mL)
Antman EM et al. N Engl J Med. 1996;335:1342-1949.
67
≥ 9.0
EARLY HOSPITAL CARE
Optimal Upstream Management after
Ischemic Risk Assessment
• Basis for assessment
– “Pain story”
– Background CVD risk
– ECG
– Troponin elevation in pertinent time frame
– Predictive risk score
• Options
– Antiplatelet therapy increasingly important as ischemic risk
increases
– UFH and enoxaparin established
– Bivalirudin and fondaparinux: New options that are
non-inferior
Current Medical Management of
Unstable Angina and NSTEMI
Acute Therapy
Maintenance Therapy
• Oxygen, bed rest
• Antiplatelet therapy
• ECG monitoring
• Beta blockers
• Nitroglycerin
• Calcium channel blockers
• Beta blockers
• Lipid-lowering agents
• ACE inhibitors
• ACE inhibitors
• Antiplatelet therapy
• Oral anticoagulant therapy
• Anticoagulant therapy
Braunwald E et al. Available at: www.acc.org.
ACUTE CORONARY SYNDROME
Patient Management Considerations:
Initial Conservative or Invasive Strategy –
Based on Risk Assessment
Early Invasive vs Initial Conservative Strategy
General Considerations in UA/NSTEMI
•
•
•
•
•
•
•
•
•
•
•
•
EARLY INVASIVE STRATEGY
GENERALLY PREFERRED
Recurrent angina or ischemia at rest or with lowlevel activities despite intensive medical therapy
Elevated cardiac biomarkers (TnT or TnI)
New or presumably new ST-depression
Signs or symptoms of heart failure
Hemodynamic instability
High risk score (e.g. GRACE, TIMI)
Sustained ventricular tachycardia
PCI within 6 months
Prior CABG
Diabetes mellitus
Mild to moderate renal dysfunction
Reduced LV function (LVEF <40%)
•
•
•
•
•
INITIAL CONSERVATIVE STRATEGY
GENERALLY PREFERRED OR REASONABLE
Low risk score (e.g. GRACE, TIMI)
Absence of high-risk features
High risk for catheterization-related complications
Patient not a revascularization candidate (with
either PCI or CABG)
Patient prefers conservative therapy
CABG = coronary artery bypass graft surgery; GRACE = Global Registry of Acute Coronary Events;
LV = left ventricular; LVEF = left ventricular ejection fraction; PCI = percutaneous coronary intervention;
TIMI = Thrombolysis in Myocardial Infarction; TnI = troponin I; TnT = troponin T
Source: ACC/AHA 2011 UA/NSTEMI guidelines.
Levine GN et al. Circulation. 2011;124:e574-e651. Wright RS et al. Circulation. 2011;123:2022-2060.
Conservative Therapy Option for UA/NSTEMI
Early Revascularization or PCI Not Planned
• Antiplatelet therapy
– Aspirin
– Clopidogrel or ticagrelor
• MONA + BAA (enoxaparin, fondaparinux preferred over UFH)
– Morphine, Oxygen, Nitroglycerin, Aspirin + Beta blocker, ACEI,
Anticoagulant (morphine has only Class IIa recommendation due to increased
mortality risk – CRUSADE)
• Glycoprotein IIb/IIIa inhibitors
– Only in certain circumstances
• Planning PCI, elevated troponin
• Surveillance in hospital
– Serial ECGs
– Serial cardiac markers
Anderson JL et al. Circulation. 2007;116:e148-e304.
Invasive Therapy Option for UA/NSTEMI
• Coronary angiography and revascularization within 12 to 48
hours after presentation to ED
• For high-risk ACS
– MONA + BAA (UFH or bivalirudin or enoxaparin)
– Morphine, Oxygen, Nitroglycerin, Aspirin + Beta blocker, ACEI,
Anticoagulant (morphine has only Class IIa recommendation due to increased
mortality risk – CRUSADE)
– Antiplatelet therapy
Aspirin; P2Y12 inhibitor (clopidogrel or ticagrelor or prasugrel) or GPI
Reduction in death/MI/stent thrombosis
PCI + BMS: at least 1 year (may stop earlier if needed)
PCI + DES: at least 1 year
Anderson JL et al. Circulation. 2007;116:e148-e304.
