Chapter 18 - WordPress.com
advertisement

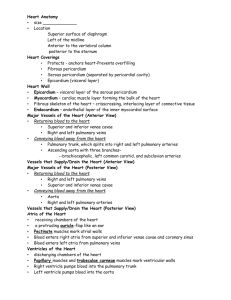
Lecture – 6 (18) Sept. 12, 2011 ** Utilize Interactive Physiology on My A&P [0:00[ pg 661 Vessels determine blood pressure due to smooth muscle lining the vessels Cardiac Output (CO) is the volume pumped per minute Volume (ml)/min Contractibility strength of contraction ↑CO Cardiac Conductive System = muscle contraction or muscle excitation [8:00] Thoracic Cavities includes: Pleural Cavity & Mediastinal Cavity [Superior Mediastinal & Inferior Mediastinal (Pericardial Cavity)] The heart contains a fibrous skeletal network of collagen/elastic fibers Coverings of the Heart Pericardium = a double-walled sac Fibrous Pericardium = loosely fitting superficial part of this sac containing a tough, dense connective tissue layer which 1) protects the heart, 2) anchors it to surrounding structures, and 3) prevents overfilling of the heart with blood. Serous Pericardium = a thin, slippery, two-layer serous membrane Parietal layer = lines the internal surface of the fibrous pericardium Visceral layer (aka: epicardium) = lays on the surface area of the heart Pericardial Cavity = is a slit-like layer between the parietal/visceral layers contains a film of serous fluid Pericarditis = inflammation of the pericardium, roughens the serous membrane surfaces. Cardiac Tamponade = heart compression due to a large amount of fluid seeping into pericardial cavity. Layers of the Heart Wall Epicardium = outer covering of the heart (aka: visceral pericardium) Myocardium = composed of cardiac muscle & the crisscross connective tissue fibers making up the fibrous skeleton of the heart. 1 Endocardium = a glistening white sheet of endothelium resting on a thin layer of connective tissue; it lines the heart chambers, covers the valves fibrous skeleton and is continuous with the endothelial linings of the blood vessels leaving and entering the heart. Two Atria separated by the interatrial septum Two Ventricles separated by the interventricular septum [20:00] pg 668 Pulmonary Circuit + 682 Cardiac Cycle Pressure and Volume related inversely Volume drives Pressure [note: blood is actually sucked into the right ventricle] BLOOD FLOW Inferior/Superior Vena Cava + coronary sinus right atrium tricuspid valve (AV valve) right ventricle pulmonary semilunar valve pulmonary trunk L/R pulmonary artery LUNGS L/R pulmonary veins left atrium mitral (bicuspid) valve (AV valve) left ventricle aortic semilunar valve aorta R/L coronary arteries (LCA -> left anterior interventricular artery -> circumflex artery; RCA -> right marginal artery -> posterior interventricular artery) brachiocephalic trunk (right carotid and right subclavian arteries) left common carotid artery left subclavian artery Anastomoses=specialized branching of coronary arteries allowing them to run collaterally(side-by-side) 2 Chordae Tendineae – prevents AV valves from hyper-extension into the atrial chambers The Aortic and Pulmonary (SL) valves guard the bases of the large arteries issuing from the ventricles (aorta and pulmonary trunk, respectively) and prevent backflow into the associated ventricles. There are NO VALVES guarding the entrances of the venae cavae and pulmonary veins into the right and left atria, respectively. Small amounts of blood do spurt back into these vessels during atrial contraction, the backflow is minimal because of the inertia of the blood and because as it contracts, the atrial myocardium compresses these venous entry points. [40:00] pg 682 Pressure drives blood through the heart Flow from high pressure to low pressure Pg 705 – Graph [x-axis = distance traveled] Systole = Contraction Diastole = relaxation Asystole = without heat beat Cardiac Cycle = includes all events associated with the blood flow through the heart during one complete heartbeat. [46:15] pg682 Ventricular filling: mid-to-late diastole pressure in the heart is low, blood returning from the circulation is flowing passively through the atria and the open AV valves into the ventricles (aortic and pulmonary valves are closed) Approximately 70-80% of ventricular filling occurs during this period, and the AV valve flaps begin to drift toward the closed position. (The remaining 20-30% is delivered to the ventricles when the atria contract towards the end of this phase) Then the atria relax and the ventricles depolarize (QRS complex). Atrial diastole persists through the rest of the cycle. Ventricular systole: As the atria relax, the