Advances in Hepatitis C Identification & Treatment
advertisement

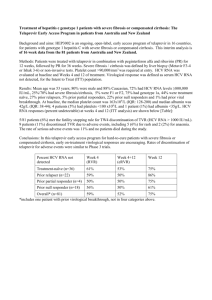
Advances in Hepatitis C Identification and Treatment Developed by Camilla S. Graham, MD, BIDMC, 5/5/15. cgraham@bidmc.harvard.edu. Slides can be selected or altered as needed. Disclosures 75% of People with Hepatitis C in the US are Baby Boomers Identifying Patients with Hepatitis C • 4-5 million people in the US have hepatitis C virus (HCV) infection – NHANES estimates 3.2 million infected but this national survey excludes people who do not have a permanent address (homeless, incarcerated, nursing home residents), active military, and under-represents most groups outside White, African-American, and Mexican-Hispanic – Accounting for under-represented international populations, homeless, and groups that have a high prevalence like IDU and veterans gives the 5+ million estimate • Most were infected in 1960’s through 1980’s – Up to 250,000 cases per year in 1980’s – About 50% infected via IDU, rest from blood transfusions, sex, tattoos, medical procedures, and other factors Smith BD et al. MMWR. August 17, 2012/61(RR04);1-18. Armstrong GL et al. Ann Intern Med. 2006 May 16;144(10):705-14. 4 http://www.iom.edu/Reports/2010/Hepatitis-and-Liver-Cancer-A-National-Strategy-for-Prevention-and-Control-of-Hepatitis-B-andC.aspx; Rein et al. Dig Liver Dis 2011; 43:66 Identifying Patients with Hepatitis C • Up to 75% of people have not been diagnosed – 50% to 75% is estimated • Risk-based screening misses many people – Overburdened primary care – Lack of knowledge for patients and providers – Stigma associated with IDU, even if decades ago • Leading cause for liver transplantation and liver cancer (HCC) − 37% lifetime risk of HCV-related mortality for patients with chronic HCV Smith BD et al. MMWR. August 17, 2012/61(RR04);1-18. Armstrong GL et al. Ann Intern Med. 2006 May 16;144(10):705-14. 5 http://www.iom.edu/Reports/2010/Hepatitis-and-Liver-Cancer-A-National-Strategy-for-Prevention-and-Control-of-Hepatitis-B-andC.aspx; Rein et al. Dig Liver Dis 2011; 43:66 Number People with Reactive anti-HCV Antibody Estimates of People with Hepatitis C in Use stateMassachusetts 200000 180000 160000 140000 120000 100000 80000 60000 40000 20000 0 specific Population age ≥18 in Massachusetts is 5,128,706 data found at http://ww w.nvhr.org /content/ nvhrHepatitis C hepatitisc-statespecificresourcesNHANES Adjust for Excluded Massachusetts DPH pages Groups United States Census Bureau 2010: Age and Sex Compositions (http://www.census.gov/prod/cen2010/briefs/c2010br-03.pdf; accessed 7/23/14); Ditah et al. J Hepatology 2014; 60:691 - NHANES HCV survey found 1.3% prevalence anti-HCV in US population age >18; Chak et al. Liver International 2011; 31:1090 - Adjustment for groups excluded from NHANES including homeless, incarcerated, active military and nursing home residents Number with chronic HCV (millions) Baby Boomers (Born in 1945–1965) Account for 76.5% of HCV in the US1 1.6 Estimated Prevalence by Age Group2 1.4 1.2 1.0 0.8 0.6 0.4 0.2 0 <192 0 1920s 1930s 1940s 1950s 1960s 1970s 1980s 1990+ Birth Year Group An estimated 35% of undiagnosed baby boomers with HCV currently have advanced fibrosis (F3-F4; bridging fibrosis to cirrhosis)3 7 1. Centers for Disease Control and Prevention. MMWR. 2012;61:1-32; Adapted from Pyenson B, et al. Consequences of Hepatitis C Virus (HCV): Costs of a baby boomer Epidemic of Liver Disease. New York, NY: Milliman, Inc; May 18, 2009. http://www.milliman.com/expertise/healthcare/publications/rr/consequences-hepatitis-c-virus-RR0515-09.php Milliman report was commissioned by Vertex Pharmaceuticals; 3. McGarry LJ et al. Hepatology. 