BIOTERRORISM
advertisement

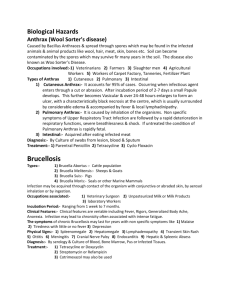
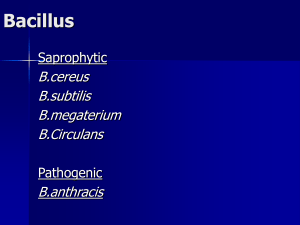
BIOTERRORISM HISTORY • Microbial pathogens were used as potential weapons of war or terrorism from ancient times: – the poisoning of water supplies in the sixth century B.C. with the fungus Calviceps purpurea (rye ergot) by the Assyrians – the hurling of the dead bodies of plague victims over the walls of the city of Kaffa by the Tartar army in 1346 – the spreading of smallpox via contaminated blankets by the British to the native American population loyal to the French in 1767. Key Features of Biologic Agents Used as Bioweapons • • • • • • • • • • High morbidity and mortality Potential for person-to-person spread Low infective dose and highly infectious by aerosol Lack of rapid diagnostic capability Lack of universally available effective vaccine Potential to cause anxiety Availability of pathogen and feasibility of production Environmental stability Database of prior research and development Potential to be “weaponized” CLASSIFICATION • Centers for Disease Control and Prevention (CDC) classifies potential biologic threats into three categories: A, B, and C • Category A agents are the highest-priority pathogens: – – – – – can be easily disseminated or transmitted from person to person result in high mortality rates have the potential for major public health impact might cause public panic and social disruption require special action for public health preparedness. • Category B agents include those that are moderately easy to disseminate, result in moderate morbidity rates and low mortality rates, and require specifically enhanced diagnostic capacity. • Category C agents include emerging pathogens – the general population lacks immunity – could be engineered for mass dissemination in the future because of availability, ease of production, ease of dissemination – The recent emergence of novel viruses leading to outbreaks of severe acute respiratory syndrome (SARS), Nipah, hantavirus are examples Category A agents • Anthrax (Bacillus anthracis) • Botulism (Clostridium botulinum toxin) • Plague (Yersinia pestis) • Smallpox (Variola major) • Tularemia (Francisella tularensis) Viral hemorrhagic fevers: • Arenaviruses: Lassa, New World (Machupo, Junin, Guanarito, and Sabia) • Bunyaviridae: Crimean Congo, Rift Valley • Filoviridae: Ebola, Marburg • Flaviviridae: Yellow fever; Omsk fever; Kyasanur Forest Category B agents • Brucellosis (Brucella spp.) • Epsilon toxin of Clostridium perfringens • Food safety threats: – Salmonella sp. – Escherichia coli 0157:H7 – Shigella sp. • Water safety threats – Vibrio cholerae – Cryptosporidium parvum) • • • • • • • • Glanders (Burkholderia mallei) Melioidosis (B. pseudomallei) Psittacosis (Chlamydia psittaci) Q fever (Coxiella burnetii) Ricin toxin from Ricinus communis (castor beans) Staphylococcal enterotoxin B Typhus fever (Rickettsia prowazekii) Viral encephalitis – alphaviruses (e.g., Venezuelan, eastern, and western equine encephalitis) Anthrax as a Bioweapon • Anthrax may be the prototypic disease of bioterrorism although rarely spread from person to person • U.S. and British government scientists studied anthrax as a biologic weapon beginning approximately at the time of World War II (WWII). • Soviet Union in the late 1980s stored hundreds of tons of anthrax spores for potential use as a bioweapon • At present there is suspicion that research on anthrax is ongoing by several nations and extremist groups • One example of this is the release of anthrax spores by the Aum Shrinrikyo cult in Tokyo in 1993. Fortunately, there were no casualties associated with this episode. Anthrax as a Bioweapon II • 1979: the accidental release of spores into the atmosphere from a Soviet