ventricles begin contracting. Ventricular pressure rises rapidly and sharply, closing the AV valves. During this ventricular ejection phase, the pressure in the aorta normally reaches about 120 mm Hg. During diastolic period of relaxation the pressure in the aorta is normally about 80 mm Hg. 3 [56:00] pg 669 Anastomoses=specialized branching of coronary arteries allowing them to run collaterally(side-by-side) Coronary Circulation = heart is the first to receive oxygenated blood [1:01:30] pg 672 Laminar Flow = flows in layers / smoothly Turbulent Flow = gushing noisily Murmur = noise as with leaky valves Incompetent valve – forces the heart to re-pump the same blood over and over because the valve does not close properly and blood backflows. Valvular Stenosis (narrowing) – the flaps become stiff (typically scar tissue from endocarditis or calcium salt deposits) and constrict the opening. This stiffening compels the heart to contract more forcibly than normal. Lecture – 7 (18) Sept. 14, 2011 Pg 672 Cardiac Muscle Fibers Intercalated discs contain anchoring desmosomes and gap junctions. Desmosomes prevent adjacent cells from separating during contraction. Gap Junctions allow ions to pass from cell to cell, transmitting current across the entire heart. Because cardiac cells are electrically coupled by the gap junctions, the myocardium behaves as a single coordinated unit, or functional syncytium – allowing the heart cells to beat as ‘ONE’. Large mitochondria account for 25-35% of the volume of cardiac cells and give the cardiac cells a high resistance to fatigue. Mechanism and Events of Contraction Although heart muscle and skeletal muscle are contractile tissues, they have some fundamental differences: Skeletal and Cardiac Muscle Differences: 4 1. Means of Stimulation – Each skeletal muscle fiber must be stimulated to contract by a nerve ending, but some cardiac muscle cells are self-excitable. These cells can initiate not only their own depolarization, but that of the rest of the heart as well, in a spontaneous and rhythmic way – this property is called automaticity, or autorhythmicity . 2. Organ versus motor unit contraction – In skeletal muscle, all cells of a giv3en motor unit (but not necessarily all motor units of the muscle) are stimulated and contract at the same time. Impulses do not spread from cell to cell. In cardiac muscle, the heart either contracts as a unit or doesn’t contract at all. This coordinated actions occurs because gap[ junctions electrically tie all cardiac muscle cells together into a single contractile unit. Consequently, the depolarization wave travels across the heart from cell to cell via ion passage through the gap junctions. 3. Length of absolute refractory period – In cardiac muscle cells, the absolute refractory period (the unexcitable period when Na+ channels are still open or inactivated) lasts approximately 250 ms, nearly as long as the contraction. Contrast this to the short refractory periods of 1-2 ms in the skeletal muscle fibers, in which contraction last 15-100 ms. The long cardiac refractory period normally prevents tetanic contractions, which would stop the heart’s pumping action (it prevents tetany of the cardiac muscle). Skeletal and Cardiac Muscle Similarities: As with skeletal muscle, cardiac muscle contraction is trigger by action potentials that sweep across the cell membrane. About 1% of cardiac fibers are autorhythmic (self-rhythm), having the special ability to depolarize spontaneously and thus pace the heart (these cells make up the SA node, AV node, AV bundle, Bundle Branches, and the purkinje fibers). Pg. 674 The bulk of heart muscle, however, is composed of contractile muscle fibers responsible for the heart’s pumping activity. In these cells, the sequence of events leading to contraction is similar to that in skeletal muscle fibers. Depolarization opens a few voltage-gated fast Na+ channels in the sarcolemma, allowing extracellular Na+ to enter. The period of Na+ influx is very brief, because the sodium channels quickly inactivate and the Na+ influx stops. Transmission of the depolarization wave down the T tubules (ultimately) causes the sarcoplasmic reticulum (SR) to release Ca++ into the sarcoplasm. Excitation-contractrion coupling occurs as Ca++ provides the signal (via troponin binding) for cross bridge activation and couples the depolarization wave to the sliding of the myofilaments. These three steps are common to both skeletal and cardiac muscle cells. These two muscle types differ in how the SR is stimulated to release Ca++. 