Cigarette Smoking, Cardiovascular Disease Risk, and
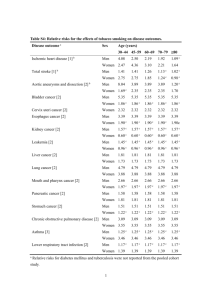
advertisement

CIGARETTE SMOKING, CARDIOVASCULAR DISEASE RISK, AND IMPLEMENTATION STRATEGIES FOR SMOKING CESSATION Adapted and Modified from: Luepker RV, Lando HA. Tobacco Use and Passive Smoking, in: Wong ND, Black HR, Gardin JM, eds. Preventive Cardiology, Mc Graw Hill, 2000 and NANCY HOUSTON MILLER, R.N., B.SN., Stanford University Roger Blumenthal, MD et al ACC Prevention Guidelines 2007 ____________________________________________________________ Smoking Statement Issued in 1956 by American Heart Association ___________________________________________________________ “It is the belief of the committee that much greater knowledge is needed before any conclusions can be drawn concerning relationships between smoking and death rates from coronary heart disease. The acquisition of such knowledge may well require the use of techniques and research methods that have not hitherto been applied to this problem.” Circulation 1960; vol. 23 ___________________________________________________________ Smoking: Mortality 33.5% of smoking-related deaths among Americans are cardiovascular-related Male smokers die an average of 13.2 years earlier than male nonsmokers Female smokers die an average of 14.5 years earlier than female nonsmokers Current cigarette smoking is a powerful independent predictor of sudden cardiac death in patients with CHD Cigarette smoking results in a two- to threefold risk of dying from CHD Arch Intern Med. 2003;163:2301–2305. Surgeon General’s Health Consequences of Smoking, 2004. CDC/NCHS. Tobacco-Related Mortality, Fact Sheet. CDC.gov/tobacco. February 2004. Heart Disease and Stroke Statistics—2005 Update, AHA. • MMWR, Vol. 51, No. 14, 2002, CDC/NCHS. CHD Risk by Cigarette Smoking. Filter Vs. Non-filter. Framingham Study. Men <55 Yrs. 14-yr. Rate/1000 250 Non-Smoker Reg. Cig. Smoker Filter Cig. Smoker 200 206 150 210 100 210 119 112 50 59 0 Total CHD Myocardial Infarction Percent of Population 40 35 30 25 20 15 10 5 0 37.3 33.4 24.1 23.9 20.4 20.2 18.9 17.8 15 11.3 Men NH White NH Black Hispanic Women Asian American Indian or Alaska Native Prevalence of current smoking for Adults age 18 and older by race/ethnicity and sex (NHIS:2004). Source: MMWR. 2004;54:1121-24. NH – non-Hispanic. Percent of Population 45 40 35 30 25 20 15 10 5 0 24.9 27 24.8 19.2 14 NH Whites 11.9 NH Blacks Males Hispanics Females Prevalence of high school students in grades 9-12 reporting current cigarette smoking by race/ethnicity and sex. (YRBS:2005).Source: MMWR. 2006;55:SS-5. June 9, 2006. . NH – non-Hispanic. • TOBACCO USE AS A CARDIOVASCULAR RISK FACTOR • OVERVIEW OF SMOKING CESSATION AND THE IMPORTANCE OF INTERVENING IN CLINICAL PRACTICE • LESSONS LEARNED FROM THE IMPLEMENTATION AND DISSEMINATION OF A SUCCESSFUL RESEARCH PROGRAM IN HOSPITALIZED PATIENTS • INTRODUCING SYSTEM - WIDE CHANGES FOR SUCCESS WITH CARDIAC AND OTHER HOSPITALIZED PATIENTS SMOKING: THE