ACCF/AHA Guidelines 2011 Focused Update
Early Invasive Strategies
I
IIa
IIb
III
High-risk patients with:
- Refractory ischemia
-
Wright RS et al. Circulation. 2011;123:2022-2060.
Recurrent angina/ischemia
Elevated cardiac biomarkers (T)
New ST-segment depression
New CHF or worsening MR
High-risk on non-invasive testing
LV dysfunction (EF <40%)
Hemodynamic instability
Sustained VT
Diabetics with single-vessel disease
Mild to moderate kidney disease
PCI within 6 months, prior CABG high-risk score
Not in low-risk women
TACTICS: Primary Endpoint
Death, MI, Rehospitalized for ACS at 6 Months
19.4%
20
15.9%
% Patients
16
12
O.R 0.78
95% CI (0.62, 0.97)
P=0.025
8
4
Conservative:
Invasive:
0
0
1
2
Cannon CP et al. N Engl J Med. 2001;344:1879-1887.
3
4
Time (months)
5
6
Meta-analysis: Mortality in NSTE-ACS by Strategy
Study
Deaths, n
Invasive
FRISC-II
45
67
24
TRUCS
3
9
12
TIMI-18
37
39
6
VINO
2
9
6
RITA-3
102
132
60
ISAR-COOL
0
3
1
ICTUS
15
15
12
Overall RR (95% CI)
0.75 (0.63-0.90)
0.1
Favors
Early Invasive
Therapy
Bavry AA et al. J Am Coll Cardiol. 2006;48:1319-1325.
1
10
Favors
Conservative
Therapy
Follow-up
Conservative Months
TIMACS
Rates of death, MI, or stroke within 6 months according to GRACE
risk level and HR (95% CI), early vs delayed invasive strategy
EARLY (%) DELAYED (%)
HR (95% CI)
P
Low/Intermediate (n=2070)
7.6
6.7
1.12 (0.88–1.56)
0.48
High (n=961)
13.9
21.0
0.65 (0.48–0.89)
0.006
*Low/intermediate risk=GRACE score <140
High risk=GRACE score ≥140
Mehta SR et al. N Engl J Med. 2009;310:2165-2175.
FREEDOM: PCI vs CABG in Diabetics* with MVD
*31% w/ UA
Farkouh ME et al. N Engl J Med. 2012;367:2375-2384.
ANTICOAGULANT THERAPY IN ACS
Coagulation Pathways and Anticoagulant
Therapy in ACS
Weitz et al. Chest. 2001;119:95S-107S.
ACC/AHA UA/NSTEMI 2011 Guidelines
Initial Anticoagulant Algorithm by Strategy
Diagnosis of UA/NSTEMI likely/definite ASA (IA); clopidogrel if ASA intolerant (IA)
SELECT MANAGEMENT STRATEGY
INVASIVE STRATEGY†
Initiate anticoagulant therapy (IA)
Acceptable options:
enoxaparin or UFH (IA)
or bivalirudin (IB)*
CONSERVATIVE STRATEGY
Initiate anticoagulant therapy (IA)
Acceptable options: enoxaparin or UFH (IA)
or fondaparinux (IB), but enoxaparin or
fondaparinux are preferred (IIa:B)
*If fondaparinux is used (IB), it must be co-administered with another anticoagulant with factor IIa activity;
for example, unfractionated heparin. should not be the sole anticoagulant to support PCI (IIIC).
† Timing of invasive strategy generally is assumed to be 4 to 48 hours. If immediate angiography is
selected, see STEMI guidelines.
Jneid H, Anderson JL et-al. Circulation. 2012;126:875-910.
ANTIPLATELET THERAPY IN ACS
Platelet Aggregation and Mechanisms of Action
of Antiplatelet Therapies
ADP
clopidogrel
prasugrel
dipyridamole
ADP
phosphodiesterase
ticagrelor
ADP
cAMP
IIb/IIIa inhibitors
Activation
COX
Gp IIb/IIIa
(Aggregation)
TXA2
aspirin
ADP = adenosine diphosphate; TXA2 = thromboxane A2; COX = cyclooxygenase
Adapted from Schafer AI. Am J Med. 1996;101:199-209.