5 Some 10-20% of the Ca++ needed for the calcium pulse that triggers contraction enters the cardiac cells from the extracellular space. Once inside, it stimulates the SR to release the other 80% of the Ca++ needed. Ca++ is barred from entering non-stimulated cardiac fibers, but when Na+ dependent membrane depolarization occurs, the voltage change also opens channel that allow Ca++ entry from the extracellular space. These channels are called slow Ca++ channels because their opening is delayed a bit. Action Potential of Contractile Cardiac Muscle Cells 1. Depolarization is due to Na+ influx through fast voltage-gated Na+ channels. A positive feedback cycle rapidly opens many Na+ channels, reversing the membrane potential. Channel inactivation ends this phase. 2. Plateau phase is due to Ca++ influx through slow Ca++ channels. This keeps the cell depolarized because few K+ channels are open. 3. Repolarization is due to Ca++ channels inactivating and K+ channels opening. This allows K+ efflux (to leave), which brings the membrane potential back to its resting voltage. Voltage-gated – remains open for short period of time only. Energy Requirements Cardiac muscle has more mitochondria than skeletal muscle does, reflecting its greater dependence on oxygen for its energy metabolism. Unlike skeletal muscle, which can contract for prolonged periods, even during oxygen deficits, by carrying out anaerobic respiration, the heart relies almost exclusively on aerobic respiration. As a result, cardiac muscle cannot incur much of an oxygen deficit and still operate effectively. Both types of muscle tissue use multiple fuel molecules, including glucose and fatty acids. But cardiac muscle is much more adaptable and readily switches metabolic pathways to use whatever nutrient supply is available, including lactic acid generated by skeletal muscle activity. Consequently, the real danger of and inadequate blood supply to the myocardium is lack of oxygen, not of nutrient fuels. 6 When a region of heart muscle is deprived of blood (is ischemic). The oxygen-starved cells begin to metabolize anaerobically, producing lactic acid. The rising H+ level that results hinders the cardiac cells’ ability to produce the ATP they need to pump Ca++ into the extracellular fluid. This ↓ pH causing ACIDOSIS. If the ischemic area is large, the pumping activity of the heart as a whole may be severely impaired, leading to a heart attack. Pacemaker and action potentials of Autorhythmic cells of the heart 1. Pacemaker potential – this slow depolarization is due to both opening of Na+ channels and closing of K+ channels. Notice that the membrane potential is never a flat line. 2. Depolarization – The action potential begins when the p[acemaker potential reaches threshold. Depolarization is due to Ca++ influx through Ca++ channels. [FAST Ca++ channels] 3. Repolarization – is due to Ca++ channels inactivating and K+ channels opening. This allows K+ efflux (to flow out), which brings the membrane potential back to its most negative voltage. More Ca++ ↑ Excitation & Contractibility [forms more cross-bridges] Ca++ required for cross-bridges Electrical activity required before contraction is possible You can have electrical activity without contraction You cannot have contraction without electrical actitity Pg. 676 Setting the Basic Rhythm Action Potential Initiation by Autorhythmic Cells Autorhythmic cells do not have a stable resting membrane potential, theirs is an unstable resting membrane potential that continuously depolarizes, drifting slowly towards threshold. These spontaneously changing membrane potentials, called pacemaker potentials or prepotentials, initiate the action potentials that spread throughout the heart to trigger its rhythmic contractions. Sequence of Excitation Autorhythmic cardiac cells are found in the following areas: SA node, VA node, AV bundle, bundle branches and Purkinje fibers. Impulses pass across the heart in order from 1 to 5. 7 1. Sinoatrial node – A minute cell mass with a mammoth job, the SA node typically generates impulses about 75 times every minute. (It’s inherent rate in the absence of extrinsic neural; and hormonal factors is closer to 100 times per minute.) The SA node sets the pace for the heart as a whole because no other region of the conduction system or the myocardium has a faster depolarization rate. For this reason, it is the heart’s pacemaker, and its characteristic rhythm, called sinus rhythm, determines the heart rate. 2. Atrioventricular node – From the SA node, the depolarization wave spreads via gap junctions throughout the atria and via the internodal pathway to the AV node. The AV node conducts impulses more slowly than other parts of the system due to the smaller diameter of the fibers and the fact that they have fewer gap junctions. 