2012;55(5):1344-1355. Who Should Be Tested for HCV CDC Recommendations USPSTF Grade B Recs* • • Everyone born from 1945 through 1965 (one-time) • Past or present injection drug use • Sex with an IDU; other high-risk sex • Blood transfusion prior to 1992 • Persons with hemophilia • Long-term hemodialysis • Born to an HCV-infected mother • Incarceration • Intranasal drug use • Receiving an unregulated tattoo • Occupational percutaneous exposure • Surgery before implementation of universal precautions • • • • • • • • Everyone born from 1945 through 1965 (one-time) Persons who ever injected illegal drugs Persons who received clotting factor concentrates produced before 1987 Chronic (long-term) hemodialysis Persons with persistently abnormal ALT levels. Recipients of transfusions or organ transplants prior to 1992 Persons with recognized occupational exposures Children born to HCV-positive women HIV positive persons 8 testing *Only pertains to persons with normal liver enzymes; if elevated liver enzymes need HBV and HCV Smith at al. Ann Intern Med 2012; 157:817-822. Moyer et al. Ann Intern Med epub 25 June 2013 Massachusetts Hepatitis C Testing Law: Section 138; Chapter 111 • Every person born between the years of 1945 and 1965 who receives health care services from a primary care provider shall be offered a hepatitis C screening test or a hepatitis C diagnostic test unless the provider believes that: (i) the person is being treated for a life threatening emergency; (ii) the person has previously been offered or has received a hepatitis screening test; or (iii) the person lacks capacity to consent to a hepatitis C screening test. 9 http://www.mass.gov/bb/gaa/fy2015/prnt_15/os_15/p138.htm Ms. Smith • 55 y/o woman followed for 12 years in primary care for anxiety and recently for menopause. Three years ago noted to have ALT 60 after estrogen replacement so switched to transdermal gel and follow up ALT 40. • Presented with URI and found to have Hgb 9.3 and platelets 81,000. Additional testing showed ALT 36, AST 82, Albumin 2.7, total bilirubin 1.0 and INR 1.2. 10 Ms. Smith • • • HCV antibody positive HCV RNA 16,500 Genotype 1a 11 Ms. Smith • • • CT abdomen with nodular liver, spleen 13.8 cm and small amount of ascites EGD with two grade 1 esophageal varices Hepatic encephalopathy? 12 Ms. Smith • Only possible “risk exposure” was foot surgery at a free-standing podiatry clinic in 1982 13 Chronic HCV Infection May Lead to Chronic Liver Disease and Liver Cancer Fibrosis Cirrhosis Hepatocellular Carcinoma (with cirrhosis) HCC3 Cancer of the liver can develop after years of chronic HCV infection Fibrosis1 Chronic HCV infection can lead to the development of fibrous scar tissue within the liver Decompensated cirrhosis: Cirrhosis1,2 Over time, fibrosis can progress, causing severe scarring of the liver, restricted blood flow, impaired liver function, and eventually liver failure Ascites Bleeding gastroesophageal varices Hepatic encephalopathy Jaundice Chronic liver disease includes fibrosis, cirrhosis, and hepatic decompensation; HCC=hepatocellular carcinoma. 1. Highleyman L. Hepatitis C Support Project. http://www.hcvadvocate.org/hepatitis/factsheets_pdf/Fibrosis.pdf. Accessed August 18, 2011; 2. Bataller 14 R et al. J Clin Invest. 2005;115:209-218; 3. Medline Plus. http://www.nlm.nih.gov/medlineplus/enxy.article/000280.htm. Accessed August 28, 2012; 4. Centers for Disease Control and Prevention. http://www.cdc.gov/hepatitis/HCV/HCVfaq.htm. Accessed May 8, 2012. Deaths Due to HCV Infections Now Exceed Those Due to HIV Infection Hepatitis C Rate per 100,000 Persons 7 HIV 16,600 deaths 6 5 4 3 2 1 0 1999 2000 2001 2002 2003 2004 2005 2006 2007 2008 2009 2010 Year Number of HCV-related deaths may be over 60,000 because of underreporting on death certificates Ly KN, Xing J, Klevens RM, Jiles RB, Holmberg SD. Causes of death and characteristics of decedents with viral hepatitis, United States, 