Nursing proc
advertisement

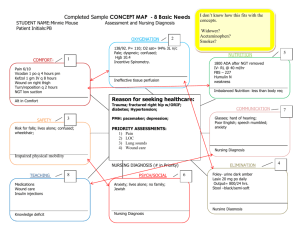
Nursing process and nursing diagnosis Nursing process An organizing framework for professional nursing practice Step I – nursing assessment Step II – making nursing diagnosis Step III – planning Step IV – implementation care Step V – evaluation the nursing care has been given Step I: Assessment Perfoming a thorough holistic nursing assessment of client Taking a medical history Perfoming a physical assessment Noting diagnostic test results Step I: Assessment To elicit as many symptoms as possible, the nurse should use open-ended rather than yes/no questions. Examples: “Describe what you are feeling” “How long have you been feeling this way?” “When did the symptoms start?” “Describe the symptoms” This type of questions will encourage the client to give more information about his or her situation. Listen carefully for cues and record relevant information. Step II: Nursing Diagnosis A nursing diagnosis is a clinical judgment about individual, family, or community responses to actual or potential health problems or life processes. Nursing diagnosis provide the basis for selection of nursing intervention to achieve outcomes for which the nurse is accountable (NANDA, 2003) Step II: Nursing Diagnosis A working of nursing diagnosis may have two or three parts. The three-part system consists of the nursing diagnosis, the “related to” statement, and the defining characteristics. PES system: P (problem) - The nursing diagnosis, the label; a concise term or phrase that represent a pattern of related cues E (etiology) – “Related to” phrase or etiology; related cause or contributor to the problem S (symptoms) –Defining characteristics phrase; symptoms that the nurse identifted in the assessment Step II: Nursing Diagnosis Case study: A 73-year-old man has been admitted to the unit with a diagnosis of chronic obstructive pulmonary disease (COPD). He states that he has “difficulty breathing when walking short distances”. He also states that his “heart feels like it is racing” at the same time. He states that he is “tired all the time”, and while talking to you he is comtinually wringing his hands and looking out the window. Step II: Nursing Diagnosis Part 1 (Problem) Interpretation of information: “difficulty breathing when walking short distances”= dyspnea “heart feels like it is racing”= dysrythmia “tired all the time”= fatigue In Section II we can find the nursing diagnosis Activity intolerance listed with these symptoms. Step II: Nursing Diagnosis To validate that the diagnosis Activity intolerance is appropriate for the client, we have to read NANDA definition of the nursing diagnosis. When reading, ask Does this definition describe the symptoms demonstrated by the client? If the appropriate nursing diagnosis has been selected, the definition should describe the condition that has been observed. Activity intolerance NANDA Definition Insufficient physiological or psychological energy to endure or complete required or desired daily activities. Defining Characteristics Verbal report of fatique or weakness; abnormal heart rate or blood pressure response to activity; exertional discomfort or dyspnea; electrocardiografic changes reflecting dysrhytmias or ischemia Related factors (r/t) Bed rest or immobility; generalized weakness,; sedentary lifestyle; imbalance between oxygen supply and demand Part 2 (Etiology) “Reated to” Phrase This phrase states what may be causing or contributing to the nursing diagnosis, commonly referred to as the etiology. Ideally the etiologe, or cause, of the nursing diagnosis is something that can be treated by a nurse. When this is the case, the diagnosis is identified as an independent nursing diagnosis. If medical Intervention is also necessary, it might be identified as a collabarative diagnosis. For each suggested nursing diagnosis, the nurse should refer to the statements listed under the heading “Related Factors” Part 3 (Symptoms) Defining Characteristic phrase It consist of the signs and symptoms that have been gathered during the assessment phase. Signs and symptoms are labeled as defining characteristics in Section III. The use of identifying defining characteristics is similar to the process the physician uses when making a medical diagnosis. Writing a Nursing Diagnosis Statement P - Activity intolerance E – “Related to” imbalance between oxygen supply and demand S – Verbal reports of fatique, exertional dyspnea (“difficulty breathing when walking”), and dysrythmia (“racing heart ”) Step III: Planning (outcomes and interventions) Consists of writing measurable client outcomes and nursing intervention to accomplish the outcomes. Before this can be done, if the client has more than one diagnosis, the priority of the nursing diagnoses must be determined. Step III: Planning (outcomes and interventions) Outcomes are conceptualized as variable client states influenced by nursing intervention. Thus client outcomes represent patient states that vary and can be measured and compared with a baseline over time. Development of appropriate oucomes can de done one or two ways: using Nursing Outcomes Classification (NOC) or writing an outcomes statement. Step III: Planning (outcomes and interventions) NOC outcome is defined as follows: An individual, family, or community state; behavior; or perception that is measured along a continium in response to one or more nursing interventions. Each outcome has a group of indicators that are used to determine patient status in relation to outcome (Moorhed, 2003) Because the NOC outcomes are very specific, they enhance the nursing process by helping to nurse to record changes after interventions have been perfomed. Step III: Planning (outcomes and interventions) Activity intolerance NOC outcomes Activity Tolerance Endurance Energy Conservation Self-Care: Instrumental Activities of Daily Living Step III: Planning (outcomes and interventions) Endurance as evidenced by the following indicators: Perfomance of usual routine /Activity /Rested appearence/Blood oxygen level within normal limits /Expresses feelings about loss /Verbalizes acceptance of loss /Describes meaning of the loss or death/Report decreased preoccupation with loss/Express positive expectations about the future (Rate each indicator of Endurance: 1=extremely compromised, 2=substantially compromised, 3=moderately compromised, 4=mildly compromised, 5=not compromised) Step III: Planning (outcomes and interventions) Interventions are like road maps directing the best ways to provide nursing care. The National Guidelines Clearinghouse (NGC) is a comprehensive database of evidence-based clinical practice guidelines and related documents www.guideline.gov Evidance-Based Nursing www.evidancebasednursing.com www.globalevidence.com Step III: Planning (outcomes and interventions) Section III suplies choices of interventions for each nursing diagnosis. The interventions are identified as independent ( autonomous actions that are initiated by the nurse in response to a nursing diagnosis) or collaborative (actions that the nurse perfoms in collaborations with other health care professionals and that may require a physician’s order and may be in response to both nursing snd medical diagnosis). Step IV: Implementation It is actual initiation of the nursing care plan. During this phase the client is assessed to determine whether the interventions are effecive. An important part of this phase is documentation. Documentation is also necessary for legal reasons because in a legal dispute anything that has not been charted is considered not to have been done. Step V: Evaluation It is actually an integrl part of each phase and something that is done continually. At the last phase the clients’ outcomes are evaluated to determine whether they were met.