Collagen
Thrombin
TXA2
Heparins
CURE Study
Primary End Point: MI/Stroke/CV Death
Cumulative Hazard Rate
0.14
20%
Relative
Risk
Reduction
Placebo
+ Aspirin
(n=6303)
0.12
0.10
0.08
Clopidogrel
+ Aspirin
(n=6259)
0.06
0.04
P<0.001
n=12,562
0.02
0.00
0
3
6
Months of Follow-up
Yusuf S et al. N Engl J Med. 2001;345:494-502.
9
12
PCI-CURE
Clopidogrel for PCI after NSTE-ACS
Composite of MI or cardiovascular death from randomization to end follow-up
0.15
12.6%
Cumulative Hazard Rate
Placebo
+ ASA*
31%
0.10
8.8%
Clopidogrel
+ ASA*
0.05
P = 0.002
n = 2658
0.0
0
100
200
Days of follow-up
* In addition to other standard therapies.
Mehta SR et al for the CURE Investigators. Lancet. 2001;358:527-533.
300
400
Overall
Relative Risk
Reduction
CURRENT: Clopidogrel Double vs Standard Dose
Primary Outcome: PCI Patients
CV Death, MI or Stroke
0.04
Clopidogrel Standard
15% RRR
0.03
0.02
HR 0.85
95% CI 0.74-0.99
P=0.036
0.0
0.01
Cumulative Hazard
Clopidogrel Double
0
3
6
9
12
15
Days
18
Mehta SR et al. Presented at: European Society of Cardiology, September, 2009.
21
24
27
30
CURRENT: Clopidogrel Double vs Standard Dose
0.008
Clopidogrel Standard Dose
46%
RRR
0.004
Clopidogrel Double Dose
HR 0.54
95% CI 0.39-0.74
P=0.0001
0.0
Cumulative Hazard
0.012
Definite Stent Thrombosis
0
3
6
9
CURRENT-OASIS 7. Lancet. 2010;376:1233-1243.
12
15
Days
18
21
24
27
30
TRITON – TIMI 38
CV Death, MI, Stroke
15
Primary Endpoint (%)
Clopidogrel
12.1
(781)
9.9
(643)
10
Prasugrel
HR 0.80
P=0.0003
5
0
HR 0.81
(0.73-0.90)
P=0.0004
NNT= 46
HR 0.77
P=0.0001
ITT= 13,608
0
30 60 90
Wiviott SD et al. N Engl J Med. 2007;357:2001-2005.
180
270
Days
LTFU = 14 (0.1%)
360
450
TRITON-TIMI 38 Study: Subgroups
Primary endpoint = first occurrence of CV death, MI, or stroke
Females
Males
320
883
Prasugrel
(%)
13.6
9.7
Age <75
Age 75
979
224
9.3
17.2
13.0
28.0
No Hx of DM
Hx of DM
856
347
10.6
11.7
11.0
27.0
UA/NSTEMI
STEMI
893
390
12.1
9.0
15.2
17.1
BMS only
DES
571
560
10.7
11.3
17.0
13.7
CrCl 60
CrCI <60
1013
176
8.4
26.2
12.3
31.7
n
Hazard Ratio
0.2
Murphy SA et al. Eur Heart J. 2008;29:2473-2479.
1
Prasugrel
better
5
Clopidogrel
better
Clopidogrel
(%)
20.5
13.6
TRITON-TIMI 38
Efficacy and Safety in the Diabetic Subgroup
18
n=3146
16
17.0
CV Death/MI/Stroke
14
Endpoint (%)
Clopidogrel
12
Prasugrel
10
12.2
HR=0.70
P<0.001
NNT=46
8
6
4
TIMI Major
Non-CABG Bleeds
2
0
Clopidogrel
2.6
2.5
Prasugrel
0
30 60 90
Wiviott SD et al. Circulation. 2008;118:1626-1636.
180
270
Time (Days)
360
450
TRITON-TIMI 38
Net Clinical Benefit Bleeding Risk Subgroups
POST HOC ANALYSIS
Prior
Stroke / TIA
Age
Wgt
Risk (%)
Yes
+ 37
No
Pint = .006
-1
≥75
-16
Pint = .18
<75
<60 kg
+3
≥60 kg
Pint = .36
-14
-13
OVERALL
0.5
-16
Prasugrel Better
Wiviott SD et al. N Engl J Med. 2007;357:2001-2015.