FACTS • FIFTY MILLION AMERICANS SMOKE (1 IN 4 ADULTS) • FIFTY PERCENT ATTEMPT TO QUIT ANNUALLY • ONLY 42% OF M.I. SMOKERS RECEIVED SMOKING CESSATION INTERVENTIONS AT HOSPITAL DISCHARGE (NRMI II) • ONLY 21% OF SMOKERS RECEIVED COUNSELING @ CLINIC VISITS (1995) • TREATMENT IS MOST OFTEN OFFERED TO THOSE WITH TOBACCO-RELATED DISEASES • DIRECT/INDIRECT MEDICAL COSTS APPROACH $130 BILLION ANNUALLY U.S. Deaths Attributable to Cigarette Smoking, 1994, Centers for Disease Control and Prevention Chronic Lung Disease Lung Cancer 81000, 19% 72000, 17% 24000, 6% 32000, 7% 98000, 23% 123000, 28% Coronary Heart Disease Other Cancers Stroke Other CIGARETTE SMOKING MORTALITY • ONE IN EVERY FIVE DEATHS FROM CARDIOVASCULAR DISEASE IN THE UNITED STATES IS SMOKING-RELATED • ON AVERAGE, SMOKERS DIE SEVEN YEARS EARLIER THAN NONSMOKERS. • 430,700 DEATHS OCCUR ANNUALLY FROM CIGARETTE SMOKING WITH 75% BEING DUE TO CANCERS AND HEART DISEASE. • DEATHS FROM LUNG CANCER AMONG WOMEN HAVE INCREASED 400%. IN 1994, 64,300 WOMEN DIED FROM LUNG CANCER AND 44,300 DIED FROM BREAST CANCER. MORBIDITY AND MORTALITY WEEKLY REPORT, 1997 AMERICAN CANCER SOCIETY, ATLANTA GEORGIA, 1996. Cigarette Smoking as a CHD Risk Factor • In PDAY study of autopsies performed on 1443 men and women aged 15-34 years, smoking was associated with excess of fatty streaks and raised lesions in the abdominal aorta. • Mechanism of injury from cigarette smoking may come from injury to endothelium, and acute effects ma include alterations in clotting, platelet adhesion, and coronary vasoconstriction due to nicotine. • Relative risk of CHD death from MRFIT study 2.1 for 1-25 cigarettes/day rising to 2.9 for >25 cigarettes/day • Acute MI and sudden death strongly associated with cigarette smoking. • Cigarette smoking has additive effect to CHD risk above lipids, obesity, diabetes, and hypertension Cohort Studies of Environmental Tobacco Smoke and CHD Source Hirayama Garland Svendsen Helsing Location,Date Japan 1984 US 1985 US 1987 US 1988 Population 91,540 695 1245 19035 Hole Layard UK 1989 US 1995 7987 2916 Tunstall-Pedoe UK 1995 2278 Steenland US 1996 309599 Kawachi US 1997 32046 RR (95% CI) 1.2 (0.9-1.4) 2.7 (0.7-10.5) 2.2 (0.7-6.9) M 1.3 (1.1-1.6) F 1.2 (1.1-1.4) 2.0 (1.2-3.4) M 0.97 (0.7-1.3) F 0.99 (0.8-1.2) 2.7 (1.3-5.6) M 1.2 (1.1-1.4) F 1.1 (-.96-1.3) F 1.9 (1.1-3.3) Environmental Tobacco Smoke and CHD • 35,000-40,000 deaths annually from acute MI are associated with environmental tobacco exposure, significantly more than due to lung cancer. • Recent meta analysis of passive smoking incorporating home-based and workplace studies (1699 cases) showed relative risk of 1.49 (1.29-1.72) • Sidestream smoke released into the environment may be more toxic and nonsmokers who are exposed regularly develop various physiologic changes and are more sensitive than regular smokers. • Lower HDL-C and platelet abnormalities, higher CO levels and lower exercise tolerance are noted. Trends in Cigarette Smoking: High School Youth (Everett et al) 40 35 30 25 20 1991 1995 15 10 5 0 9th Grade 10th Grade 11th Grade 12th Grade Percent of High School Students Who Reported Cigarette Smoking, 1995, CDC WV MO WY OH ME NE RI NJ IL TN MT CO SC NC GA CA UT 0 10 20 30 40 50 Percent of Adults Who Reported Cigarette Smoking, 1996, CDC KY OH MO WV AK NC IL VA DE VT MA NY CO NE NM CT MN MD CA UT 0 5 10 15 20 25 30 35 Prevention and Intervention Strategies in Youth • School-based prevention programs – Social environment / influences • Community-based prevention programs – May enhance effects of school-based programs • State and federal prevention initiatives – Anti-tobacco media campaigns – Restrictions on tobacco advertising – Restrictions on tobacco availability to minors – Restrictions on smoking in public places including schools – Increased taxation Adult Cessation Strategies • Contingency contracting (wards for abstinence) • Social support (from clinician, group, family, friends) • Relaxation techniques (progressive relaxation, deep breathing) • Stimulus control and cue extinction (restricting where smoking takes place) • Coping skills • Reduced smoking and nicotine fading (gradual reduction) • Multicomponent treatment programs • Hypnosis • Acupuncture • Self-help (written materials, videos, tapes, hotlines, helplines) • Computer-tailored messages Time-to-Benefit of Smoking Cessation After Last Cigarette Within 20 minutes: BP decreases; body temperature, pulse rate returns to normal Within 24 hours: Risk of MI decreases Within 1 year: Excess risk for CHD is half that of a person who smokes At 5 years: Stroke risk is reduced to that of someone who has never smoked Within 15 years: CHD risk is the same as a person who has never smoked American Lung Association. www.lungusa.org/tobacco/quit_ben.html Counseling: 5 A’s Ask: Systematically identify all tobacco-users at every visit Advise: Strongly urge all smokers to quit Attempt: Identify smokers willing to try and quit Assist: Aid the patient in quitting Arrange: Schedule follow-up contact Estimated cessation rate (%) Efficacy of various behavioural support approaches 20 16.8 15 12.3 13.9 13.1 10.8 10 5 0 No intervention (reference group) Self-help Proactive telephone counselling Individual counselling Group counselling USDHHS. Treating Tobacco use and dependence. A clinical practice guideline. Rockville, MD AHQR 2000. EFFICACY OF SMOKING CESSATION INTERVENTIONS (1 YEAR QUIT RATES) ACUPUNCTURE ---- HYPNOSIS ---- PHYSICIAN ADVICE 6% SELF-HELP METHODS 14% NICOTINE PATCH 11-15% PHYSICIAN ADVICE/SELF-HELP PAMPHLETS 22% AVERSIVE SMOKING (RAPID PUFFING) 25% PHARMACOTHERAPY/BEHAVIORAL THERAPY25% BEHAVIORAL STRATEGIES (GROUP PROG.) 40% Tailored vs. generic behavioural support material % Abstinent at 4 months Self-help materials tailored for the needs of individual smokers are more effective than standard materials 35 30.7 Generic materials Tailored materials 30 25 20 15 10 7.7 7.1 9 5 0 Light / moderate (<20 cig/day) Heavy (>20 cig/day) Cigarettes smoked per day Strecher VJ. Patient Educ Couns. 