2010. Clin Infect Dis. 2014 Jan;58(1):40-9. Mahajan, IDSA 2013 Projected Numbers of Decompensated Cirrhosis and Cases of HCC to Rise Through 2020 Timing of Mortality Among Known HCV Cases in Massachusetts, 1992-2009 1800 Median interval: 3 years Median age: 53 years Number of deaths 1600 1400 1200 1000 800 600 400 200 0 <1 1 2 3 4 5 6 7 8 9 10 11 12 13 14 Years to death from date of HCV diagnosis N=8,499 76,122 HCV diagnoses were reported to the MDPH between 1992 and 2009, 8,499 of these reported HCV cases died and are represented in the figure. Data as of 1/11/2011. 17 Lijewski, et al, 2012 15 16 17 Screening of Baby Boomers May Prevent >120,000 Deaths Due to HCV Infection 1,070,840 new cases of HCV identified with birth-cohort screening 552,000 patients treated 364,000 patients cured* 121,000 deaths averted† › Birth-cohort screening in primary care would identify 86% of all undiagnosed cases in the birth cohort, compared with 21% under risk based screening1 › Cost effectiveness of HCV screening is comparable to cervical cancer or cholesterol screening (cost/QALY gained with protease inhibitor+IFN+RBV = $35,700) Markov chain Monte Carol simulation model of prevalence of hepatitis C antibody stratified by age, sex, race/ethnicity, history of injection drug use, and natural history of chronic hepatitis C. *With pegylated interferon and ribavirin plus DAA treatment. †Deaths due to decompensated cirrhosis or hepatocellular carcinoma within 1945-1965 birth cohort. 470,000 deaths under birth cohort screening vs 592,000 deaths under risk-based screening 1. Rein D et al. Ann Intern Med. 2012;156(4):263-270; 2. McGarry LJ et al. Hepatology. 2012;55(5):1344-1355. 18 Efficient Identification of Hepatitis C in a Health Care Setting 19 BIDMC/CareGroup Experience • Network of academic hospitals, primary care practices, community health centers that share a common electronic medical record system – 5,500 clinicians and ~1.5 million patients • Implemented a prompt in EMR for a one-time anti-HCV test in all patients born from 1945-1965 who had no prior record of testing, while continuing risk-based testing – Went live on June 4, 2013 – In the first ten months, we tested a total of 20,000 people for HCV Steps to Implement Birth Cohort HCV Testing • Build a core team: Primary Care, Infectious Disease, Hepatology, Database Management, and Clinical Pathology • Implement a one-time electronic prompt for anti-HCV antibody testing for all patients born from 1945 through 1965 who have no record of HCV antibody testing • One-page educational tool for providers and one for patients (samples at KNOW MORE HEPATITIS/CDC and NVHR.org) • Email notification to affected clinicians • HCV nurse educator – Help facilitate patient referral in the Liver Center and Infectious Diseases Clinic • Slide deck for presentations to primary care providers about HCV (sample at NVHR.org) • Collaboration with Laboratory Services – Expand capacity for increased volume of HCV Ab and RNA tests – Add language to results page (or a second prompt) for all positive HCV antibody tests informing clinicians to order an HCV RNA test to determine the presence of active HCV infection – Generates a report of all positive HCV antibody tests for follow up Example for HCV testing p found at http://nv Initial Hepatitis C Testing and Evaluation Who Should Be Tested for Hepatitis C? New: Anyone born between 1945 and 1965 should be tested once, regardless of risk factors In addition, patients with the following risk factors: • Elevated ALT (even intermittently) • A history of illicit injection drug use or intranasal cocaine use (even once) • Needle stick or mucosal exposure to blood • Current sexual partners of HCV infected persons • Received blood/organs before 1992 • Received clotting factors made before 1987 • Chronic