1
HR
Clopidogrel Better
2
Ticagrelor (AZD 6140)
An Oral Reversible P2Y12 antagonist
HO
N
N
N
H
N
HO
O
N
F
N
S
Ticagrelor is a
cyclo-pentyl-triazolo-pyrimidine (CPTP)
F
OH
• Direct acting
– Not a prodrug; does not require metabolic activation
– Rapid onset of inhibitory effect on the P2Y12 receptor
– Greater inhibition of platelet aggregation than clopidogrel
• Reversibly bound
– Degree of inhibition reflects plasma concentration
– Faster offset of effect than clopidogrel
– Functional recovery of all circulating platelets
PLATO: Kaplan-Meier Estimate of Time to First Primary
Cumulative incidence (%)
Efficacy Event (Composite of CV Death, MI, or Stroke)
13
12
11
10
9
8
7
6
5
4
3
2
1
0
9.8
Ticagrelor
HR = hazard ratio
CI = confidence interval
HR 0.84 (95% CI 0.77–0.92), P=0.0003
0
No. at risk
Ticagrelor
Clopidogrel
11.7
Clopidogrel
60
120
180
240
300
360
5,161
5,096
4,147
4,047
Days after randomisation
9,333
9,291
8,628
8,521
Wallentin L et al. N Engl J Med. 2009;361:1045-1057.
8,460
8,362
8,219
8,124
6,743
6,743
Stent Thrombosis
Evaluated in Patients with Any Stent During the Study
Ticagrelor
(n=5,640)
Clopidogrel
(n=5,649)
HR
(95% CI)
Definite
71 (1.3)
106 (1.9)
Probable or definite
118 (2.1)
155 (2.8)
158 (2.8)
0.67 (0.50–0.91)
0.75 (0.59–0.95)
0.77 (0.62–0.95)
P value
Stent thrombosis, n (%)
Possible, probable, definite
202 (3.6)
*Time-at-risk is calculated from first stent insertion in the study or date of randomization
Wallentin L et al. N Engl J Med. 2009;361:1045-1057.
0.009
0.02
0.01
Ticagrelor Interaction with Aspirin Dose
Hazard Ratio Compared with Clopidogrel
Aspirin Dose (mg/day)
Hazard Ratio
95% CI
≥300
1.45
1.01 – 2.09
>100 – <300
0.99
0.70 – 1.40
≤100
0.77
0.69 – 0.86
WARNING: ASPIRIN DOSE AND TICAGRELOR EFFECTIVENESS
Maintenance doses of aspirin above 100mg reduce the effectiveness of
ticagrelor and should be avoided. After any initial dose, use with aspirin
75-100 mg per day. (FDA-approved prescribing information, July 2011)
Wallentin L et al. N Engl J Med. 2009;361:1045-1057.
Highlights of P2Y12 Inhibitor Trials
• Clopidogrel
– Double-dose (600 mg load, 150 mg qd x 1 week) in setting of PCI decreases
non-fatal MI and stent thrombosis
– Preferred P2Y12 inhibitor in patients with h/o TIA/stroke
• Prasugrel
–
–
–
–
–
Ischemic events c/w clopidogrel, both early & late, c/w clopidogrel
Stent thrombosis c/w clopidogrel
Especially large benefit in diabetics and in STEMI
Not superior to clopidogrel in medically managed patients
Contraindicated in patients with h/o TIA/stroke
• Ticagrelor
– Ischemic events c/w clopidogrel, both early & late, both with invasive and
conservative management, c/w clopidogrel
– Stent thrombosis c/w clopidogrel
– CV mortality c/w clopidogrel, including with CABG
ACC/AHA UA/NSTEMI 2012 Guidelines
Initial Antiplatelet Algorithm by Strategy
Diagnosis of UA/NSTEMI likely/definite ASA (IA); clopidogrel if ASA intolerant (IA)
SELECT MANAGEMENT STRATEGY
INVASIVE STRATEGY†
Initiate anticoagulant therapy (IA)
Pre-cath: add a 2nd antiplatelet agent (IA):
clopidogrel (IB) or ticagrelor (IB) or a GPI (IA)
(eptifibatide or tirofiban preferred: LOE-B)
If PCI: clopidogrel (IA) or ticagrelor (IB) if not begun
pre-cath; or prasugrel (IB); or (selectively) a GPI (IA)
If CABG: Maintenance ASA (IA)
If Med Rx: clopidogrel or ticagrelor (IB)
Jneid H, Anderson JL et-al. Circulation. 2012;126:875-910.
