Mag. Res. In Med.

Northwestern University Feinberg School of Medicine
Voxel Transit Time is a More Sensitive Measure of
Altered Tissue Perfusion Than Mean Transit Time in Advanced Intracranial Atherosclerotic Disease
EP-36
AW Korutz, D Ban, F Syed, A Honarmand, MC Hurley, TJ Carroll and SA Ansari
Departments of Radiology and Biomedical Engineering, Northwestern University,
Feinberg School of Medicine, Chicago, IL
2
Disclosures
The authors have no conflicts of interest or financial relationships to disclose with respect to industry research support, consulting, or speaking
There will be no discussion of unapproved/off-label or investigational device utilization
.
3
Background
• Stroke is the 3 rd leading cause of death in the US 1
• Intracranial atherosclerotic disease (ICAD) is responsible for
7-10% of all strokes, with up to a 23% recurrence rate in 1 year despite optimal medical management. 2-4
• MRI Perfusion - Traditionally a measure of relative CBV by
Dynamic Susceptibility Contrast MRI (i.e rCBV
DSC
) 5
• Tissue-concentration curve generated with GRE-EPI
• Arterial Input Function (AIF) generated by the concentration curve in region of major intracranial vessel (i.e. MCA)
• rCBV related to the ratio: area under tissue-concentration curve / area under AIF curve
Background
• Initial attempts at quantitation used population-based scaling factors 6,7
• i.e. scaling “presumed normal” white matter to a constant value or calculation of venous output function.
• Does not account for patient-specific physiology/pathology.
4
• Newer attempts at quantification of perfusion 8-11
• Employ patient specific calibration factors based on T1 changes in white matter relative to the blood pool (CBVss)
• Additional modeling of rate of intra-extravascular water exchange
• Performed using a “Bookend” technique with T1 measurement before and after perfusion imaging
• Reproducible, reliable and accurate 12
5
Background
• Despite the attempts at quantification in perfusion MRI, perfusion imaging continues to underestimate the effects of bolus delay and dispersion (DnD).
13
• Broadening of the contrast bolus during injection
• Broadening of the bolus during the circulation through the heart and lungs
• Broadening of the bolus due to proximal arterial stenoocclusive disease.
• Recently published research has proposed an algorithm to correct for DnD effects as seen in MR perfusion imaging performed with Bookend Dynamic Susceptibility
Contrast MRI (DSC-MR PWI).
14
6
Background
• Our goal
• To compare conventional mean transit time (MTT) to voxel transit time (VTT) derived from a locally determined AIF in patients with vessels supplied by vessels with severe
(>50%) intracranial atherosclerotic disease (ICAD).
• Our hypothesis
• VTT is a more sensitive metric of hypoperfusion than MTT in the setting of severe ICAD.
Materials and Methods
• Using our institution ’s PACS and medical record databases we retrospectively identified and analyzed 7 patients
• Patients were excluded with occlusion related to presumed central emboli or those with a history of prior endovascular/surgical intervention.
• Territories were excluded with encephalomalacia involving >50% of the territory volume or intermediate atherosclerotic narrowing (0-50%)
7
• Included patients had moderate to severe narrowing
(>50%) of one or more of the major intracranial vessels
• Supraclinoid ICA, A2 ACA, M1/M2 MCA or P2 PCA
Materials and Methods
• Analysis was performed on the major intracranial vascular territories (ACA, MCA and PCA)
• Separated into those with no vascular narrowing
(Normal), intermediate vascular narrowing (0-50% stenosis) and advanced vascular narrowing (> 50%).
• Territories with intermediate narrowing were excluded from analysis
8
• For supraclinoid ICAD Imaging was reviewed to evaluate the ipsilateral A1 ACA and the PCOM.
• If the A1 was hypoplastic/aplastic, the ACA territory was included in the
“Normal” group.
• If a fetal type PCA was present, the PCA was included in the “Advanced ICAD” group.
9
Materials and Methods
• Voxel transit time was calculated by forward convolving the global AIF to remove the effects on the shape of the contrast bolus as it flows through the cerebral vasculature, including the pial collateral arteries.
• The final deconvolution analysis yields a much shorter mean time for the bolus to traverse the image voxel.
Materials and Methods
• To only include brain parenchyma in the perfusion quantification, regions of encephalomalacia were excluded manually by a neuroradiologist on T2 images.
These images were then used to create subtraction masks.
• Each subject’s T1 images were warped to MNI space using the SPM software package in MATLAB.
10
• Perfusion and T2 images were then coregistered to the warped T1 images as well as vascular territory maps
• Automated segmentation of vascular territories could be performed for quantification of territory-specific MTT/VTT.
Materials and Methods
• Vascular Territory Maps
• Maps were created when a neurointerventional radiologist manually outlined the vascular territories on a high resolution T1 sequence from a single subject in MNI space
• These images were coregistered to an average of 128 normal subject T1 images
SPM ’s T1.nii template
11
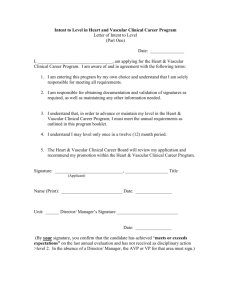
Three select T1 images with vascular maps applied. These images show the ACA, PCA and all three divisions of the
MCA (superior, inferior and perforators)
12
Materials and Methods
• Using the vascular maps, co-registered perfusion images were segmented into separate vascular territories in
MATLAB.