Union bioweapons facility in Sverdlosk: – at least 77 cases of anthrax were diagnosed with certainty, of which 66 were fatal – victims have been exposed in an area within 4 km downwind of the facility – deaths due to anthrax were also noted in livestock up to 50 km away from the facility – interval between probable exposure and development of clinical illness ranged from 2 to 43 days (the majority of cases were within the first 2 weeks) – death typically occurred within 1 to 4 days following the onset of symptoms – the anthrax spores can lie dormant in the respiratory tract for at least 4 to 6 weeks • September 2001: anthrax spores delivered through the U.S. Postal System. – CDC identified 22 confirmed or suspected cases of anthrax (11 patients with inhalational anthrax, of whom 5 died, and 11 patients with cutaneous anthrax - 7 confirmed - all of whom survived) – cases occurred in individuals who opened contaminated letters as well as in postal workers involved in the processing of mail – one letter contained 2 g of material, equivalent to 100 billion to 1 trillion spores (inoculum with a theoretical potential of infecting up to 50 million individuals) – The strain used in this attack was the Ames strain - was susceptible to all antibiotics Bacillus anthracis • Aerobic, sporing Gram-positive rod: infection usually transmitted by spores • Generally more sensitive to antibiotics than other Bacillus species, but multi drug resistant strains have been found in nature • BUT not sensitive to 3rd generation cephalosporins • Easily dismissed as a contaminant when identified in general hospital laboratories B.anthracis, forming spores Typical, wavy chains of bacilli, appearance like railway trucks B. anthracis toxins • Lethal toxin (LeTx): intracellular endopeptidase, probably directly damages endothelial cells; also immunosuppressive. • Oedema toxin (ETx): potent adenyl cyclase; contributes to shock and potentiates LeTx. • Protective antigen: the portion of the binary LeTx and ETx complexes which mediates attachment to target cells Bacillus anthracis: epidemiology • Spores of B. anthracis are widely dispersed in nature: in soil, animal carcases and skins, and items made from skin, wool or hair (eg drums made with animal skins, bags, fur robes, plaster reinforced with horse-hair etc) • It is relatively difficult to infect humans: usually skin inoculation or a large inhalational exposure is required • The organism is therefore classified at biosafety level 3 (CL 3) Anthrax presentations • Inhalational: ‘flu’ followed by mediastinitis and pneumonitis • Cutaneous • Gastrointestinal • Meningitic CUTANEOUS ANTHRAX Most common presentation: Look for black eschar; halo of vesicles; extensive oedema Cutaneous Anthrax: Early lesions (CDC Public Health Image Library) (courtesy AB Christie, Liverpool) Cutaneous Anthrax • 95% of naturally occurring cases • Subcutaneous inoculation of spores • Hands, forearm, head • Incubation: <1 to 7 days • Small painless papule ulcer with marginal vesicles (24-48h) • Painless oedema surrounds lesion • Develops into eschar (2-6 d) • Untreated mortality 20% (treated v. rare) ( CDC. www.bt.cdc.gov/agent/cutaneous.asp) Cutaneous Anthrax Note extensive oedema in relation to lesion size ( CDC www.bt.cdc.gov/agent/cutaneous.asp) Cutaneous Anthrax: Differential Diagnosis • • • • • • Necrotic ulcers Rickettsial eschar (e.g. tick typhus) Pox virus infection (e.g. cowpox, orf) Spider bites Cowpox (courtesy Dr D. Baxby, Liverpool) Cutaneous anthrax: oedema • Rarely, bacteraemia can accompany cutaneous anthrax • Always investigate, and treat sepsis with high-dose IV antibiotic Intestinal Anthrax • Ingestion of contaminated meat • Incubation: <1 - 7 days • Fever, acute abdomen, vomiting, bloody diarrhoea • Intestinal eschar (similar to cutaneous lesion) • Progression to sepsis syndrome • Mortality 50 - 100% despite treatment (Armed Forces Institute of Pathology, USA) Inhalational anthrax • Flu’-like onset, respiratory failure develops abruptly after 3-4 days-fatal in 1 or 2 days • CXR suggestive, but features can be subtle • Blood cultures pos.