hemodialysis • Infection with HIV • Children born to HCV-infected mothers Why Test People Born Between 19451965? • 76% of the ~4 million people with HCV infection in the US are baby boomers • In the 1945-1965 cohort: • All: 1 out of 30 • Men: 1 out of 23 • African American men: 1 out of 12 • Up to 75% do not know they have HCV • 73% of HCV-related deaths are in baby boomers What Can Happen to People with Hepatitis C? • It is important to identify if patients have cirrhosis • Patients with cirrhosis are at risk for liver cancer (HCC) and liver decompensation (ascites, variceal bleed, hepatic encephalopathy, jaundice) • Hepatitis C is curable, and cure reduces the risk of severe complications, even with cirrhosis • Refer patients to a specialist who has experience treating hepatitis C to see if they need treatment Hepatitis C Antibody (HCV Ab)1 Negative (-) STOP here if no concern for acute infection or severe immunosuppression. If so, check HCV RNA. Positive (+) These people are NOT chronically infected. Check HCV RNA (viral load) Negative (-) • Positive (+) Detectable HCV Ab with negative HCV RNA can occur with spontaneous clearance of infection ( about 25% of people exposed to HCV will clear; verify HCV RNA negative in 4 to 6 months) or with treatment of HCV. Hepatitis C infection 1Example Evaluation and referral ICD-9 codes for HCV antibody testing: • V73.89: screening for other specified viral disease • 790.4: nonspecific elevation of levels of transaminase; use if patient ever had an elevated ALT Counsel Patients with HCV Infection About Reducing Risk of Transmission • Do not donate blood, body organs, other tissue, or semen • Do not share personal items that might have small amounts of blood (toothbrushes, razors, nail-grooming equipment, needles) and cover cuts and wounds • HCV is not spread by hugging, kissing, food or water, sharing utensils, or casual contact • If in short term or multiple relationships, use latex condoms. No condom use is recommended for long-term monogamous couples (risk of transmission is very low) Initial Management • Evaluate alcohol use (CAGE, AUDIT-C) and recommend stopping use • Vaccinate for hepatitis A and hepatitis B if not previously exposed • Evaluate sources of support (social, emotional, financial) needed for HCV treatment 23 Smith BD et al. MMWR. August 17, 2012/61(RR04); 1-18. Adapted from Winston et al. Management of hepatitis C by the primary care provider: Monitoring guidelines; 2010; http://www.hcvadvocate.org/hepatitis/factsheets_pdf/PCP_web_10.pdf PCP Education Example: Screening in Clinic 1,000 adult patients Efficiently identify birth cohort 19451965: • Electronic prompt 330 baby boomers ~1/3 of adults are in 19451965 cohort 10 HCV antibody positive • • • 1 of 30 baby boomers 1 of 23 men baby boomers 1 of 12 African American men baby boomers 7 HCV RNA positive 3 with more advanced fibrosis 4 with mild fibrosis 15%-30% of HCV antibody patients will spontaneously clear Up to 25% of baby boomers may have cirrhosis 75% of cirrhotic patients are men 24 Davis, Gastro 2010; 138: 513 Number of HCV Antibody Tests Performed In Four Week Intervals 2500 2000 1500 Total Tests 1000 Boomers Non-Boomers 500 3/1/2014 1/1/2014 11/1/2013 9/1/2013 7/1/2013 5/1/2013 3/1/2013 1/1/2013 11/1/2012 9/1/2012 7/1/2012 5/1/2012 3/1/2012 1/1/2012 0 Beth Israel Deaconess Medical Center, Boston, MA, Quality Outcomes Data, 1/22/14 HCV Antibody Test Volume Increased after EMR Prompt Boomers Average = 1192 tests/4 weeks 1600 EMR prompt 1400 1200 CDC 19451965 testing guidelines 1000 800 600 Average = 303 tests/4 weeks Average = 438 tests/4 weeks Boomers 400 200 3/1/2014 1/1/2014 11/1/2013 9/1/2013 7/1/2013 5/1/2013 3/1/2013 1/1/2013 11/1/2012 9/1/2012 7/1/2012 5/1/2012 3/1/2012 1/1/2012 0 Beth Israel Deaconess Medical Center, Boston, MA, Quality