1999; 36: 107-117. Strecher VJ, et al. Journal of Family Practice. 1994; 39(3): 262–270. Pharmacologic Treatment Options TREATMENT POTENTIAL RISKS Nicotine patch Skin rashes and irritation Nicotine polacrilex (nicotine gum) Mouth soreness, hiccups, dyspepsia, jaw ache Nicotine nasal spray Nose and eye irritation, usually disappears within 1 week Nicotine inhaler May cause mouth or throat irritation Zyban (bupropion hydrochloride) Slight risk of seizure, contraindicated in those with eating or seizure disorders Nicotine Replacement Therapy Potent psychoactive drug that induces euphoria Effects are related to blood concentration and the rate of increase in concentration Safe in patients with cardiovascular disease Should be used as part of smoking cessation therapy; however, many individuals may quit without it Smoking and Nicotine Other toxins in tobacco smoke, not nicotine, are responsible for majority of adverse health effects >4000 different chemicals Tar, carbon monoxide, irritants, and oxidant gases >40 carcinogens The main adverse effect of nicotine from tobacco is addiction, which sustains tobacco use Nicotine dependence leads to continued exposure to toxins in tobacco smoke Smith et al. Food Chem Toxicol. 1997;35:1107–30. Hoffman and Hoffman. J Toxicol Environ Health. 1997;50:307–64. Benowitz NL. Nicotine Safety and Toxicity. New York: Oxford University Press, 1998. Nicotine Replacement Therapy (NRT) Goal: Attenuate symptoms related to nicotine withdrawal Dysphoric or depressed mood Insomnia Irritability, frustration, or anger Anxiety Difficulty concentrating Restlessness Decreased heart rate Increased appetite or weight gain NRT: Treatment Options Forms of NRT: Gum, Patch, Inhaler, Lozenge, Nasal spray, Sublingual tablet All forms of NRT appear to be similarly effective NRT choice may be based on susceptibility to side effects, patient preference, and availability Little research on combinations of different types of NRT Limited evidence that adding another form of NRT to the nicotine patch increases the success rate Plasma nicotine concentrations for smoking and NRT 14 Increase in nicotine concentration ( ng/ml ) 12 10 8 Cigarette Gum 4 mg 6 Gum 2 mg 4 Inhaler Nasal spray Patch 2 0 5 10 15 20 25 30 Minutes Balfour DJ and Fagerström KO. Pharmacol Ther. 1996;72:51-81. NRT: Benefit of Behavioral Support Limited Support Intervention Nicotine gum Nicotine transdermal patch Effect size 5% 5% 95% CI 4%-6% 4%-7% Intensive Support Intervention Nicotine gum Nicotine transdermal patch Nicotine nasal spray Nicotine inhalator Nicotine sublingual tablet Effect size 8% 6% 12% 8% 8% 95% CI 6%-10% 5%-8% 7%-17% 4%-12% 1%-14% West R, McNeill A and Raw M. Thorax. 2000;55:987-999. Silagy C, et al. Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev. 2002; 1. Safety of NRT NRT is safe in most individuals with cardiovascular disease, even with concomitant smoking There is a negligible risk of cancer compared to the risk from continued smoking Although it is a potential fetal teratogen, the benefits outweigh the risks of smoking during pregnancy There is a low risk of abuse Buproprion (Zyban) Sustained release form of the antidepressant Acts by enhancing CNS noradrenergic and dopaminergic function Start 1 week before smoking cessation date 150 mg QD x 3d, then 150 mg BID x 60d Higher doses and longer duration with greater side effects and no clear benefit Buproprion (Zyban) vs. NRT Jorenby DE et al. N Engl J Med. 1999 Mar 4;340(9):685-91 Other Therapies: Limited Success Clonidine Nortryptiline (tricyclic antidepressant) Maclobemide (MAO-inhibitor) Buspirone (anxiolytic) Naloxone (opiate antagonist) Naltrexone (opiate antagonist) Amphetamines ‘Reduced risk’ cigarettes Includes low tar and ‘light’ cigarettes, and novel products that deliver nicotine with minimal tobacco combustion Low tar cigarettes have not be shown to substantially reduce health hazards of smoking but do provide sufficient nicotine to sustain addiction Some novel products may deliver fewer or lower levels of toxins but some deliver more carbon monoxide. Smoking cessation medications are most likely safer than any ‘reduced risk’ cigarette Smokeless tobacco Snuff or chewing tobacco has been suggested as a potential aid to harm reduction or smoking cessation Such products known to cause oral cancer Smokeless tobacco is addictive and not recommended for smoking cessation CLINICAL PRACTICE GUIDELINE “TREATING TOBACCO USE AND DEPENDENCE” • 6,000 ARTICLES (1975-99) INCORPORATING 50 META-ANALYSES • REF: JAMA 2000; 283: 3244-3254 • AVAILABLE ON HTTP://WWW.AHQR.GOV U.S. DEPARTMENT OF HEALTH AND HUMAN SERVICES THE CLINICAL PRACTICE GUIDELINE ON SMOKING WHAT’S NEW? • TREATMENT OF TOBACCO MUST BE CONSIDERED A CHRONIC DISEASE • ALL CLINICIANS SHOULD OFFER AT LEAST A 3 MIN COUNSELING INTERACTION AT EVERY VISIT • ALL SMOKERS WILLING TO QUIT SHOULD BE OFFERED PHARMACOTHERAPY (EXCEPTIONS: PREGNANT/ BREAST - FEEDING WOMEN, ADOLESCENTS, THOSE WITH MEDICAL CONTRAINDICATIONS, OR < 10 CIGS/DAY) THE CLINICAL PRACTICE GUIDELINE ON SMOKING WHAT’S NEW? • CLINICIANS AND HEALTH CARE DELIVERY SYSTEMS MUST IDENTIFY, DOCUMENT, AND TREAT EVERY TOBACCO USER • INSURERS AND PURCHASERS SHOULD REIMBURSE: a. COUNSELING/PHARMACOTHERAPY FOR PATIENTS b. CLINICIANS WHO PROVIDE TOBACCO DEPENDENCE TREATMENT PERFORMANCE MEASURES FOR SMOKING CESSATION: HOW DO THEY DIFFER? AMA - (1) ALL CHRONIC STABLE CORONARY ARTERY DISEASE PTS IDENTIFIED AS SMOKERS DURING THE REPORTING YEAR (2) ALL CHRONIC STABLE CORONARY ARTERY DISEASE PTS WHO RECEIVE TOBACCO CESSATION INTERVENTION IN THE REPORTING YEAR HCFA - ALL AMI PTS. SMOKING WITHIN ONE YEAR PRIOR TO ADMISSION WHO RECEIVE SMOKING CESSATION ADVICE OR COUNSELING DURING HOSPITALIZATION PERFORMANCE MEASURES FOR SMOKING CESSATION: HOW DO THEY DIFFER? NCQA - BY SURVEY ALL CURRENT/RECENT QUITTERS THAT HAD ONE OR MORE VISITS INDICATING THEY RECEIVED ADVICE TO QUIT FROM AN MCO PRACTITIONER