(CL3) • PCR possible (ref.lab) • responds to early vigorous treatment Jernigan et al. EID 2001; 7: 933 Confirmed anthrax cases associated with bioterrorism: U.S., 2001. A. Geographic location and clinical manifestation of the 11 cases of confirmed inhalational and 7 cases of confirmed cutaneous anthrax. B. Epidemic curve for the 18 confirmed cases of inhalational and cutaneous anthrax and 4 cases of suspected cutaneous anthrax. Progression of chest x-ray findings in a patient with inhalational anthrax. Findings evolved from subtle hilar prominence and right perihilar infiltrate to a progressively widened mediastinum, marked perihilar infiltrates, peribronchial cuffing, and air bronchograms. Recognising inhalational anthrax • 10 cases of inhalational anthrax: USA • WCC 7.5-13.3 x109/l (6 < 10.0) • 6/6 had >70,000 RBCs in pleural fluid, with high protein and low WBCs • 6/6 had PaO2 80mmHg or less on air • 5/7 treated within 5 days of onset survived • 1/3 treated after 5 days survived JA Jernigan et al. EID 2001; 7: 933 Treating inhalational anthrax • Severe chest infection of unknown cause. • DON’T use 3rd gen. Cephalosporin alone. • Use a penicillin eg.coamoxyclav plus a macrolide/ciproflox. • Or add gentamicin. • Antibiotics effective for anthrax. • Ciprofloxacin. • Benzyl penicillin. • Macrolides. • Gentamicin (plus pen.). • Doxycycline. • Chloramphenicol. Vaccination and Prevention • The first successful vaccine for anthrax was developed for animals by Louis Pasteur in 1881. • At present, the single vaccine licensed for human use is a product from the cell-free culture supernatant of an attenuated, nonencapsulated strain of B. anthracis (Stern strain) - anthrax vaccine adsorbed (AVA). • Clinical trials for safety in humans and efficacy in animals are currently under way to evaluate the role of recombinant protective antigen (one of the major components, along with lethal factor and edema factor, of B. anthracis toxins) as an alternative to AVA. • The efficacy of AVA in a postexposure setting in humans has not been established. • The current recommendation for postexposure prophylaxis is 60 days of antibiotics (ciprofloxacin or doxycycline). Chemo-prophylaxis of anthrax Prophylaxis Adult doses Child doses Ciprofloxacin 500mg orally bd 20-30mg/kg bd for 6 weeks Doxycycline (if 100mg orally bd 5mg/kg orally in cipro x tolerated two divided /indicated) doses Although normally used with caution or contraindicated, these drugs may be given in pregnancy, lactation and childhood to protect against anthrax PLAGUE MICROBIOLOGICAL FEATURES: gram-negative, rod-shaped, facultative anaerobic bipolar staining, non-motile, non-sporulating BIOLOGICAL SURVIVAL: 15 minutes in 55° C/ few hours in sunlight weeks in water, grains, moist soil, dry sputum, flea feces lives months/years at just above 0°C HOST RANGE: zoonotic disease of rodents: intracellular organism: rats, mice, ground squirrels monocytes/macrophages => long-term survival requires host => Circumstances for natural human outbreaks: disasters/ disruption of rat habitats/ rat dis- or relocation SYNDROMIC PRESENTATION – SESSION 1 PLAGUE EPIDEMIOLOGY I Since 1965: NATURALLY OCCURING PLAGUE approximately 1500 cases/year 25 countries reported cases 50% Eastern and South Africa, esp. Madagascar 1980-1994: 18,739 cases reported from 20 countries to WHO 2000 – 2005: December 2007: Zambia, Algeria, Malawi, DR Congo n=1, marmoth hunter, China