ADVANCED INTERVENTIONAL PAIN
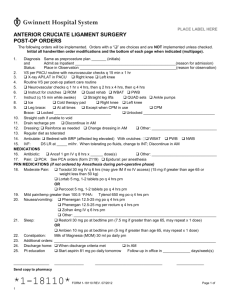
advertisement

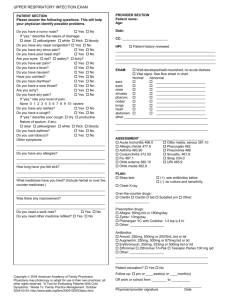
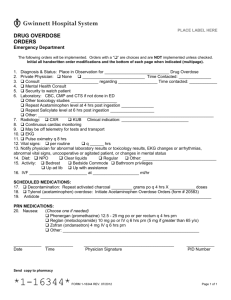
ADVANCED INTERVENTIONAL PAIN CONSULTANTS Follow Up Visit Name _______________________________ Date of Birth __________ Age ____ Date ____________ PRIMARY CARE DOCTOR ___________________ CHIEF PAIN COMPLAINT REFERRING PHYSICIAN _______________________ Back Neck Headaches Muscles Joints Shoulder Hip Knee HISTORY OF PRESENT ILLNESS How are you doing since your last visit? ___ Improved ___ No change ___ Worse Explain: ______________________________ Where is your pain located? Draw How intense is your pain? Circle the lowest and highest How do you best describe your pain? ___Dull ___Electrical ___Stabbing ___Burning ___Aching ___Throbbing ___Shock-like ___Sharp What is the pattern of your pain? ___ Constant ___ Intermittent ___ Mornings ___ Afternoons ___ Nights Does the pain radiate to other areas? ___Yes ___No If yes, where? ____________________________ Any associated symptoms? ___ Numbness ___ Weakness ___ Muscle spasms ___ Tingling Where are you headaches located? Draw Fill this part only if you are being consulted for HEADACHES How many headaches did you have last month? _____ How do they usually last? ________________ The intensity of the headaches is ___ better ___ worse ___ same Have the medications we prescribed caused any of the following SIDE EFFECTS? (Circle all that apply) Nausea Vomiting Itchiness Constipation Drowsiness Sweating Loss of libido Weight gain Swelling Since your last visit, have you had a PAIN INJECTION? ___Yes ___No If yes, how much PAIN RELIEF did you obtain with the injection? None 10% 20% 30% 40% 50% 60% 70% 80% 90% 100% Have you had PHYSICAL THERAPY in the last 6 months? ___ Yes ___ No Date_________________ Did it help? ___ Yes ___ No Has the TREATMENT you are receiving improved any of the following aspects of your life? Activities of daily living ___ Yes ___ No Relations with people Ability to work ___ Yes ___ No Sleeping/rest Family life ___ Yes ___ No Depression/anxiety ___ Yes ___ Yes ___ Yes ___ No ___ No ___ No Overall, has the treatment you are receiving made a positive change in your condition? ___ Yes ___ No 1 Are you ALLERGIC or sensitive to any medications? ___ No ___ Yes List ___________________________________________ List all OTHER MEDICATIONS you are currently taking. Include pain creams. Include dose and times per day taken 1) 2) 3) 4) 5) ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ ________________________________________________ 6) _______________________________________________ 7) _______________________________________________ 8) _______________________________________________ 9) _______________________________________________ 10) _______________________________________________ Do you take any blood thinners? ___ No ___ Yes OPIOID ATTESTATION I attest and certify that all of the following statements are true and factual: ___ I have used all medications prescribed to me exactly as prescribed. ___ I have reported all side effects to my physician. ___ I have