3. Atrioventricular Bundle – aka Bundle of HIS 4. Right/Left Bundle Branches – splits from AV bundle into two branches 5. Purkinje Fibers – Essentially long strands of barrel shaped cells. What is responsible for the pacemaker potential (Autorhythmic)? = LEAKY Na+ / unstable membrane SA node (fibers) are the most excitable part of the heart SA node has a lower threshold – than other Autorhythmic cells. Pg. 678 Ventricular contraction almost immediately follows the ventricular depolarization wave. The wring motion of contraction begins at the heart apex and moves toward the atria, following the direction of the excitation wave through the ventricle walls. The SA node normally drives the heart at a rate of 75 b.p.m. Without SA node input, the AV node would depolarize only about 50 times per minute. ALikewise, the AV bundle and the Purkinje fibers would depolarize only about 30 times per minute without input from the AV node. The cardiac conduction system coordinates and synchronized heart activity. Arrhythmias – (without rhythm) uncoordinated atrial and ventricular contractions, and even fibrillation, a condition of rapid and irregular or out-of-phase contractions in which the SA node has lost control of pace-making. Defibrillation is accomplished by electrically shocking the heart, which interrupts its chaotic twitching by depolarizing the entire myocardium, wiping the slate clean. An ectopic focus, which is an abnormal pacemaker, may appear and take over the pacing of heart rate, or the AV node may become the pacemaker. 8 Any damage to the AV node interferes with the ability of the ventricles to receive pacing impulses, this is referred to as a heart block. Modifying the Basic Rhythm: Extrinsic innervation of the heart Basic heart rate is set by the intrinsic conduction system, however, fibers of the autonomic nervous system modify the march-like beat and introduce a subtle variability from one beat to the next. The sympathetic nervous system (the accelerator) incrase both the rate and the force of heartbeat, and the parasympathetic activation (the brakes) slows the heart. Cardiac Centers in Medulla Oblongata – The cardioacceleratory center projects to sympathetic neurons in the T1-T3 levels of the spinal cord. The Cardioinhibitory center sends impulses to the parasympathetic dorsal vagus nucleus in the medulla, which in turn sends inhibitory impulses to th3e heart via branches of the vegus nerves. Electrocardiography Electrocardiograph – Equipment used to measure electrical currents generated by the heart Electrocardiogram (EKG/ECG) – A graphic record of the hearts electrical activity. Lecture – 8 (18) Sept. 19, 2011 Pg.680-681 P Wave = Atrial depolarization, initiated by the SA node, causes the P wave QRS Complex = Ventricular depolarization occurs at apex (R); Atrial repolarization T Wave = Ventricular repolarization begins at apex, causing the T wave Normal Sinus Rhythm = Normal Heart Conductivity – aka Sinus Rhythm Junctional Rhythm = SA node is non-functioning, P waves are absent; AV sets a slower pace Second-Degree Heart Block = Some P waves are not conducted through to the AV node; hence more P waves are seen than QRS complexes, usually 2:1 Ventricular Fibrillation = Chaotic/Grossly irregular EKG deflections (quivering); non-functioning heart 9 [17:00] pg.689 Tetralogy of Fallot = Multiple defects (tetra = four) 1- pulmonary trunk too narrow and pulmonary valve stenosed, resulting in 2- hypertrophied right ventricle; 3- ventricular septal defect; 4- aorta opens from both ventricles. Occurs in 1:2000 births, somewhat common. Foramen Ovale – Interatrial septum of the fetal heart is incomplete; connecting the two atria. Ductus Arteriosus – another lung bypass exists between the pulmonary trunk and aorta (fetal). Pg. 681 Heart Sounds = the lub-dub associated with closing of the heart valves Because the mitral valve closes slightly before the tricuspid valve does, and the aortic SL valve generally snaps shut just before the pulmonary valve, it is possible to distinguish the individual valve sounds by auscultating four specific