Endemic in U.S. 1947-96: 1970-2003: 83% 15% 2% 390 cases/y 5-15 cases/y Bubonic Septicemic Primary Pneumonic SYNDROMIC PRESENTATION – SESSION 1 PLAGUE TRANSMISSION 4 ROUTES FOR HUMAN INFECTION 1. Flea-bite (most common) => Rat-borne urban epidemics in history => Human overcrowding, indoor contacts 2. Handling infected animals (skin contact, scratch, bite) => Endemic sylvatic plague with sporadic outbreaks => Occupational risks 3. Inhalation of contaminated aerosol (human/animal) => Only pneumonia capable of person to person spread 4. Ingestion of infected meat SYNDROMIC PRESENTATION – SESSION 1 PLAGUE CLINICAL COURSE I 3 TYPES OF DISEASE Bubonic Septicaemic Pneumonic Plague: Clinical Forms Bubonic • Common form of naturally occurring plague, following bite of infected flea • Inguinal, axillary, or cervical lymph nodes are the most commonly affected • 80% can become bacteraemic • 60% mortality if untreated (CDC image library) SYNDROMIC PRESENTATION – SESSION 1 PLAGUE CLINICAL COURSE II 1. “CLASSIC” Bubonic Plague ENTRY: Bite of infectious flea Contact/ ingestion of infected animals Contact/ ingestion of infectious material BUBOES: Enlarged tender lymphnodes (unilateral) Usually inguinal/ femoral in adults Cervical/ submaxillary common < 10y CFR: 40-60% untreated, <5% treated Overall 14% in U.S. (delayed diagnosis/ therapy) COMPLICATION: BACTERAEMIA secondary septicaemic plague secondary pneumonic plague secondary plague meningitis www.cdc.gov 3. Pneumonic Plague US cases: 2% 12% PRIMARY PNEUMONIC SECONDARY PNEUMONIC PRIMARY: Result of droplet inhalation Only few cases in endemic areas ENTRY: Aerosol => other patients/ infected animals/ BW SECONDARY: Hematogenously spread to lungs Initially: interstitial pattern/ later: abscess CFR: ~ 100% if untreated/ therapy delayed > 18-24h after onset Remains high despite treatment: Overall 57% (U.S.) DEATH WITHIN 2-4 DAYS (max 6d): cyanosis, stridor, resp. failure Plague: Differential Diagnosis Pneumonic • Bioterrorism threats • Anthrax - Tularaemia - Melioidosis Bubonic • Staph/strep adenitis • Glandular tularaemia • Other pneumonias, esp. “atypicals” Septicaemic • Other Gram-negative sepsis • Meningococcaemia • Rickettsia • Leptospirosis (haemorrhagic) • Cat scratch disease • LGV & chancroid SYNDROMIC PRESENTATION – SESSION 1 PLAGUE TREATMENT FIRST LINE: STREPTOMYCIN CHILDREN: ADULTS: =>bacteriocidal 30 mg/kg IM divided q8-12h (max 2g/day) 1g IM bid GENTAMYCIN CHILDREN: ADULTS: => as effective, qd dosage 2.5mg/kg im/iv q8h 5mg/kg iv qd (check levels) OR load 2mg/kg, then 1.7mg/kg q8h SECOND LINE: DOXYCYCLIN => good in vitro + good human data 1. Single 200mg iv loading dose 2. 100mg iv bid or 200 mg iv qd adults/ kids >45kg => 1st choice po therapy for mass casualties/ PEP Smallpox The variola virus • A member of the family of Orthopoxviridae • The largest viral genome: double-stranded DNA • An enveloped virus, but the envelope is not essential for infectiousness The Yugoslavia outbreak 1972 • Single index case spent time in Iraq – 11 contacts developed smallpox • 100 secondary cases in contacts and other hospital patients • 14 tertiary cases • Spread to other cities • Total 175 cases, 35 deaths Variola: first and second day of rash (4th-5th day of fever) Variola: 4th day of rash •For the first time-on the fourth day of the rash and the fifth day of infectiousness, a typical vesicular appearance is seen Variola major: drying rash (7-9 days) •The rash is becoming less infectious •Conjunctival lesions are usually benign and heal completely Variola major: confluent on day 7 of rash Variola major: scabbing of rash: day 11 Smallpox Clinical Course • Prodrome (day 13) • Erythematous rash (days 2-3) • Maculopapular rash (days 4-6) • Vesicular pustular rash (days 8-14+) (Fenner