not sold, given to someone else, or otherwise transferred my medications to anyone. ___ I have safeguarded my medications from theft. ___ I have not received, accepted, taken, or otherwise used any other opioid medications (narcotics) from any other source, including from other physicians. ___ I have not received, accepted, taken, or otherwise used any illegal drugs. ___ I have not used alcohol while taking my opioid medications (narcotics). Patient‘s Signature _________________________________ MEDICAL HISTORY Has your medical history changed since your last visit, including ER visits and hospitalizations? ___No ___Yes Explain __________________________________________________________________________________________________ ________________________________________________________________________________________________________ SURGICAL HISTORY Have you had surgery since your last visit? ___ No ___ Yes, explain _______________________________ _________________________________________________________________________________________________________ Do you smoke? ___ No ___ Yes, packs per day ____ Are you under psychiatric care or receiving counseling? ___ No ___ Yes REVIEW OF SYSTEMS Circle all that apply 1. General 2. ENT Weight gain or loss, unexplained hair loss, fever or chills, low energy, too sleepy, too tired Eye pain, vision problems (blurred vision, loss of vision), hearing loss, swollen glands in neck, sore throat/pain when swallowing, dental problems Chest pain (sharp, crushing, or heaviness), heart racing (palpitations), fainting spells, shortness of breath, swelling of legs (edema) Shortness of breath, cough/coughing up blood Increased appetite, decreased appetite, stomach pain, nausea/vomiting, diarrhea, constipation Pain when passing water (urination), blood in urine, urinating more than usual (day and/or night), bladder Infection, pain during sex, changes in sex drive (libido) Limited motion of arms or leg, joint pain, swelling/redness, numbness, tingling, or weakness in arms or legs Arm/leg weakness, new headaches, problems with memory or speech, tremors Sadness, stress, anxious, seeing or hearing things, suicidal thoughts, feeling down, insomnia Weight gain/loss, thirsty all the time, cannot stand temperature changes (heat/cold) Swollen glands (armpits or groin) Rash (palm of hands, sole of feet), changes in skin, sores or rash on skin Hives/skin rashes, allergic reaction to foods 3. Cardiovascular 4. Respiratory 5. Gastrointestinal 6. Genitourinary 7. Musculoskeletal 8. Neurological 9. Psychiatric 10. Endocrine 11. Lymph 12. Skin 13. Allergies ____ No new problems SLEEP APNEA SURVEY ___ Excessive loud snoring ___ Gasping or choking for breath while sleeping ___ Tired after sleeping ___ Falling asleep and daytime tiredness ___ Witnessed respiratory pauses ___ Night time difficulties ___ Have high blood pressure I attest that all of the information I have provided is accurate and factual, and I can provide supporting information. Patient‘s Signature __________________________________ 2 PHYSICAL EXAM VITAL SIGNS HR ______ BP ____________ RR ______ Weight _________ Height _________ BMI _______ GENERAL ___ Alert ___ Somnolent ___ Calm ___ Distressed ___ Pain behavior ___Clear speech ___ Pupils are round and equal, patient used adequate respiratory efforts and pulses are present MUSCULOSKELETAL ___ Cane ___ Walker ___ Wheelchair ___ Brace ___ Sling Inspection: Area _____________________ ___ Asymmetry ___Scars ___Atrophy ___ Scoliosis deformity ___ Kyphosis deformity ___ Midline posterior lumbar/cervical scar(s) ___ Anterior abdominal scar ___ Anterior neck scar Palpation: Tender or trigger point areas and/or muscle spasm ___ Masseters ___ Supraspinatus ___ Gluteus max ___ Splenius capiti ___ Infraspinatus ___ Gluteus med ___ Semispinalis ___ Rhomboid ___ Piriformis ___ Trapezius ___ Latissimus ___ > 11/18 tender ___ Deltoid ___ Paraspinalis points (FM) ROM: NEURO Facet joints pain/positive facet joint loading test ___ C2-3 ___ T1-2 ___ T7-8 ___ L1-2 ___ C3-4 ___ T2-3 ___ T8-9 ___ L2-3 ___ C4-5 ___ T3-4 ___ T9-10 ___ L3-4 ___ C5-6 ___ T4-5 ___ T10-11 ___ L4-5 ___ C6-7 ___ T5-6 ___ T11-12 ___ L5-S1 ___ C7-T1 ___ T6-7 ___ T12-L1 Painful areas ___ Supraorbital ___ Temporal ___ Occipital ___ AC Joint ___ Greater trochanter ___ Infrapatellar ___ IT Band ___ Suprapatellar ___ SIJ Pain ___Lumbar ___Cervical ___Thoracic ___Hip ___Shoulder ___Knee ___Ankle ___Elbow ___ Flexion ___ Flexion ___ Flexion ___ Flexion ___ Flexion ___ Flexion ___ Flexion ___ Flexion ___ Extension ___ Extension ___ Extension ___ Extension ___ Extension ___ Extension ___ Extension ___ Extension ___ Distraction ___ Thigh Thrust ___ Compression ___ Gaenslen ___ Faber ___ SIJ 3/5 Positive ___ Rotation ___ Lateral Bend ___ Rotation ___ Lateral Bend ___ Rotation ___ Lateral Bend ___ Patrick-Faber (Hip/SIJ) ___ Resisted Abd Release (GT bursa) ___ Abd ___ Add ___ Internal/External rotation ___ Drop Arm Test (RCT) ___ACL-PCL Drawer ___ MCL Test ___LCL Test ___ McMurray’s (meniscus) ___ Inversion ___Eversion ___ AAO x 4 ___ CN 3-12 intact ___ Normal Gait ___ Cerebellar function test normal (nose-finger-nose) ___ Normal motor function (5/5) ___ Normal deep tendon reflexes (2/4) ___Normal sensory function ___Allodynia ___Hyperalgesia ___Edema ___Erythema ___Cyanosis ___Cold/warm ___Hair pattern ___Skin ___ Abnormal motor function Right Arm flexion/deltoid abd (C5) ___/5 Writs extension (C6) ___/5 Arm extension (C7) ___/5 Hand grip (C8) ___/5 Hip flexion (L2, 3) ___/5 Knee extension (L4) ___/5 Ankle dorsiflexion (L5) ___/5 Ankle plantar flexion (S1) ___/5 Left ___/5 ___/5 ___/5 ___/5 ___/5 ___/5 ___/5 ___/5 ___ Abnormal deep tendon reflexes Biceps (C5) ___/4 Brachioradialis (C6) ___/4 Triceps (C7) ___/4 Patellar (L4, 5) ___/4 Achilles (S1) ___/4 ___/4 ___/4 ___/4 ___/4 ___/4 ___ Decrease light touch/pin prick sensation ___ Cervical axial loading test (disc) ___ Lumbar axial loading test (disc) ___ SLR Right Left ___Spurling Right Left 3 NEW MEDICAL RECORDS: ___Reviewed ___Not Available MRI: Date ________ ___ Reviewed XRAY: Date _________ ___Reviewed CT SCAN: Date ________ ___Reviewed EMG: Date _________ ___ Reviewed URINE DRUG TEST Date: ______________ ___ Passed ___ Failed Inclinometry