regions of the thorax. Heart Murmurs = Abnormal heart sounds. Murmurs usually indicate valve problems/Foramen Ovale most common heart murmur (more women than men). If a valve fails to close completely, a swishing sound is heard as the blood backflows or regurgitates through the partially open valve after the valve has supposedly closed. Such valves are termed insufficient or incompetent and create turbulent flow. If a valve fails to open completely, its narrow opening restricts blood flow through the valve. Such valves are termed stenotic. Systole & Diastole refer respectively to ventricular contraction and relaxation periods. The cardiac cycle is marked by a succession of pressure and blood volume changes in the heart. Volume Drives Pressure Volume Effects Pressure ↑ Volume – ↓ Pressure Negative Pressure = (means) Less Than Ventricular filling: mid-to-late diastole – Pressure in the heart is low, blood returning from the circulation is flowing passively through the atria and the open AV valves into the ventricles, and the aortic and pulmonary valves are closed. Approximately 80 % of ventricular filling occurs during this period, and the AV valve flaps begin to drift toward the closed position. The remaining 20% is delivered to the ventricles when the atria contract toward the end of this phase. Isovolumetric Contraction Phase = The split-second period when the ventricles are completely closed chambers and the blood volume in the chambers remains constant as the ventricles contract. Isovolumetric Relaxation Phase (early diastole) = Brief phase following the T wave, the ventricles relax. Because the blood remaining in their chambers, referred to as the end systolic volume (ESV), is no longer compressed, ventricular pressure drops rapidly and blood in the aorta and pulmonary trunk flows back toward the heart, closing the SL valves. 10 The pulmonary circulation is a low-pressure circulation as evidenced by the much thinner myocardium of its right ventricle. So, typical systolic and diastolic pressures for the pulmonary artery are 24/8 mm Hg as compared to systemic aortic pressures of 120/80 mm Hg, respectively. However, the two sides of the heart eject the same blood volume with each heartbeat. Pg.682 Cardiac Output Cardiac Output (CO) is the amount of blood pumped out by each ventricle in 1 minute. Cardiac Output (CO) = Product of the Heart Rate (HR) or pulse and Stroke Volume (SR) Stroke Volume (SV) = the volume of blood pumped out by one ventricle with each beat. In general, Stroke Volume is correlated with the force of ventricular contraction. Hormones, drugs and ions can change CO. CO = HR x SV SV = EDV – ESV Pg.684 Normal adult blood volume is about 5L (a little more than a gallon), The entire blood supply passes through each side of the heart once each minute. Cardiac output is highly variable and increases markedly in response to special demands, such a running to catch a bus. Cardiac Reserve = the difference between resting and maximal CO. In nonathletic people, cardiac reserve is typically 4-5 times resting CO (20-25 L/min.) CO in trained athletes during competition may reach 7 times resting (35 L/min.) Regulation of Stroke Volume SV represents the difference between end diastolic volume (EDV), the amount of blood that collects in a ventricle during diastole, and end systolic volume (ESV)m the volume of blood remaining in a ventricle after it has contracted. SV = EDV – ESV The ESV, determined by arterial blood pressure and the force of ventricular contraction, is approximately 50 ml. The higher the arterial blood pressure the higher the ESV. Three most important factors affecting SV are: preload, contractility, and afterload. 11 Preload – (degree of stretch of heart muscle) – the criticle factor controlling SV is the preload, which is the degree to which cardiac muscle cells are stretched just before the contract. Venous Return – most important factor stretching cardiac muslce is the amount of blood returning to the heart and distending its ventricles, called Venous Return. Anything that increases the volume or speed of venous return, such as a slow heart rate or exercise, increased EDV and, consequently, SV and contraction force. A slow heart rate allows more time for venous return/ventricle filling; exercise speeds venous return because both increased sympathetic nervous system activity and the squeezing action of the skeletal muscles compresses the veins. During vigorous exercise, SV may double as a result of