F et al. Smallpox and its eradication. WHO 1998. http://whqlibdoc.who.int/smallpox/9241561106.pdf ) Variola major: variation in severity Boys aged 13 years, infected from the same source-admitted same day: right-unvaccinated; left-vaccinated in infancy Diagnosis of smallpox: (must be in CL4 facility) • Classical tests EM of vesicle fluid for poxvirus Virus culture (CFT and ELISA for plasma antibodies-not reliable) PCR: rapid, specific, can distinguish between poxvirusesperformed on blood or vesicle fluid Smallpox vs. Chickenpox • • • • • • • • • • • Smallpox Incubation 7-17d Severe illness Prodrome Headache and back pain Centrifugal Synchronous Rash not initially itchy Lesions round Scabs form 10-14d Scabs separate 14-28d • • • • • • • • • • • Chicken pox Incubation 14-21 d Usually mild Prodrome Mild malaise Centripetal Asynchronous Rash initially itchy Lesions oval Scabs form 4-7d Scabs separate <14d Management of smallpox • General supportive measures • Analgesia (the rash is very painful) • Good hygiene (secondary infection is a danger-the skin is a common portal of entry) • Antibiotics to treat secondary infection and limit scarring • ?antiviral drugs Smallpox vaccine • Live vaccinia vaccines Lister-Elstree NYCBH 2nd generation live (Modified vaccinia and others) • Given by scarification MELIOIDOSIS – – – – – Burkholderia pseudomallei Aerobic, gram-negative, motile bacillus Found in water and moist soil Opportunistic pathogen Produces exotoxins Can survive in phagocytic cells • Latent infections common SYNDROMIC PRESENTATION – SESSION 1 MELIOIDOSIS V Epidemiology II disease of rice farmers endemic in tropics and subtropics: Southeast Asia, Australia, the Middle East, India, China, Caribbean U.S. and EU cases linked with travel abroad SYNDROMIC PRESENTATION – SESSION 1 MELIOIDOSIS VI Epidemiology III Clinical disease uncommon in endemic areas – antibodies in 5-20% of agricultural workers – no history of disease Seasonal increase (wet season) – heavy rainfall – high humidity or temperature SYNDROMIC PRESENTATION – SESSION 1 MELIOIDOSIS VIII Transmission WOUND INFECTION – Contact with contaminated soil or water INGESTION – Contaminated water INHALATION – Dust/ contaminated soil RARELY – Person-to-person – Animal-to-person SYNDROMIC PRESENTATION – SESSION 1 MELIOIDOSIS IX Clinical Course I INCUBATION PERIOD: 1-21 days (~ 9 days) up to 30 years Always Fever, chills, malaise Soft tissue: Pulmonary: Septicaemic/disseminated: Abscess Productive cough, dyspnoea Multiple abscesses, Septic shock MOST INFECTIONS ASYMPTOMATIC/ LATENT MODE OF TRANSMISSION INDUCES DIFFERENT CLINICAL FORMS: INOCULATION => INHALATION => Focal (wound) infection Acute pulmonary infection Both can result in secondary SEPTICEMIA CNS involvement is rare SYNDROMIC PRESENTATION – SESSION 1 MELIOIDOSIS X Clinical Course II FOCAL INFECTIONS Abscess/ granuloma formation – Skin – Bone and/or muscle – Joints – Internal organs – Genitourinary – Nervous system (infrequent) SYNDROMIC PRESENTATION – SESSION 1 MELIOIDOSIS XI Clinical Course III ACUTE PULMONARY INFECTION Most common form: High fever, headache Dull aching chest pain Cough, tachypnea, rales Chest X-rays – Upper lobe consolidation – Nodular lesions – Pleural effusion SYNDROMIC PRESENTATION – SESSION 1 MELIOIDOSIS XII Clinical Course IV PULMONARY INFECTION - RADIOLOGY FINDINGS USE CT IF AVAILIABLE ! SYNDROMIC PRESENTATION – SESSION 1 MELIOIDOSIS XIV Diagnosis and prevention DIAGNOSIS: Clinical suspicion => travel to endemic areas low budget, outdoor travel => occupational exposure medical, military Microbiology => Isolation of organism => Various serological tests PREVENTION Avoid contact with soil/water => Chlorination if needed Handling infected animals with care Thorough cleaning of wounds