CONSERVATIVE STRATEGY
Initiate anticoagulant therapy (IA)
Initiate clopidogrel (IB)
or ticagrelor (IB)
Oral Antiplatelet Therapy
I IIa IIb III
Patients should be counseled on the need for
and risk of dual antiplatelet therapy (DAPT)
before placement of intracoronary stents,
especially a DES, and alternative therapies
should be pursued if they are unwilling or
unable to comply with the recommended
duration of DAPT.
2011 ACCF/AHA PCI Guidelines
Early Discontinuation of Antiplatelet Therapy is
An Important Risk Factor for Stent Thrombosis
Incidence of ST (%)
30
Overall ST=1.3%
(P=0.09, n=2229)
29.0
20
8.7
10
0
6.2
2.5
3.3
3.6
1.4
2.0
UA
Thrombus
Diabetes
Unprotected
Left Main
Bifurcation
Lesion
ST = stent thrombosis
Iakovou I et al. JAMA. 2005;293:2126-2130.
Renal
Failure
Prior
Brachytherapy
Premature
Antiplatelet
Discontinuation
Post-procedural Antiplatelet Therapy
I IIa IIb III
After PCI, aspirin should be continued indefinitely.
I IIa IIb III
The duration of P2Y12 inhibitor therapy after stent
implantation should generally be as follows:
a) In patients receiving a stent (BMS or DES)
during PCI for ACS, P2Y12 inhibitor therapy should
be given for at least 12 months. Options include:
clopidogrel 75 mg daily, prasugrel 10 mg daily,
and ticagrelor 90 mg twice daily.
2011 ACCF/AHA PCI Guidelines
ANTI-ISCHEMIC EFFECTS
vs BLEEDING RISK
The Delicate Balance
CRUSADE Bleeding Score in NSTEMI
• 8 predictors of in-hospital major bleeding in CRUSADE Quality
Improvement Initiative: baseline Hct, CrCl, HR, sex, CHF at
presentation, prior vascular disease, DM, systolic BP
• ↑ Rate major bleeding by bleeding risk score quintiles:
– 3.1% very low risk (score ≤20)
– 5.5% low risk (score 21-30)
– 8.6% moderate risk (score 31-40)
– 11.9% high risk (score 41-50)
– 19.5% very high risk (score >50)
• CRUSADE bleeding score quantifies risk for in-hospital major
bleeding; enhances risk assessment in NSTEMI care; allows
improved risk/benefit analysis
Subherwal S et al. Circulation. 2009;119:1873-1882.
Possible Relationship Between
Bleeding and Mortality
Major Bleeding
Hypotension
Cessation of
ASA/Clopidogrel
Transfusion
Ischemia
Stent Thrombosis
Inflammation
Mortality
Bhatt DL et al. In Braunwald: Harrison’s Online 2005.
CURE: Life-threatening Bleeding
Life-threatening Bleeding
Fatal
Causing 5 g/dL drop hemoglobin
Hypotension requiring inotropic therapy
Surgery required
Causing hemorrhagic stroke
Transfusion of ≥4 blood units
Transfusion of ≥2 blood units
* In combination with standard therapy
The CURE Trial Investigators. N Engl J Med. 2001;345:494-502.
Placebo + ASA*
n = 6303
(%)
Clopidogrel + ASA*
n = 6259
(%)
1.8
0.2
0.9
0.5
0.7
0.1
1.0
2.2
2.2
0.2
0.9
0.5
0.7
0.1
1.2
2.8
TRITON TIMI 38
Bleeding Events – Safety Cohort (n=13,457)
% Events
4
ICH in patients with
prior stroke/TIA
(n=518); Clop
0 vs 60 (0) %
events Pras 6 (2.3)%
(P=0.02)
Clopidogrel
Prasugrel
2.4
2
1.8
1.4
0.9
0.9
1.1
0.4
0
0.1
0.3
0.3
TIMI Major
Bleeds
Life
Threatening
Nonfatal
Fatal
ICH
ARD 0.6%
HR 1.32
P=0.03
NNH=167
ARD 0.5%
HR 1.52
P=0.01
ARD 0.2%
P=0.23
ARD 0.3%
P=0.002
ARD 0%
P=0.74
Wiviott SD et al. N Engl J Med. 2007;357:2001-2015.