Outcomes Data, 6/5/14 More Women Tested for HCV but More Men are Anti-HCV Positive Group Number (%) Tested for HCV Ab Anti-HCV Seroprevalence (%) 13,107 2.3% Boomer women 7,555 (58%) 1.4% (34% of HCV Ab+ results) Boomer men 5,552 (42%) 3.6% (66% of HCV Ab+ results) 7,022 2.6% Non-Boomer women 4,023 (57%) 1.9% (42% of HCV Ab+ results) Non-Boomer men 2,999 (43%) 3.5% (58% of HCV Ab+ results) All Boomers All Non-Boomer Beth Israel Deaconess Medical Center, Boston, MA, Quality Outcomes Data, 6/5/14 Initial Approach to Patients Diagnosed with Hepatitis C Hepatitis C Diagnosis has been Made: What to Discuss with the Patient • Do not donate blood. May donate organs to others with HCV • Do not share personal items that might have small amounts of blood – Toothbrushes, razors, nail-grooming equipment • HCV is not spread by hugging, kissing, food or water, sharing utensils, or casual contact • If using illicit drugs, stop using. If continued, get into a treatment program and do not share needles, syringes or works – • Concern among payers about poor adherence and reinfection after antiviral Rx If in short term, multiple or MSM relationships, use latex condoms. No condom use is recommended for long-term monogamous heterosexual couples – Maximum incidence rate of HCV sexual transmission estimated about 1 new infection per 190,000 sexual contacts per year (Terrault, Hepatology. 2013; 57(3):881) • Limit Tylenol to 2 gm a day and discuss all other medications (including OTC and herbal ) with a provider • Check exposure status for hepatitis A and B and vaccinate if needed Adapted from Winston et al. Management of hepatitis C by the primary care provider: Monitoring guidelines; 2010 http://www.hcvadvocate.org/hepatitis/factsheets_pdf/PCP_web_10.pdf Address Alcohol Use in HCV • • • • The CDC recommends brief alcohol intervention for all patients with HCV There is no “safe” amount of alcohol consumption Insist on absolute abstinence if patient has bridging fibrosis or cirrhosis Assess for risky alcohol use – Men: >2 drinks/day (>14/week) or more that 4 in one day – Women: >1 drink/day (>7/week) or more than 3 in one day • Screen for alcohol misuse – How many times in the past year have you had X or more drinks in a day?”, where X is 5 for men and 4 for women, and a response of >1 is considered positive http://www.integration.samhsa.gov/images/res/tool_auditc.pdf 30 Moyer et al. Screening and Behavioral Counseling Interventions in Primary Care to Reduce Alcohol Misuse: USPSTF Recommendation Statement. Annals Int Med; 14 May 2013 online Baseline Labs in Patients with Newly Diagnosed HCV • HCV RNA “viral load” (determines active infection) • Hepatitis C genotype (determines treatment choice) • Complete blood count (platelets <150,000 assc with cirrhosis) • INR, Albumin, Total bilirubin (abnormal liver synthetic function often indicates advanced liver disease) • Creatinine, Glucose, ALT, AST, Alkaline Phosphatase • Hepatitis A serology: total or IgG (vaccinate if nonreactive) • Hepatitis B serology: HBsAb, HBcAb, HBsAg (vaccinate if all nonreactive) • HIV antibody • Iron studies, ANA • Assessment of liver fibrosis (such as Hepascore, Fibrotest, APRI, FIB-4, Fibroscan) 31 BIDMC HCV ECHO Program Recommendations, 2014 Distribution of Fibrosis Scores • • • • • F0 = 15% F1 = 25% F2 = 20% F3 = 15% F4 = 25% Recently infected and slow progressors “Advanced fibrosis • Limits of fibrosis tests: – Liver biopsies are +/- 1 fibrosis stage – Noninvasive tests are best at determining a high versus low probability of advanced fibrosis 32 Determine Likelihood of Cirrhosis • Noninvasive test results increase the likelihood of cirrhosis, especially if more than one are present: – APRI >1.5 or FIB-4 >3.25 (use on-line calculators) • FIB-4 more predictive of ESLD than liver biopsy (CROI 