• T2 masks were applied to the vascular territories
• Final VTT and MTT values were generated for each vascular territory
13
Materials and Methods
• Statistics
• Perfusion values were compared using a two-tailed
Student ’s t-test
• Patient age in the two experimental groups was compared using a two-tailed Student ’s t-test
• Patient sex in the two experimental groups was compared using a Chi Square test.
14
Results
• Demographics
• 3 male, 4 female patients (mean 66 +/- 15 years)
• 17 vascular territories with severe ICAD were included
2 ACA, 7 MCA and 8 PCA
• 16 vascular territories without ICAD were included
8 ACA, 4 MCA and 4 PCA
15
Results
• Demographics
• Age (Not significant between normal and severe ICAD)
65 +/- 17 years in vascular territories with normal vessels
66 +/- 15 years in vascular territories with severe ICAD
• Sex (Significant difference p = 0.02)
Territories with normal vessels - 11 men and 5 women
Territories with severe ICAD - 5 men and 12 women
16
Results
MTT VTT
Normal Vessel 4.0 +/- 0.26 sec 0.36 +/-0.04 sec
Severe ICAD 3.8 +/- 0.21 sec 1.0 +/- 0.19 sec
MTT difference between groups was not significant: p=0.46
VTT difference between groups was significant: p< 0.01
Conclusions
• ICAD alters the the shape of the contrast bolus as it flows towards the parenchyma that it supplies
• Mean transit time derived from typical deconvolution analysis does not include DnD effects from the supplying arterial network
• Voxel transit time may better represent transit time in flowlimiting pathologies such as ICAD
17
• DnD correction may unveil territories which are hemodynamically compromised, but would otherwise appear similar to territories supplied by normal vessels.
18
References
1. Roger VL, Go AS, Lloyd-Jones EM, et al. Heart Disease and Stroke Statistics –
2011 Update. Circulation 2011; 123:e18-e209.
2. Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race-ethnicity and
Determinants of Intracranial Atherosclerotic Cerebral Infarction: The Northern
Manhattan Stroke Study. Stroke 1995; 26:14-20.
3. Chimowitz MI, Lynn MJ, Howlett-Smith H, et al. Comparison of Warfarin and aspirin for Symptomatic Intracranial Arterial Stenosis. NEJM 2005; 352:1305-1316.
4. Chimowitz MI, Lynn MJ, Derdeyn CP, et al. Stenting versus Aggressive Medical
Therapy for Intracranial Arterial Stenosis. NEJM 2011; 365:993-1003.
5. Sakaie KE, Shin W, Curtin K, et al. Method for Improving the Accuracy of
Quantitative Perfusion Imaging. J. MRI 2005; 21:512-519.
6. Mukherjee P, Kang HC, Videen TO, et al. Measurement of Cerebral Blood Flow in Chronic Carotid Occlusive Disease: Comparison of Dynamic Susceptibility
Contrast Perfusion MR Imaging with Positron Emission Tomography. AJNR
2003;24:862-871.
7. Lin W, Celik A, Derdeyn C, et al. Quantitative Measurements of Cerebral Blood
Flow in Patients with Unilateral Carotid Artery Occlusion: A PET and MR Study. J
MRI 2001;14:659-667.
19
References
8. Shin W, Cashen TA, Horowitz SW, et al. Quantitative CBV Measurement From
Static T1 Changes in Tissue and Correction for Intravascular Water Exchange.
Mag. Res. In Med. 2006; 56:138-145.
9. Shin W, Horowitz S, Ragin A, et al. Quantitative Cerebral Perfusion Using
Dynamic Susceptibility Contrast MRI: Evaluation of Reproducibility and Age- and
Gender-Dependence with Fully Automated Image Processing Algorithm. Mag.
Res. In Med. 2007;58:1232-1241.
10. Parikh V, Shin W, Mouannes J, et al. QCBF: A Comparison of the Accuracy
Between the Bookend Technique, Empirical Reference Values and [O 15 ]-H
2
O PET in Moyamoya Patients. Proc. Intl. Soc. Mag. Reson. Med Poster Presentation
2009.
11. Leenders KL, Perani D, Lammertsma AA, et al. Cerebral Blood Flow, Blood
Volume and Oxygen Utilization: Normal Values and Effect on Age. Brain.
1990;113:27-47.
12. Vakil P, Lee JJ, Mouannes-Srour JJ, et al. Cerebrovascular occlusive disease: quantitative cerebral blood flow using dynamic susceptibility contrast mr imaging correlated with quantitative H2[O]15-PET. Radiology. 2013;266(3):879-86.
20
References
13. Calamante F. Bolus Dispersion Issues Related to the Quantification of
Perfusion MRI Data. J. Magn. Reson. Imaging. 2005;22(6):718-22.
14. Mouannes-Srour JJ, Shin W, Ansari SA, et al. Correction for Arterial-Tissue
Delay and Dispersion in Absolute Quantitative Cerebral Perfusion DSC MR
Imaging. Magn. Reson. Med. 2012;68:495-506.