PLATO
Major Bleeding: Non-CABG vs CABG
NS
Kaplan-Meier estimated rate (%)
7.9
Ticagrelor
Clopidogrel
8
7.4
7
NS
5.8
6
5
4
5.3
P=0.026
4.5
3.8
P=0.025
2.8
3
2.2
2
1
0
Non-CABG
PLATO major
bleeding
Non-CABG
TIMI major
bleeding
Wallentin L et al. N Engl J Med. 2009;361:1045-1057.
CABG
PLATO major
bleeding
CABG
TIMI major
bleeding
ANTIPLATELET RESPONSE
VARIABILITY
Optimizing Antiplatelet Therapy
Balancing Safety and Efficacy
“Sweet spot”
Ischemic risk
High risk of
bleeding events
Bleeding risk
Inhibition of Platelet Aggregation
ACS = acute coronary syndrome; CKD = chronic kidney disease; DM = diabetes mellitus
Ferreiro JL et al. Thromb Haemost. 2010;103:1128-1135. Courtesy of Stephen Wiviott, MD.
Risk of Any Event
Risk of Any Event
High risk of
ischemic events
Variability in Antiplatelet Effect with
Clopidogrel and Prasugrel
100
n = 64
Interpatient
Variability
60
40
20
Interpatient
Variability
IPA at 24 Hours, %
80
0
-20
Clopidogrel Responder
Clopidogrel Non-responder
Response to
Clopidogrel 300 mg
IPA = inhibition of platelet aggregation
Adapted from Brandt JT et al. Am Heart J. 2007;153:66.e9-e66.e16.
Storey RF. Eur Heart J Suppl. 2008;10(suppl D):D30-D37.
Response to
Prasugrel 60 mg
CYP2C19 Genetic Polymorphisms and
Treatment with Clopidogrel
MAJOR ADVERSE CV EVENTS (n=9684)
RISK RATIO (95% CI)
P VALUE
Carriers vs Non-carriers
1.61 (1.28-2.02)
<0.001
Heterozygotes vs Wildtype
1.50 (1.08-2.08)
0.016
Homozygotes vs Wildtype
1.81 (1.21-2.71)
0.004
Carriers vs Noncarriers
2.76 (1.77-4.30)
<0.001
Heterozygotes vs Wildtype
2.51 (1.59-3.98)
<0.001
Homozygotes vs Wildtype
4.78 (2.01-11.39)
<0.001
Stent Thrombosis (n=5772)
0.5
Risk Lower With
CYP2C19 Variant
1.0
15.0
Relative Risk
Mega JL et al. JAMA 2010; 304:1821-1830. Courtesy of JL Mega and MS Sabatine.
Risk Higher With
CYP2C19 Variant
Prospective Platelet-Monitoring and
Clopidogrel-Titration Study
Mean ±SD
VASP after first LD, %
Control
VASP-guided
P
68 ±11
69 ±10
0.4
38 ±14
<0.0001
VASP after adjustment, %
-49%
-35%
100
-42%
VASP-guided group
CV Event-free
Survival (%)
VASP Index (%)
100
75
50
25
95
90
Control group
85
80
0
VASP 1
(n=78)
VASP 2
(n=78)
VASP 3
(n=40)
VASP 4
(n=26)
0
5
10
15
20
25
30
Bonello L, et al. J Am Coll Cardiol. 2008;51:1404-1411.
Courtesy of Stephen Wiviott MD
GRAVITAS: Trial Design
Successful PCI with DES without major complication or GPIIb/IIIa use
N=~6600
Post-PCI VerifyNow P2Y12 Assay (PRU) 12-24 hours post-PCI
High Residual Platelet Activity
PRU ≥ 230?
Randomized 1:1
N = 1100
Not High Residual Platelet Reactivity
Random Selection
N = 1100
N = 583
“Tailored Therapy”
“Standard Therapy”
“Standard Therapy”
clopidogrel 150 mg/day
clopidogrel 75 mg + placebo/day
clopidogrel 75 mg + placebo/day
Clinical Follow-up And VerifyNow Assessment at 30 days, 6 months
Primary Endpoint: 6 month CV Death, MI, ARC Def/Prob Stent Thrombosis
PRU = P2Y12 reaction units
Price MJ, et al. Am Heart J. 2011.
