Hand and Tongue Physical Exam Powerpoint
advertisement

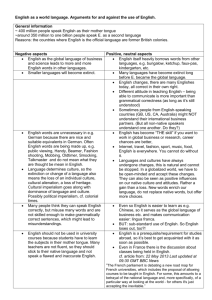
The Hands and the Tongue Lets look at the patient, not just the Labs, images, EKGs, i.e. Expanding our physical exam skills and findings: The Hands: Examination of the hand can reveal several physical findings helpful for diagnosis Start the exam with the Handshake: Moist and warm hands think…. nervousness, thyrotoxicosis look for tremor, eye signs Inability to let go your hand think…. Myotonia Look for other signs of myotonic dystrophy: hatchet face, cataracts, baldness, myopathic facies Physical Examination: Inspection Palpation Range of motion Stability Muscle and Tendon Function Nerve Assessment Vascular Assessment Integument Assessment Inspection: Look For…. Discoloration Deformity Muscular atrophy Trophic changes (sweat pattern, hair growth) Swelling Wounds or scars Also: compare to normal hand Discoloration: Redness: cellulitis White: arterial blockage Blue/purple: venous congestion Patches of blue/purple: trauma Black spots/lines: rule out melanoma Other color producing processes: fungi, viruses, psoriasis Osteoarthritis: Heberden’s nodes: DIP Bouchard’s nodes: PIP Rheumatoid Arthritis Boutonniere deformity: flexion of PIP and extension of DIP Swan neck deformity: extension of the PIP, flexion of DIP Dupuytren’s Contractures: Palmar or digital fibromatosis Flexion contracture Painless nodules near palmar crease Male> Female Epilepsy, diabetes, pulmonary dz, alcoholism Mallet Finger Hyperflexion injury Ruptured terminal extensor mechanism at DIP Incomplete extension of DIP joint or extensor lag Treatment: stack splint Muscle Atrophy: Generalized: may indicate disuse Specific muscle groups: suggest nerve pathology Thenar atrophy: carpal tunnel syndrome Interossei atrophy: cubital tunnel or cervical spine problem Subcutaneous atrophy: often after local steroid injection Range of Motion Assessment Nerve Assessment Radial: test dorsal thumb-index web space Median: test palmar surface of index or thumb Ulnar: test palmar aspect of little finger Digital nerves: test each the radial and ulnar side of each fingertip on the palmar aspect Proximal median nerve dysfunction Thenar atrophy, inability to flex 1st & 2nd fingers at PIP aka Pope’s Hand or Hand of Benediction Ask patient to use both hands to make and “Okay” sign by forming a circle with thumb and index finger Median nerve palsy may make one hand produce a pinched circle Ulnar nerve damage hypothenar atrophy and inability to flex 4th & 5th digits at the PIP aka Claw Hand Froment’s Sign: Ask patient to hold a piece of paper between thumb and index finger If you can pull paper away (a positive Froment’s sign), it suggests that an ulnar palsy has weakened the thumbs strength of opposition Special Tests: Finkelstein’s Used to test for deQuervain’s tendonitis inflammation of the EPB and APL tendons in the 1st extensor compartment Patient is asked to make a fist with the fingers overlying the thumb Examiner then ulnarly deviates the wrist (gently) Positive findings: pain along the 1st compartment Special Tests: Tinel’s A provocative test for carpal tunnel syndrome The examiner percusses with two fingers directly over the distal palmar crease in the midline Positive test: patient reports paresthesias in the median distribution when the nerve is percussed Special Tests: Phalen’s A provocative test for carpal tunnel syndrome The patient’s wrist is held in maximum flexion for two minutes Positive test: patient reports paresthesias in the median distribution Special Tests: Allen’s Tests ulnar and radial artery blood flow Patient makes a tight fist and examiner manually occludes both radial and ulnar artery Examiner releases one of the vessels and examines for reperfusion in the long finger Abnormal test: hand reperfusion > 5 seconds Test is repeated for the other artery Nail Abnormalities: Clues to Systemic Disease Clubbing: First described by Hippocrates in 5th century B.C thickening of the soft tissue beneath the proximal nail plate that results in sponginess of the proximal plate and thickening in that area of the digit Important causes of clubbing Lungs: LUNG CANCER clubbing is in general an ominous sign for this “beware of the yellow clubbed digit” Yellow from nicotine, and clubbed from cancer PUS in the lung bronchiectasis as in CF Lung abscess and empyema FIBROSIS but has to be considerable fibrosis to do this COPD IS NOT A CAUSE OF CLUBBING even though some textbooks say so–if it were clubbing would be a pretty useless sign, and many VA patients would have clubbing, but they don’t Important causes of clubbing Heart Causes: R to L shunts, Endocarditis, Pericarditis, atrioventricular malformations There are other causes of clubbing, outside the heart and lungs Inflammatory bowel disease, cirrhosis, congenital heart disease, fistulas Pseudoclubbing: distinguished from clubbing by the preservation of the nail-fold angle and bony erosion of the terminal phalanges on radiography changes in fingers are the result of soft-tissue collapse owing to severe bone erosions of the terminal phalanges Pitting: caused by defective layering of the superficial nail plate by the proximal nail matrix any localized dermatitis (e.g., atopic or chemical dermatitis) that disrupts orderly growth in that area also can cause pitting Psoriasis, Reiter’s syndrome, incontinentia pigmenti, alopecia