increased venous return. EDV – is the major intrinsic factor influencing SV. EDV – is affected by preload (↑ preload - ↑ EDV - ↑ CO) (slow HR - ↑ preload - ↑EDV - ↑CO) (↑ venous return - ↑EDV - ↑CO) (Exercise - ↑ venous return - ↑EDV - ↑CO) Contractility – contractile strength achieved at a given muscle length – an extrinsic factor affecting SV. Increased sympathetic stimulation increases contractility of the heart. One effect of norepinephrine or epinephrine binding is to initiate a cyclic AMP second-messenger system that increases Ca++ entry, which in turn promotes more cross bridge binding and enhances ventricular contractility. Factors that increase contractility are called positive inotropic agents = A battery of other chemicals also influences contractility; For example, contractility is enhanced by the hormones glucagon, thyroxine, and epinephrine, by the drug digitalis, and by high levels of extracellular Ca++. Factors that impair or decrease contractility are called negative inotropic agents – includes acidosis ↓pH (excess H+ ions), rising extracellular K+ levels and drugs called calcium channel blockers. Contractility (a force) – Extrinsic affects ESV (↑ contractility - ↓ESV - ↑SV - ↑CO) Afterload – Back pressure exerted by Arterial Blood – The pressure that must be overcome for the ventricles to eject blood is called afterload. It is essentially the back pressure exerted on the aortic and pulmonary valves by arterial blood, about 80 mm Hg in the aorta and 8 mm Hg in pulmonary trunk. Afterload – affects ESV (↑ afterload - ↑ ESV - ↓ SV - ↓ CO) Volume Drives Pressure Volume effects Pressure Negative pressure means pressure less than the chamber next to it. 12 ↑ Volume - ↓ Pressure Lecture – 9 (18) Sept. 21, 2011 Pg. 685 Cardiac Output CO = HR x SV ↑HR = Exercise, Flight/fight, hormones, fever, pain, dehydration, drugs, anxiety, age/gender Regulation of Heat Rate Autonomic Nervous System Regulation Most important extrinsic controls affecting heart rate are exerted by the autonomic nervous system (↑Sympathetic activity) Norepinephrine binds to β₁-adrenergic receptors in the heart, causing threshold to be reached more quickly. As a result, the pacemaker fires more rapidly and the heart responds by beating faster. Sympathetic stimulation also enhances contractility and speeds relaxation. It does this by enhancing Ca++ movements in the contractile cells as we described above. ESV falls as a result of this increased contractility, so SV does not decline, as it would if only heart rate were increased. (Remember, when the heart beats faster, there is less time for ventricular filling and so a lower EDV.) 13 The parasympathetic division opposes sympathetic effects and effectively reduces heart rate when a stressful situation has passed. Parasympathetic-initiated cardiac responses are mediated by acetylcholine, which hyperpolarizes (further away from threshold/depolarization) the membranes of its effector cells by opening K+ channels. Under resting conditions, both autonomic divisions continuously send impulses to the SA node of the heart, but the dominant influence is inhibitory. For this reason, the heart is said to exhibit VAGAL TONE, and heart rate is generally slower than it would be if the vagal nerves were not innervationg it. Cutting the vagal nerves results in an almost immediate increase in heart rate of about 25 beats/min, reflecting the inherent rate (100 beats/min) of the SA node. Most such sensory input 9is generated by baroreceptors which respond to changes in systemic blood pressure. Another example, the atrial (Bainbridge) reflex, is a sympathetic reflex initiated by increased venous return and increased atrial filling. Stretching the atrial walls increases heart rate by stimulating both the SA node and the atrial stretch receptors, which trigger reflexive adjustments that result in increased sympathetic stimulation of the heart. ** Exercise initiates sympathetic response Chemical Regulation 1. Hormones a. Epinephrine – liberated by the adrenal medulla during sympathetic nervous system activation, produces the same cardiac effects as norepinephrine released by the sympathetic nerves. It enhances heart rate and contractility. b. Thyroxine – is a thyroid gland hormone that increases metabolic rate, body heat production, and heart rate. Thyroxine also enhances (synergistic effect) the effects of epinephrine and norepinephrine on the heart, so chronically hyperthyroid individuals may develop a weakened heart. 