GRAVITAS: Results and Conclusions
4
CV death, MI, or
Stent Thrombosis
2.3%
2.3%
2
Results
• Same rate of CV death, MI, or stent
thrombosis in 2 groups (P=.98)
• GUSTO moderate or severe bleeding:
1.4% HD vs. 2.3% standard (P=.10)
Conclusions
0
Primary Outcome
primary
outcome
P=.98(NS)
High clopidogrel dose
Standard clopidogrel dose
Price MJ, et al. JAMA. 2011.
• Patients with high residual platelet
reactivity after PCI with DES did not
benefit from high-dose clopidogrel
• High-dose clopidogrel for 6 months did
not reduce the primary ischemic outcome
• GUSTO moderate or severe bleeding was
not increased
• Routine testing of platelet reactivity after
PCI is not warranted
GRAVITAS: CV Events and Post-PCI PRU In Patients With
High and Not High PRU Treated With Clopidogrel
500
Red dots: patients with
CV death, MI, or ST
400
PRU
300
12 - 24 hrs
post-PCI
• hypertensive,
200
100
0
N=1105
High Residual
Reactivity
ITT population
N= 586
Not High
Residual Reactivity
230 PRU
Platelet Function Testing
For Patients Undergoing PCI
RECOMMENDATION
COR
LOE
Platelet function testing in patients at high risk for poor
clinical outcomes
IIb
C
Routine clinical use of platelet function testing to screen
clopidogrel-treated patients undergoing PCI
III – No
Benefit
C
IIb
C
Treatment with an alternate P2Y12 inhibitor (e.g.
prasugrel or ticagrelor) in clopidogrel-treated patients
with high platelet reactivity
GNL. 2011.
PERFORMANCE MEASURES AND
QUALITY OUTCOMES IN ACS
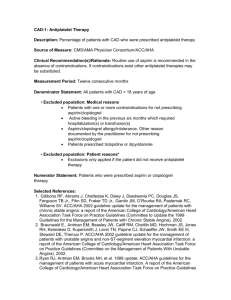
ACC/AHA 2008 Performance Measures at
Discharge for STEMI and NSTEMI
• Aspirin at discharge
• -blocker at discharge
• Statin at discharge (changed from: lipid-lowering therapy in
patients with LDL-C >100 mg/dL)
• ACEI or ARB for LVSD
• Adult smoking cessation advice/counseling
• Cardiac rehabilitation patient referral from an inpatient
setting (new in 2008)
ACEI = angiotensin-converting enzyme inhibitor; ARB = angiotensin receptor blocker; LVSD = left ventricular systolic dysfunction
Krumholz HM et al. J Am Coll Cardiol. 2008;52:2046-2099.
Quality of Care and Outcomes for
Acute Coronary Syndromes
I IIa IIb III
New
2011
It is reasonable for clinicians and hospitals that provide
care to patients with UA/NSTEMI to participate in a
standardized quality-of-care data registry designed to track
and measure outcomes, complications, and adherence to
evidence-based processes of care and quality
improvement for UA/NSTEMI.
Evidence-based Therapies on 6-month
Survival GRACE Registry Cohort*
NUMBER OF THERAPIES
(vs 0 or 1 therapy)
OR
(95% CI)
2 therapies
0.80 (0.52-1.26)
3 therapies
0.74 (0.48-1.13)
4 therapies
0.59 (0.39-0.90)
5 therapies
0.51 (0.33-0.78)
6 therapies
0.40 (0.26-0.62)
7 therapies
0.27 (0.16-0.44)
8 therapies
0.31 (0.17-0.57)
0
OR = odds ratio
*Registry of patients with ACS
Chew DP et al. Heart. 2010;96:1201-1206.
0.5
1
OR
1.5
2
Mean 30-day Hospital Readmission Rates
Following PCI: By Hospital Decile of Readmission
Percent Readmission
30
25
20
15
10
5
0
1st
2nd
3rd
4th
5th
6th
7th
Hospital Decile of Readmission Rate
Curtis JP et al. J Am Coll Cardiol. 2009;54:903-907.