areata usually is associated with psoriasis affecting 10 to 50 percent of patients with that disorder Paronychia: Inflammation of the nail folds–red, swollen, often tender Frequent immersion in water a risk factor for chronic paronychia If an abscess has formed, the recommended treatment is to drain the abscess by doing an I&D Herpetic Whitlow: Occupational hazard for respiratory therapists and housestaff who work around oral secretions HSV-1 is the cause in ~ 60% of cases HSV-2 cause in the remaining 40% Diagnosis usually is clinical Definitive diagnostic testing includes: Tzanck test, viral cultures, serum antibody titers, fluorescent antibody testing, or DNA hybridization Self-limited disease Treatment often is directed toward symptomatic relief Use antibiotic treatment only in cases complicated by bacterial superinfection Acral lentiginous melanoma Accounts for about 2-3% of all melanomas most common type of malignant melanoma among Asians and dark-skinned individuals, with a particular predilection for the soles of the feet The involvement of the proximal nail fold (Hutchinson’s sign) is considered a clue to the diagnosis Koilonychia: represented by transverse and longitudinal concavity of the nail -resulting in a “spoon-shaped” nail Iron deficiency anemia, hemochromatosis, Raynaud’s disease, SLE, trauma, nail-patella syndrome Yellow nail: Associated with: Lymphedema, pleural effusion, immunodeficiency, bronchiectasis, sinusitis, rheumatoid arthritis, nephrotic syndrome, thyroiditis, tuberculosis, Raynaud’s disease yellow nail syndrome: Triad of yellow slow-growing nails, lymphedema, and pleural effusions Splinter hemorrhage longitudinal thin lines, red or brown in color, that occur beneath the nail plate Subacute bacterial endocarditis, SLE, rheumatoid arthritis, antiphospholipid syndrome, peptic ulcer disease, malignancies, oral contraceptive use, pregnancy, psoriasis, trauma Tongue The tongue manifests the features of many systemic illnesses and is a natural site for oral pathology On physical examination, there are several characteristics that should be noted Color Texture Size Physical Examination: Normal tongue Dorsal surface Pinkish-red color Rough-appearing texture on the dorsal surface due to the presence of papillae three varieties with different sizes Ventral Surface similarly be pinkish-red some vasculature may be visible Tongue should fit comfortably in the mouth with the tip against the lower incisors Physical Examination: Normal tongue Examination of the tongue should occur in the following steps: Have the pt touch the tip of the tongue to the roof of their mouth and inspect the ventral surface Have the pt protrude the tongue straight out and inspect for deviation, color, texture, and masses With gloved hands, hold the tongue with gauze in one hand while palpating the tongue between the thumb and index finger of the other, noting masses and areas of tenderness Physical Examination: Normal tongue Abnormal Tongue Findings: Smooth Tongue: Most common cause is the use of dentures Can also be a late sign of iron, folate, Vit B12 deficiency Glossitis may also cause the tongue to appear smooth Among women, low-estrogen states may cause a “menopausal glossitis” Discolored Tongue: Due to a variety of conditions Micronutrient deficiencies is perhaps the bestknown of these B12 deficiency-> causing a sore, beefy-red tongue Pellagra-> causing a black tongue Geographic tongue: Benign condition in which discolored, painless patches of the tongue appear and then reappear, often in a different distribution Hairy Tongue: Best-known condition causing the tongue to appear hairy is Oral Hairy Leukoplakia A black, hairy tongue consistent with aspergillus overgrowth Ulcers: Many different causes Inspecting ulcers, it is important to note: size, number, color, distribution, and whether or not they cause the patient any discomfort Of particular concern is a single erythematous, often painful ulcer that does not heal May indicate that the patient has lingual or oral cancer particularly if the patient uses tobacco and/or alcohol Patient history and risk factors are important to note in these cases Aphthous ulcers: Painful form of ulcer that is most frequently encountered Minor aphthous ulcers: usually 2-8mm in size, spontaneously heal w/in 14 days Major aphthous ulcers: >1cm in size and may scar when they heal Herpetiform ulcers: pin-point size, often multiple, and may coalesce to form a larger ulcer These ulcers may result in odynophagia when they occur toward the posterior surface of the oropharynx Microglossia: May result from pseudobulbar palsy, the result of damage to the upper motor neurons of the corticobulbar tracts that innervate the tongue This results in a small, stiff tongue There may be an apparent microglossia resulting from ankyloglossia, a congenitally short lingual frenulum commonly called a “tongue tie” Macroglossia: Exam should include palpation of the sublingual glands, will be displaced in true macroglossia Macroglossia maybe congenitally present in acromegaly New-onset macroglossia in an adult is essentially pathognomonic for amyloidosis and should be treated as such until proven otherwise Fasciculation: Indicative of lower motor neuron injury May present with dysarthria or dysphagia Amyotrophic lateral sclerosis is of particular concern with new-onset of these Can cause atrophy of tongue