2. Ions – Physiological relationships between intercellular and extracellular ions must be maintained for normal heart function. Plasma electrolyte imbalances pose real dangers to the heart. [K+, Ca++, Na+] Reduced Ca++ blood levels (hypocalcemia) depress the heart. Conversely, above-normal levels (hypercalcemia) tightly couple the excitation-contraction mechanism and prolong the plateau phase of the action potential. High or low blood K+ levels are particularly dangerous and arise in a number of clinical conditions. Excessive K+ (hyperkalemia) interferes with depolarization by lowering the resting potential, and may lead to heart block and cardiac arrest. Hypokalemia is also life threatening, in that the heart beats feebly and arrhythmically. 14 Other Factors: Age, gender, exercise, and body temperature also influences HR, although they are less important than neural factors. Resting HR is fastest in the fetus (140-160 bpm) and gradually declines throughout life. Average HR is faster in females 972-80 bpm) than in males (64-72 bpm). Exercise raises HR by acting through the sympathetic nervous system (Bainbridge/atrial reflex). Exercise also increases systemic blood pressure and routes more blood to the working muscles. Heat increases HR by enhancing the metabolic rate of cardiac cells. This explains the rapid, pounding heartbeat you feel when you have a high fever and also accounts, in part, for the effect of exercise on HR (remember, working muscles generates heat). Cold directly decreases heart rate. Tachycardia = an abnormally fast heart rate (usually anything > 100 bpm) Bradycardia = an abnormally low heart rate (usually anything < 60 bpm) Note: Athlete bradycardia is the results of conditioning and training and is normal for them. Congestive Heart Failure (CHF) – A condition where the CO is inadequate to meet tissue needs. This progressively worsening condition reflects weakening of the myocardium by various conditions which damage it in different ways – Such As: 1. Coronary Atherosclerosis – essentially a clogging of the coronary vessels with fatty buildup, impairing blood and oxygen delivery to the cardiac cells. 2. Persistent High Blood Pressure – When aortic diastolic BP rise to 90 mm Hg or more, the myocardium must exert more force to open the aortic valve to pump out the blood. 3. Multiple Myocardial Infarcts – Dead heart cells are replaced by non-contractile fibrous scar tissue. 4. Dilated Cardiomyopathy (DCM) - A condition in which the ventricles stretch and become flabby and the myocardium deteriorates. Pulmonary Congestion – Caused by failure of the left side of the heart Peripheral Congestion – Caused by failure of the right side of the heart Congenital heart defects – Most common of all birth defects Note: Norepinephrine increases heart contractility via a cyclic AMP (cAMP) second-messenger system. Internet Source Material Google: Indiana Fetal Circulatory System & University of Minnesota Web Anatomy - Cardio 15 Related Clinical Terms: Asystole – heart fails to contract (without beat) Cardiac Catheterization – Diagnostic procedure involving passage of a fine catheter through a blood vessel into the heart. Commotio Cordis – (Concussion of the Heart) – A mild blow to the chest cause heart failure and sudden death occurs because it occurs during a vulnerable interval (2ms) when the heart is repolarizing. Cor Pulmonale – Pulmonary Hypertension caused by right-sided heart failure. Endocarditis – Inflammation of the endocardium, usually confined to the endocardium of the heart valves; often resulting from bacterial/fungal infection in the blood stream, or an autoimmune response. Heart Palpitation – A heartbeat that is unusually strong, fast, or irregular; a person may be aware of it. Hypertrophic Cardiomyopathy (HCM) – A condition, usually inherited, causes the cardiac muscle cells to enlarge, thickening the heart wall. The heart doesn’t relax well during diastole when the heart is filling. Mitral Valve Prolapse – Usually an abnormal chordae tendineae or a malfunction of the papillary muscles; causing the mitral valve to become incompetent allowing blood regurgitation. Myocarditis – Inflammation of the cardiac muscle layer of the heart; may follow an untreated streptococcal infection in children. Paroxysmal Atrial Tachycardia (PAT) – Bursts of atrial contractions with little pause between them. Ventricular Tachycardia (VT or V-tac) – Rapid ventricular contractions that are not coordinated with atrial activity. 16