and muscle strength test: ___ Done today ___ Reviewed SOAAP-R Score: PMQ-R Score: DEPRESSION Score: DPS Report: SLEEP APNEA Survey: ____ ____ ____ ____ Reviewed ____ Done ASESSEMENT: ___ Stable medication regimen ___ Adequate analgesia ___ Adequate level of activity ___ No abuse, misuse, aberrant, addiction behavior ___ No significant/significant side effects ___ Rotate to a different opoid _______________________________ ___ Increase/decrease total dose ___ Start weaning opioid off ___ Low/average/high risk ___ Violation of medication contract LUMBAR ___ Lumbalgia ___ Facet arthralgia/arthritis ___ Spondylosis ___ DDD ___ HNP ___ Radiculopathy ___ Stenosis ___ Pseudoclaudication ___ Listhesis ___ Scoliosis ___ FBSS ___ Compression fracture ___ Foraminal stenosis CERVICAL ___ Cervicalgia ___ Facet arthralgia/arthritis ___ Spondylosis ___ DDD ___ HNP ___ Radiculopathy ___ Stenosis ___ Listhesis ___ Kyphosis ___ FBSS ___ Foraminal stenosis THORACIC ___ Thoracalgia ___ Facet arthralgia/arthritis ___ Spondylosis ___ DDD ___ HNP ___ Radiculopathy ___ Stenosis ___ Scoliosis ___ Kyphosis ___ Compression fracture ___ PTPS ___ PMPS ___ Costochonditits HEAD ___ Cervicogenic headaches ___ CDHA ___ Migraine ___ Occipital neuralgia ___ Supraobital neurlagia ___ Trigeminal neuralgia ___ Central pain ___ Seizures ___ CVA/TIA ___ TMJ syndrome ___ Atypical facial pain PELVIS ___ Hip pain ___ Hip arthritis ___ Trochanteric bursitis ___ Piriformis syndrome ___ SIJ pain ___ Sacroilitis ___ SIJ dysfunction ___ Coccygodynia ___ Pelvic pain syndrome ___ Interstitial cystitis ___ Vulvodynia ___ Genital pain ___ Endometriosis JOINTS ___ Shoulder pain ___ Shoulder arthritis ___ RC impingement ___ Rotator cuff strain ___ Rotator cuff tear ___ AC arthritis ___ SA bursitis ___ Knee pain ___ Knee arthritis ___ MCL LLC ACL/PCL ___ Meniscus tear (M/L) ___ Elbow pain/arthritis ___ Foot/ankle pain ___ Synovial bursa tendon ___ Hand/wrist arthritis NERVES/MUSCLES ___ Fibromyalgia ___ Myofascial pain syd ___ Muscle spasms ___ CRPS arm ___ CRPS leg ___ Neuralgia/neuritis ___ Polyneuropathy idiopathic ___ DPN ___ PHN ___ CTS ___ Phantom pain syd ___ Neuroma ___ Paraplegia ___ Meralgia ___ Post-polio syd ___ Multiple sclerosis CONNECTIVE ___ Osteoarthritis ___ Osteoposis ___ Rheumatoid arthritis ___ Psoriatic arthritis ___ Ankylosing Spondylitis ___ Sjogren’s ___ SLE ___ Enhlers Danlo’s syndrome ___ Raynaud’s ___ Enthesopathy ___ Plantar fasciitis ___ IT band pain/fasciitis ___ Thoraco-scapular syndrome VARIOUS ___ Abdominal pain ___ Chronic pancreatitis ___ PAD ___ Ischemic pain ___ Adhesions ___ Post-surgical pain ___ Tumor pain ___ Kidney pain ___ Obstructive sleep apnea PSYCH ___ Depression ___ Anxiety ___ Bipolar ___ PTSD ___ Alcohol dependence ___ Drug dependence ___ Drug withdrawal ___ Chronic pain syndrome ___ Insomnia ___ Drug abuse/misuse 4 TREATMENT PLAN: The goal of treatment is/are ___ pain relief, ___ optimize medication use, ___ improve function. 