JCAHO - ALL AMI PATIENTS SMOKING WITHIN THE YEAR PRIOR TO ADMISSION WHO RECEIVE SMOKING CESSATION ADVICE OR COUNSELING DURING HOSPITALIZATION POINT OF ACCESS: THE USE OF HOSPITALS FOR SMOKING CESSATION • 30-40 MILLION PEOPLE HOSPITALIZED ANNUALLY • 20-30% OF HOSPITALIZED PATIENTS SMOKE • MOST SMOKERS HAVE HAD TO QUIT • GREATER MOTIVATION TO QUIT • OPPORTUNITY FOR COUNSELING GENERAL INTERVENTION METHODS INHOSPITAL • RN/MD COUNSELING • AUDIOVISUAL MATERIALS • SELF-HELP PAMPHLETS POSTHOSPITAL • RN INITIATED PHONE CALLS: WEEKLY X 2-3 WEEKS MONTHLY X 4-6 MONTHS • NICOTINE REPLACEMENT THERAPY • 1-2 FACE-TO-FACE VISITS AS NEEDED DISSEMINATION OF “STAYING FREE” SMOKING CESSATION PROGRAM PRIMARY AIM • TO DETERMINE EFFECTIVENESS OF INITIAL IMPLEMENTATION INTO SEVERAL HOSPITALS IN SAN FRANCISCO BAY AREA SECONDARY AIM • TO IMVESTIGATE FACTORS THAT PREDICT SUSTAINABILITY OF STAYING FREE STAYING FREE INTERVENTION WHAT PATIENTS RECEIVE: – A STRONG PHYSICIAN MESSAGE ABOUT THE HAZARDS OF SMOKING – A 17 PAGE WORKBOOK ON QUITTING SMOKING – A 16 MINUTE VIDEOTAPE SHOWN AT THE BEDSIDE ABOUT HOW TO REMAIN AN EX-SMOKER – A RELAXATION AUDIOTAPE STAYING FREE INTERVENTION WHAT PATIENTS RECEIVE: – A COUNSELING SESSION AT THE BEDSIDE BY A HEALTH CARE PROFESSIONAL – PHARMACOLOGICAL THERAPY AS NEEDED – FOLLOW-UP PHONE CALLS FROM HOSPITAL STAFF AND/OR PUBLIC HEALTH (1 TO 4) – OUTPATIENT REFERRALS TO PUBLIC HEALTH PROGRAMS AND OTHER LOCAL RESOURCES STANDARD PROGRAM IMPLEMENTATION STAYING FREE HOSPITAL ADVISORY BOARD – MULTIDISCIPLINARY TEAM COMPRISED OF PHYSICIANS, PSYCHOLOGISTS, NURSING STAFF, SOCIAL WORKERS, RESPIRATORY THERAPISTS AND OTHERS • PHYSICIAN ORIENTATION – HOT PINK STAYING FREE STICKERS PLACED ON PATIENT CHARTS TO CUE PHYSICIANS TO DELIVER STRONG MESSAGE – PHYSICIAN INFORMATION POCKET CARDS – GRAND ROUNDS OR MONTHLY STAFF MEETING PRESENTATIONS REGARDING PHYSICIANS’ KEY ROLE IN SMOKING CESSATION STANDARD PROGRAM IMPLEMENTATION PATIENT IDENTIFICATION – COMPUTERIZED ADMISSIONS FORMS OR PAPER ADMISSIONS SLIPS – NURSING HISTORIES – SELF REFERRAL TRIGGERED BY PUBLICITY MATERIALS (E.G., POSTERS) – IDENTIFICATION QUESTIONS “HAVE YOU SMOKED ANY TOBACCO PRODUCTS IN THE PAST 30 DAYS?” “ARE YOU WILLING TO MAKE AN ATTEMPT TO QUIT SMOKING DURING THIS HOSPITALIZATION?” • REFERRAL – PHYSICIANS, CASE MANAGERS, NURSING AND UNIT STAFF – DEDICATED STAYING FREE TELEPHONE LINE – REFERRAL SLIPS STANDARD PROGRAM IMPLEMENTATION PATIENT EDUCATION – NURSING AND/OR INTERVENTION STAFF PROVIDE PATIENT WORKBOOK, VIDEOTAPE AND RELAXATION AUDIOTAPE • FOLLOW-UP TELEPHONE CONTACT – 1 TO 4 TIMES POST DISCHARGE MODEL I: A VA HOSPITAL PALO ALTO HEALTH CARE SYSTEM • SPECIAL FEATURES: – INTERVENTION PROVIDED BY PSYCHOLOGISTS, PSYCHOLOGY INTERNS AND QUALITY ASSURANCE NURSE – USE OF CLOSED CIRCUIT TV TO SHOW VIDEO – USE OF COMPUTERIZED STAYING FREE TEMPLATES TO DOCUMENT INTERVENTION IN PATIENTS’ ELECTRONIC MEDICAL RECORDS – STAYING FREE GROUP E-MAIL CREATED TO DISSEMINATE INFORMATION/UPDATES TO TEAM – “ASK ME