2014) – – – – Hepascore or Fibrotest >0.74 Fibroscan >12.5 Platelets <150,000 Albumin < 3.5 • Splenomegaly on exam or ultrasound • Any signs of liver decompensation • MELD and Child-Pugh scores (use on-line calculators) Chou, Annals Int Med 2013; 158:807; Bonder, Curr Gastro Rep 2014; 16:372; Berenguer #640 and Lo Re #650 CROI 2014 FibroScan - Transient Elastography • Ultrasound determines velocity of shear wave in m/s, which is proportional to liver stiffness in kilopascal (kPa) • Entire process requires 15 to 20 minutes, provides immediate results • Falsely elevated results: – High ALT (>100) – Eating within 2 hours Bonder, Curr Gastro Rep 2014; 16:372 ALV 10.7.13 Continuum of Fibrosis/Cirrhosis in HCV <7 kPa = Stage 0-1 7-9.5 kPa = Stage 2 9.5-12.5 kPa = Stage 3 >12.5 kPa = Cirrhosis >20 kPa = Increased risk liver-related complications Continuum of scores (in kPa) Bonder, Curr Gastro Rep 2014; 16:372 70+ kPa Management of Patients with Hepatitis C and Cirrhosis 36 • Every 6 month screening for liver cancer • Usually ultrasound • Consider CT or MRI if highly nodular liver; first exam • Screening for esophageal varices • Repeat every 1 -3 years depending on results • Counsel on symptoms of hepatic encephalopathy • Vaccination for pneumococcus • Counseling around medication use to avoid overdose or adverse events (including common drugs like Tylenol and NSAIDS) • Counseling about complete abstinence from alcohol • Evaluation for antiviral treatment • Cure of HCV can reduce liver failure and liver cancer, even in patients with cirrhosis (+/- HIV coinfection) • Possible referral for liver transplant services http://www.aasld.org/practiceguidelines/pages/guidelinelisting.aspx 10-year Cumulative Incidence Rate SVR (Cure) Associated with Decreased All-Cause Mortality 29.9 26 21.8 8.9 Van der Meer et al. JAMA 2012; 308:2584 5.1 2.1 530 patients with advanced fibrosis, treated with interferonbased therapy, and followed for 8.4 (IQR 6.4-1.4) years Recent Treatment Data and Guidelines Slide 39 of 30 The World is Rapidly Changing in HCV • • • • • • • • • • Pegylated interferon (Peg-IFN) + ribavirin (RBV) Peg-IFN + RBV + Telaprevir Peg-IFN + RBV + Boceprevir Peg-IFN + RBV + Simeprevir Sofosbuvir+Ledipasvir x 8 weeks Paritaprevir/r/ombitasvir+dasabuvir+/-RBV x 12 weeks Sofosbuvir +RBV x 12 weeks Sofosbuvir+Ledipasvir x 12 weeks Sofosbuvir+Simeprevir x 12 weeks Paritaprevir/r/ombitasvir+dasabuvir+/-RBV x 24 weeks (geno 1a cirrhotic [F3-F4] null [non-] responders?) • Sofosbuvir+RBV x 24 weeks • Sofosbuvir+Ledipasvir x 24 weeks • Sofosbuvir+RBV x 48 weeks Slide 40 of 30 Percent SVR SVR in Genotype 1, Naïve, Non-cirrhotic Patients Treated with Sofosbuvir+Ledipasvir (ION-3) 100 90 80 70 60 50 40 30 20 10 0 97% 90% 96% 96% 119/ 123 83/ 92 126/ 131 82/ 85 8 wks VL <6 mil 8 wks VL > 6 mil 12 wks VL <6 mil Harvoni package insert, 10/11/14 12 wks VL >6 mil 40 Slide 41 of 30 Key Points with Sofosbuvir+Ledipasvir • Most common AEs are fatigue and headache • Taken with or without food • Ledipasvir needs acid for solubility/absorption – Be careful with OTC acid blockers (TUMS, Rolaids, Mylanta, calcium supplements, as well as proton pump and H2) • eGFR >30 mL/min/1.73m2 • No dose adjustment for Child-Pugh Class A, B, or C cirrhosis • Pregnancy Class B • Avoid P-gp inducers; see all other DDI data in PI 41 Harvoni package insert, 10/11/14 Slide 42 of 30 SVR-12 in Genotype 1 Patients Treated with Paritaprevir/r+Ombitasvir+Dasabuvir +/- RBV (3-D) Naïve, no cirrhosis, Geno 1b: Viekira Pak x12 wks Percent SVR Naïve, no cirrhosis, Geno 1a: Viekira Pak+RBV x12 wks Naïve, cirrhosis, Geno 1a or 1b: Viekira Pak+RBV x12 wks Peg-IFN/RBV failure, Geno 1b: Viekira Pak+RBV x12 wks N=473 N=297 N=209 N=91 N=100 N=208* Feld; NEJM 2014 Apr 11; Zeuzem; NEJM 2014 Apr 10; Poordad NEJM 2014 Apr 12 Peg-IFN/RBV