1. ___Pharmacologic therapy: ___ Medication’s risks (side effects) and benefits were discussed with patient. OPIOIDS Post date _________________ Refills ___ Tylenol 3 4 1 ________ # ____ PRN Tramadol 50 mg 1 ________ # ____ PRN Oxycodone 5 10 15 30 mg 1 _______ # ____ PRN Opana 5 10 mg 1 ________ # ____ PRN Hydromorphone 2 4 8 mg 1 ________ # ____ PRN Tapentadol 50 75 100 mg 1 q6 hrs # ____ PRN Morphine IR 15 30 mg 1 ________ # ____ PRN Hydrocodone 5 7.5 10 mg 1 ________ # ____ PRN APAP 325 Butrans 5 10 15 20 mcg/hr 1 q 7 days # ____ Ultram ER 100 200 mg 1 qd # ____ MUSCLE RELAXANTS PRN MUSCLE SPASM Refills ____ Tizanidine 2 4 6 mg 1 qHS bid tid # ____ Flexeril 5 10 mg 1 qHS bid tid # ____ Soma 250 350 mg 1 qHS bid tid qid # ____ Baclofen 10 20 mg ½ 1 tid # ____ Methocarbamol 500 750 mg 1 tid qid # ____ ANTI-INFLAMMATORIES Refills ____ Etodolac 400 mg 1 q12 hrs # ____ Ibuprofen 800 mg 1 q8 hrs # ____ Meloxicam 7.5 15 mg 1 qd bid # ____ Oxycontin 10 15 20 30 40 60 mg 1 q8 q12 hrs # ____ Opana ER 5 7.5 10 15 20 30 40 mg 1 q12 hrs # Exalgo 8 12 16 32 mg 1 ____ qd # ____ Morphine ER 15 30 60 mg 1 q8 q12hrs # ____ Nucynta ER 100 150 200 250 mg 1 q12 hrs # ____ Zohydro 10 15 20 30 40 50 mg 1 q12 hrs # ____ Methadone 5 10 mg 1 q12 q8 q6 hrs # ____ Fentanyl 12 25 50 75 100 mcg/hr 1 q72 q48 hrs # ____ Kadian 20 30 50 60 80 100 200 mg 1 q12 hrs # ____ Avinza 30 45 60 75 90 120 mg 1 qd # ____ ANTI-CONVULSANTS Refills ____ Lyrica 25 50 75 100 mg 1 qHS bid tid # ____ Neurontin 100 300 400 600 800 mg 1 qHS bid tid qid # ___ ANTI-DEPRESSANTS Refills ____ Cymbalta 20 30 60 mg 1 qd bid # ____ Refills ____ _________________ mg 1 qd bid # ____ Refills ____ ANXIOLYTICS PRN ANXIETY Refills ____ Alprazolam 0.25 0.5 1 2 mg 1 qd bid tid # ____ Clonazepam 0.5 1 2 mg ½ 1 bid # ____ TOPICAL Compound Cream Anti-inflammatory Neuropathic Combination apply 1-2 gms to affected areas 120 240 gm 5 refills Lidodem 5 % Patches apply 1 2 to affected areas q12 hrs on/12 hrs off # ____ 2. ___ Interventional pain procedures: 1) _____________________________________ 2) _____________________________________ 3) _____________________________________ 4) ______________________________________ 7. ___ Psychological testing SOAAP-R PMQ-R 3. ___ Physical therapy: ___ Land ___ Aquatic ___ Home Health ___ times per week for ___ weeks 9. ___ Psychological Evaluation: ___ Spinal cord stimulator trial ___ Suitability for chronic opioid use ___ Counseling ___ Biofeedback 4. ___ Imaging: ___ MRI ___ XRAY ___ CT SCAN ___ Myelogram ___ Bone scan ___ Lumbar ___ Cervical ___ Thoracic ___ Hip ___ Pelvis ___ Knee ___ Shoulder 6. ___ Urine drug testing: ___Today ___Next visit ___ As per PMQ protocol ___ Every visit 3 BBHI2 8. ___ Inclinometry and Muscle Strength Testing ___ Today every ___ months 10.___ Referral for consultation Dr. _________________________________ Reason ______________________________ 11. ___ Sleep Study. Diagnosis: OSA 5. ___ EMG/NCS: Dr. Al Baeer Dr. Nammour Dr. Yasser ___ Upper ___ Lower extremities Level of service FOLLOW UP VISIT Depression 4 5 12. ___ Run DPS report 13. ___ Follow up ___ month(s) ___ week(s) ___ Review UDT ___ Med refill ___ Review imaging ___ Post procedure(s) ___ Obtain patient’s medical records _____________________________ Jaime Robledo, M.D. 5