ABOUT STAYING FREE” ID TAGS FOR STAFF MODEL II: A COUNTY HOSPITAL SANTA CLARA VALLEY MEDICAL CENTER • SPECIAL FEATURES: – INTERVENTION PROVIDED BY PHYSICIANS – FOLLOW-UP PHONE CALLS PROVIDED BY SANTA CLARA COUNTY PUBLIC HEALTH TOBACCO PREVENTION AND EDUCATION PROGRAM – SPANISH AND VIETNAMESE LANGUAGE VERSIONS OF STAYING FREE – CERTIFICATES OF ACHIEVEMENT FOR PATIENTS MODEL III: COMMUNITY HOSPITALS • SPECIAL FEATURES: – MILLS-PENINSULA HEALTH SERVICES INTERVENTION PROVIDED BY CARDIAC REHABILITATION AND A DIVERSE TEAM OF VOLUNTEERS (NURSING STUDENT, FORMER CARDIAC REHABILITATION PATIENTS, MENDED HEARTS VOLUNTEERS, RETIRED COUNSELORS) DEDICATED STAYING FREE PHONE LINE – COMMUNITY HOSPITAL OF LOS GATOS INTERVENTION PROVIDED BY STAFF CHAPLAIN COMPUTERIZED IDENTIFICATION OF ALL SMOKERS AT ADMISSION MODEL IV: A UNIVERSITY TEACHING HOSPITAL STANFORD UNIVERSITY HOSPITAL • SPECIAL FEATURES: – PARTNERSHIP WITH COMMUNITY AND PATIENT RELATIONS PROGRAM – INTERVENTION PROVIDED BY “SMOKING CESSATION ADVISORS,” (HEALTH PROFESSIONAL VOLUNTEERS AND MEDICAL SCHOOL TRACK UNDERGRADUATES) MAKING HOSPITAL-WIDE SYSTEM LEVEL CHANGES THAT SUCCEED STEP 1: DETERMINE PERCENTAGE OF ALL SMOKERS ENTERING A HOSPITAL WHO SMOKED IN PAST 30 DAYS • ADMISSION SHEETS • FACE TO FACE CONTACT (2-4 WEEKS) MAKING HOSPITAL-WIDE SYSTEM LEVEL CHANGES THAT SUCCEED STEP 2: ACTIVELY SCREEN ALL SMOKERS • UTILIZE COMPUTERIZED ADMISSION FORM • INCORPORATE INTO NURSING HISTORIES • INTEGRATE AS PART OF STANDING CCU/CSU ADMISSION ORDERS • INCORPORATE AS A VITAL SIGN • USE PATIENT STICKERS MAKING HOSPITAL-WIDE SYSTEM LEVEL CHANGES THAT SUCCEED STEP 3: EXPECT ALL HEALTH CARE PROFESSIONALS TO INTERVENE • ASK ABOUT SMOKING STATUS APPROPRIATELY • OFFER MOTIVATIONAL INTERVIEW • DOCUMENT, DOCUMENT, DOCUMENT (TRACKING FORM, PROGRESS NOTES) MAKING HOSPITAL-WIDE SYSTEM LEVEL CHANGES THAT SUCCEED STEP 4: TRAIN ALL MD’s TO RESPOND • ASK ABOUT SMOKING STATUS APPROPRIATELY • OFFER STRONG, CREDIBLE MESSAGE ABOUT QUITTING • DETERMINE NEED FOR PHARMACOLOGICAL THERAPY • DOCUMENT, DOCUMENT, DOCUMENT (MEDICAL RECORD, TRACKING FORM) MAKING HOSPITAL-WIDE SYSTEM LEVEL CHANGES THAT SUCCEED STEP 5: CONSIDER A SYSTEM TO OFFER SELF-HELP MATERIALS AND BEHAVIORAL COUNSELING • STANDARDIZE PATIENT EDUCATION MATERIALS • UTILIZE CLOSED-CIRCUIT TELEVISION FOR VIDEOTAPES • DETERMINE WHO CAN BE TRAINED TO PROVIDE BEHAVIORAL COUNSELING (ie. VOLUNTEERS, CANDIDATE MEDICAL STUDENTS, CHAPLAINS, NURSES, PSYCHOLOGISTS) • PROVIDE A LIST OF COMMUNITY RESOURCES MAKING HOSPITAL-WIDE SYSTEM LEVEL CHANGES THAT SUCCEED STEP 6: DETERMINE A MECHANISM FOR FOLLOW-UP • USE SMOKING INTERVENTIONISTS TO UNDERTAKE PATIENT FOLLOW-UP • OFFER TELEPHONE CONTACT BY HEALTH CARE PROFESSIONALS ALREADY MAKING CALLS • INTEGRATE CALLS WITHIN PUBLIC HEALTH DEPT. • USE CENTRALIZED TELEPHONE SYSTEM FOR ALL SMOKERS WITHIN COMMUNITY • DOCUMENT, DOCUMENT, DOCUMENT Clinician’s Guide, Agency for Health Care Policy and Research Quit Smoking Action Plan, American Lung Association