failure , Geno 1a: Viekira Pak+RBV x 24 wks (may use 12 wks if relapse, or no cirrhosis) Slide 43 of 30 Compare Key Attributes of Harvoni vs. Viekira Pak Harvoni Viekira Pak SVR ≥95% with correct duration SVR ≥92% with correct duration (may have better efficacy in geno 1b) Very well tolerated Needs monitoring for anemia, dose reduce RBV (<10%) Pts with decompensation and post-Tx need RBV 85% of patients need RBV One pill once a day 10 pills a day (if require generic RBV) 8 to 12 week duration 12 to 24 week duration Can use with Child B and C Cannot use with Child B and C Common DDIs: HIV meds, acid blockers Common DDIs: HIV meds, Estradiol, fluticasone, salmeterol, some statins Fail with NS5A resistance Fail with 3-drug class resistance 43 Genotype 2 Naïve, with or without cirrhosis or Treatment experienced, no cirrhosis Sofosbuvir+RBV x 12 weeks Treatment experienced, with cirrhosis Sofosbuvir+RBV x 12-16 weeks 2014 IDSA/AASLD Recommendations: www.hcvguidelines.org Sofosbuvir+PegIFN+RBV x 12 weeks Percent SVR SVR in Genotype 2 Patients Treated with Sofosbuvir+Ribavirin for 12 Weeks Treatment experienced, cirrhotic patients only had a 78% SVR with 16 weeks SOF+LDV. May wait for sofosbuvir + daclatasvir EASL 2014 Genotype 3 Naïve, with or without cirrhosis or Treatment experienced, no cirrhosis Sofosbuvir+RBV x 24 weeks Sofosbuvir+PegIFN+RBV x 12 weeks www.hcvguidelines.org Treatment experienced, with cirrhosis Sofosbuvir+PegIFN+RBV x 12 weeks Sofosbuvir+Ledipasvir + RBV x 12 weeks? Sofosbuvir+Daclatasvir (Compassionate use until Sofosbuvir+RBV x 24 weeks FDA approval) Slide 47 of 30 Hypothetical Costs of Not Optimizing SVR Rates in Clinical Practice 95% SVR in clinical trials 85% SVR in real world 10% difference in SVR rates for a $100,000 regimen result in: •$12,384 “loss $ per unachieved cure” for each patient •Cost of retreating all patients who did not achieve SVR •Costs of liver complications (decompensation, liver cancer, etc.) in those who are not cured and progress Slide 48 of 30 HCV Treatment Initiation: BIDMC Example • Assess patients for readiness, insurance status, and fill out clinical assessment form • Deliver the 1st fill of medication to provider office only • Require teaching visit with clinical staff prior to starting treatment • Document true start date and inform Specialty Pharmacy • Set up ALL follow-up and lab appointments right after teaching visit • Provide teaching handout and list of appointments to patient • Utilize pill box / blister pack / smart phone reminder apps to enhance medication compliance • Specialty pharmacy with weekly or biweekly phone call to patients for follow up assessment • Adopt a real time tracking system (ie, TrioHealth) – Record patient baseline characteristics and treatment regimen – Prompt for wk 4, wk 12 viral load and SVR12 due dates – Method of communication for provider office and specialty pharmacy Pricing and Reimbursement Current Negative Environment Created By High Price of HCV Drugs • • • • • • • • • • • • • Confusion and doubt among HCV treaters Fear from PCPs about testing and treatment Fear/outrage among payers (public and private) Hesitation in DPH/public outreach programs Questions about integrity of CDC work (research and KNOW MORE HEPATITIS campaign) Declarations by prisons, state Medicaids that HCV treatment is not of value Difficulty establishing broad baby boomer testing programs Rationing of treatment, ie F3-F4; substance use Conflict between provider, patient and payer over rationing No discussion of cure-as-prevention Justification for overt discriminatory practices like mandating clean urine samples Confirmation by patients that they are not “worth” treatment Loss of vision about transformative, curative developments HOW DID WE GET INTO THIS MESS? Unique Aspects of Hepatitis C • Relatively common disease • Majority of people infected 20 – 40 years ago (75% in 1945-1965 birth cohort) • Peak of severe liver complications expected to occur over this next decade, so urgency to identify and treat people soon • Everyone who has >1 year life expectancy is theoretically a treatment candidate • Pricing more similar to treatments for rare diseases “Standard of Care” Regimens for Hepatitis C Have Been Expensive for Years: Examples for Treatment of Genotype 1, Naïve, Non-Cirrhotic Patients Regimen Pegasys + Ribavirin x 48 weeks1 Telaprevir + PegIFN + Ribavirin x 24 weeks2 Sofosbuvir + PegIFN + Ribavirin x 12 weeks Sofosbuvir+Ledipasvir x 8 weeks Sofosbuvir + Ledipasvir x 12 weeks SVR rates WAC Price Cost per SVR 41% $41,758 $101,849 75% $86,843 $115,791 90% $94,421 $104,912 94% $63,000 99% $94,500 $67,021 ($36,191?)* $95,454 ($51,545?)* Package inserts for products; *http://blogs.wsj.com/pharmalot/2015/02/04/what-the-shocking-gilead-discounts-on-itshepatitis-c-drugs-will-mean/ Cost-Effectiveness of HCV Treatment Study Key Findings Leidner, Hepatology 2015 For 55 y/o treated with $100,000 regimen and SVR = 90%, treating at F2 compared to waiting until F3 had CE = $37,300/QALY Threshold cost for treating at F0 versus waiting until F1 to yield $50,000/QALY = $22,200 Rein, CID 2015 Harvoni and Viekira Pak compared to no treatment yields $32,000 to $35,000/QALY Compared to no treatment, threshold cost for treating F0 with all-oral regimen = $47,000 Najafzadeh, Annals Int Med 2015 Compared to no treatment in genotype 1, costs per additional QALY gained for Harvoni = $25,291 and Peg-IRN/RBV = $24,833 If Harvoni <$66,000/treatment course, would be cost saving Chhatwal, Annals Int Average ICER for sofosbuvir-based treatment compared to prior Med 2015 SOC = $55,378/QALY Range = $9,703/QALY for naïve, cirrhotic geno 1 to $410,548 for treatment experienced, geno 3 without cirrhosis Payer Dilemmas • Most payers had no idea how much they were actually spending per treated patient (or per cure) in the interferon era – PI/P/R in cirrhotic patients ~ $266,000 per cure1 • Pharmacy budgets often separate from medical budgets – Pharmacy budgets don’t get “credit” for avoidance of medical costs – Annual budgets • “Is it cost effective?” (off-sets over the long term) • “Is it affordable?” (costs over one year) 1Sethi, AASLD 2013 Slide 56 of 30 Medical Need Restriction • Advanced fibrosis (Metavir F3-F4) – Evidenced by liver biopsy, transient elastography, Fibrotest, APRI or FIB-4 score, radiological imaging consistent with cirrhosis, physical findings or clinical evidence consistent with cirrhosis as attested by the prescribing physician Slide 57 of 30 Response to Restricting Treatment to F3/F4 • Cannot require liver biopsy (may be highest risk of death in HCV care with all-oral regimens) • Since no test can perfectly distinguish F2 from F3 or F3 from F4, limiting access to F3/F4 really means directing treatment to cirrhotic patients • If we wait until advanced fibrosis, need to do lifelong screening for HCC every six months even if cured (expense, logistics, patient anxiety) • Prioritization of F2-F4 unless other compelling urgency may align with provider capacity Community Network in HCV Departments of Public Health Academic Centers Slide 58 of 30 ECHO Community Health Centers Government Policy Makers Prisons Private Primary Care Centers Media Patient Advocacy Organizations Community Gastroenterology Commercial Payers Pharmacies Government Payers Pharmaceutical Companies Slide 59 of 30 Resources • IDSA/AASLD/IAS–USA HCV Guidance • Federal guidelines (VA, prison system) • National Viral Hepatitis Roundtable – Collects templates, sample slide presentations, analyses of state and federal policies – Program assistance with 1945-1965 birth cohort testing – www.NVHR.org