this MS Word Document

To All Interested Parties:
As the nation continues to move toward a culture of affordable health coverage, we are witnessing phenomenal growth of state Medicaid programs. Due to the Medicaid expansion provisions of the Affordable Care Act, new beneficiaries and providers in state Medicaid programs are at record levels.
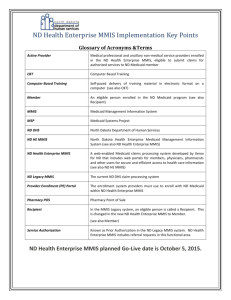
Governing magazine and the Center for Digital Government recognize the need to ensure that the required functions of
State Medicaid Management Information Systems (MMIS) are fully functioning and operating at increased levels of efficiency. However, MMIS modernization over the past 5 years has been challenging for state Medicaid Agencies as well as for the technology vendors under contract. We therefore see an opportunity to help state Medicaid Agencies that seek to move away from the traditional custom built MMIS solution. While existing CMS regulations and related
Federal statutes currently allow state Medicaid agencies substantial flexibility to seek innovative MMIS solutions that meet their evolving needs, according to a legal analysis by Covington and Burling, most states have not chosen to do so for a variety of reasons.
1
Over the next few months, Governing magazine and the Center for Digital Government will examine how CMS and state
Medicaid Agencies can add the simplified option of acquiring fiscal agent services where the system comes as part of the service. Referred to as Business Processes as a Service (BPaaS), this optional solution will provide all of the primary functions currently delivered by traditional MMIS solutions, e.g., integrated group of procedures and computer processing operations that meet the principal objectives of Title XIX plus much more. However, it will do so in a manner that leverages and somewhat resembles the administrative and medical management models of managed care health plans. Several Medicaid Agencies are already exploring this approach and refer to it as an Administrative Services
Organization (ASO) or Third-party Administrator (TPA). Importantly, this BPaaS optional solution is meant to be in alignment with CMS’ current enhanced federal financial participation (FFP) for MMIS replacement or modernization.
To help us ensure this effort serves CMS and state Medicaid Agencies, we are planning a series of meetings. These meeting will include representatives from both organizations as well as valued experts from the technology vendor and consultant community. Our primary task will be to develop a draft Medicaid Enterprise MMIS Certification Business
Area Checklist that leverages the concept of “conceptual equivalence” to arrive at a version of the Checklist suitable for
BPaaS certification for the purposes of states accessing enhanced FFP.
2 We believe once this task is completed, CMS and state Medicaid Agencies will then have a roadmap to pursue the BPaaS option as an alternative MMIS solution.
We would like to invite you to join us in this project. There will be at least two face-to-face meetings, one in
Washington, DC and the other in a location to be determined in the next few weeks. There will also be conference calls and document review sessions that will be conducted on-line. You can contribute as much or as little time as you have available and your support would be greatly appreciated.
We recognize the investment CMS and state Medicaid Agencies make in regard to MMIS replacement and/or modernization and the ongoing maintenance and operation of these systems. Governing magazine and the Center for
Digital Government look forward to working with CMS and the state Medicaid Agencies in the near future on this very timely and exciting project.
Governing magazine Center for Digital Government
1 Covington and Burling, LLP, “Re: Legal Analysis of a Medicaid “Managed Fee-for-Service” Model and a Medicaid Fee-for Service
Administrative Services Only (ASO) Model, (2013).
2 Op. cit, p. 3.