8th
9th
10th
Hospitals
Quality of Care for Heart Attack
Percent of patients who received recommended care
100
100
98
Heart attack 30-day mortality
94
10th %ile
(best)
Median
20
15
50
Percent
Percent
75
25th %ile
25
14
15
10
5
0
0
10th %ile
(best)
Median 90th %ile
(worst)
Data: IPRO analysis of data from CMS Hospital Compare.
Source: Commonwealth Fund National Scorecard on US Health System Performance, 2011.
16
75th %ile
17
90th %ile
(worst)
18
INVESTIGATIONAL POST-DISCHARGE
USE OF ADJUNCTIVE LOW-DOSE
ANTICOAGULATION AFTER ACUTE
CORONARY SYNDROME
RIVAROXABAN: ATLAS ACS 2 TIMI 51
Primary Efficacy Endpoint: CV Death / MI / Stroke
12
2 Yr KM Estimate
Placebo*
10.7%
10
8.9%
8
6
HR 0.84
(0.74-0.96)
Rivaroxaban*
mITT P = 0.008
ITT P = 0.002
(both doses 2.5
mg bid and 5 mg bid)
4
2
0
ARR 1.8%
NNT = 56
0
4
12
16
20
24
1079
2084
421
831
Months After Randomization
No. at Risk
Placebo
Rivaroxaban
8
5113
10229
4307
8502
Mega JL et al. N Engl J Med. 2012;366:9-19.
3470
6753
2664
5137
1831
3554
*with clopidogrel in majority of patients
RIVAROXABAN: ATLAS ACS 2 TIMI 51
Efficacy Endpoints: Very Low Dose 2.5 mg BID
Patients Treated with Aspirin + Thienopyridine
CV Death / MI / Stroke
Cardiovascular Death
5%
HR 0.84
12%
Placebo
HR 0.66
9.0%
mITT
P<0.001
Placebo
4.2%
10.4%
Estimated Cumulative incidence (%)
mITT
P=0.04
ITT
P=0.01
ITT
P<0.001
2.5%
Rivaroxaban
2.5 mg BID
Rivaroxaban
2.5 mg BID
NNT = 59
NNT = 71
0
12
Months
Mega JL et al. N Engl J Med. 2012;366:9-19.
24
0
12
Months
24
RIVAROXABAN: ATLAS ACS 2 TIMI 51
Treatment Emergent Fatal Bleeds and ICH
1.2
1
P = NS for Riva vs Placebo
P = NS for Riva 5 vs Placebo
P = NS for Riva 2.5 vs Placebo
P = 0.044 for Riva 2.5 vs 5
P = 0.009 for Riva vs Placebo
P = 0.005 Riva 5 vs Placebo
P = 0.037 for Riva 2.5 vs Placebo
P = 0.44 for Riva 2.5 vs 5
0.8
Placebo
2.5 mg Rivaroxaban
5.0 mg Rivaroxaban
0.7
P = NS for all
comparisons
0.6
0.4
0.4
0.2
0
0.2
0.4
0.2
0.2
0.1
n=9
n=6 n=15
n=5 n=14 n=18
Fatal
ICH
ICH: intracranial hemorrhage
Adapted from Mega JL et al. N Engl J Med. 2012:336:9-19.
0.1
0.1
n=4
n=5
Fatal ICH
n=8
Apixaban: APPRAISE-2 Trial
Primary Outcome: CV Death, MI, Ischemic Stroke
Apixaban 279 (7.5%)
Placebo 293 (7.9%)
HR 0.95; 95% CI 0.80-1.11; P=0.509
Alexander JH et al. N Engl J Med. 2011;365:699-708.
CONCLUSIONS
Clinical Management of Acute Chest Pain Syndrome
• Need for differential diagnosis of the spectrum of ACS
• Fundamental aspects of management of acute chest pain
– Elements for optimal early hospital care
• The importance of risk stratification to guide practice decisions
– Options: initial conservative or invasive strategy
– If invasive strategy, rationale for early catheterization
• The expanded field of existing antiplatelet treatment options
– Clopidogrel, prasugrel, ticagrelor
• The need to balance anti-ischemic effects vs bleeding risk
• Post-discharge anticoagulant therapy for ACS
– Current contender: very low dose rivaroxaban
• The growing importance of quality outcomes in ACS