Contact Lenses - Texas Optometric Association
advertisement

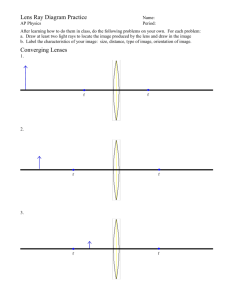
Certified Paraoptometric Assistant Review Course CPOA Provision The Self Study Course for Paraoptometric Assistants and Technicians, Self Assessment Examination, and the AOA PS CPOA Review Course are not prerequisites for taking the paraoptometric certification examination given by the Commission on Paraoptometric Certification (CPC). Using these study materials and/or taking the CPOA Review course does not guarantee passing the paraoptometric certification examination given by the CPC. Attending the CPOA Review Course is not a substitute for studying for the paraoptometric certification examination given by the CPC. This course is designed to review previously acquired knowledge. This review course is not intended to be a substitute for responsible study and preparation for the CPOA test. Outline Office Operations (13%) Ophthalmic Optics and Dispensing (20%) Testing and Procedures (20%) Special Procedures (17%) Refractive Status of the Eye and Binocularity (13%) Basic Ocular Anatomy and Physiology (17%) Office Operations (13%) Office Procedures Office Procedures Manual “Official rulebook of the practice” Used to clarify the policies of the practice Records Management Filing Systems Alphabetical Simplest and most widely used Numerical Decreased chance of misfiling Cross index card required Recall Systems Types of Patient Recall Pre-appoint (most effective) Postcard or letter Computerized Recall list generated Email Record Corrections Recording errors can happen - What to do? Draw a single line through the error Initial Example: Monday, June 29, 3008 sjm 2008 Never, never erase to completely remove Confidentiality What is HIPAA? Health Information Portability & Accountability Act Minimum Necessary Principle Requires office to take reasonable steps to limit the use or disclosure of, and request for, PHI to the minimum necessary to accomplish intended purpose HIPAA Regulations Confidentiality Safeguards Release of records Legal record of ownership Release of records Computer use Patient Handling Telephone Techniques Greeting Taking messages Handling requests for information Handling complaints Making appointments Confirming appointments Patient Flow Control the appointment schedule Have thorough knowledge of different types of appointments and time required by each doctor for specific appointments Public Relations Types of correspondence and brochures “Welcome to the practice” Referral letters Consultation letters School reports Legal reports Patient information pamphlet Patient Handling Triage Categories Emergency - immediate Urgent - 12-24 hours Routine - next available appointment Ask questions to determine Bookkeeping Procedures Accounts Receivable Accounts Payable Petty cash Banking Procedures Deposits Reconciling bank statements Office Finances Presentation of fees Do not apologize Collection of fees Cash, check or credit card? Professional Issues Role and function of the eye care professional Delegation Certification vs. licensure Liability and Malpractice Paraoptometrics are: Responsible to provide the highest level of service possible Protected under the employing doctor of optometry’s malpractice insurance Conduct, Confidentiality & Ethics To keep the patient’s visual welfare uppermost at all times To strive to see that no person shall lack for visual care To conduct ourselves as exemplary citizens To promote and maintain cordial and unselfish relationships with members of our profession Excerpts from “Code of Ethics” adopted by the House of Delegates of the AOA June 28, 1944, Modified in 2005 Hygiene & Infection Control Asepsis Hand washing Instrument disinfection Contact lens disinfection Cross-contamination Sterilization Ophthalmic Optics & Dispensing (20%) Prescriptions Components Sphere, cylinder, axis Add power Prism Prism base direction Ordering should include: Jones Optical 5209 South Penn Oklahoma City, OK 73109 638-7889 Whether on order form or online ordering Patient SPH Jane Doe CYL DEC In +1.00 - 0.25 90 +1.00 - 1.00 Seg Ht. 95 Width 2/23/01 Date AXIS OD PRISM PLASTIC GLASS Out 1/2 Δ BU SV FDA Tested 1/2 Δ Pup BD Dist RND EXEC ST 28 LENT TRIFOCAL OS A D +2.00 20 D +2.00 20 Set F.P.D. F R A M E S Size 58 ACCT: 28 Insert Total R R Dist L L 66 Lens Shape A B BDG 16 ED LOC UNCUT Near 62 OTHER Edge Rimless Grove Drill Metal ZYL Temp Style 145 Safilo Titanium 109 REMARK SUPPLY Color Gray OT30 TRAY# Colour PINK 1 2 3 GREEN 1 2 3 GRAY 1 2 3 BROWN 1 2 3 OTHER: 1 2 3 GRADIENT TO Lite RX LENS MISC TAX TOTAL DATE INVOICE $ Clear Optical Cross Optical cross is a diagram that denotes the dioptric power in the two principal meridians of a lens. Hint: Think of the value of the numbers as they are read off of the lensometer wheel. Lens Clock Readings Example +8.00 -5.00 Image from Sharp- Trawick +8.00 Front Lens Surface -3.00 Back Lens Surface Optical Cross Optical Cross Results Plus cylinder notation: + 3.00 +3.00 +2.00 x 090 + 5.00 Minus cylinder notation: +5.00 -2.00 x 180 Hint: The sphere is “married” to the axis; the cylinder is the distance between the numbers on the cross Prescriptions: Transposition Transposition Combine the sphere and cylinder power mathematically Change the sign of the cylinder Change the axis by 90 degrees Hint: When combining positive and negative numbers, think in terms of money. Example: -2.00 combined with +0.50 If you are $2.00 “in the hole” and you deposit $0.50, what is your balance? Answer: $1.50 “in the hole”, or -1.50. Prescriptions: Transposition Transposition Examples -1.00 +2.00 X 160 +1.00 -2.00 x 070 +1.25 -0.75 x 030 +0.50 +0.75 x 120 Plano +1.00 x 090 +1.00 -1.00 x 180 Prescriptions: Decentration Decentration calculations Eye size plus distance between lenses minus patient’s PD divided by 2. Example: Eye size = 58 +16 = 74 Patient’s PD = 62 74 – 62 = 12 12 divided by 2 = 6 Prescriptions: Vertex Power Vertex Distance- distance between the ophthalmic lens and the front of the patient’s eye Effective Power- change in the prescription when the distance varies from the normally refracted 13.5mm distance to where the patient wears the RX. Concerned with high Rx’s (-/+ 4.00) Prescriptions: Vertex Power Vertex distance and effective power Lenses gain minus or lose plus power as they are moved closer to the eye. Conversely lenses gain plus or lose minus as they are moved away from the eye. Instruments used for verification Lensometer Lens power and axis location Presence, amount and direction of prism Caliper Lens thickness Instruments used for verification Colmascope or Polariscope Progressive add markings Geneva Lens Clock Base curve Prescriptions: Prentice’s Formula Prentice’s Prism Formula – if the patient is not looking through the optical center of the lens that has power, they are looking through prism Optical Center Induced Prism What Does Prism Do? Displaces light Light bends toward base Image displaced toward apex Verification of Prism Determine optical center of lens Compare with patient’s pupillary distance for horizontal prism (base in or base out) Compare with patient’s line of sight (LOS) for vertical prism (base up or base down) To Determine Base Direction Prescriptions: Prentice’s Formula Prentice’s Prism Formula Prism = power x decentration (in cm) Prism = lens power (in diopters) multiplied by d in cm (Where d = amount the patient PD varies from the major reference point in cm) EX: -4.00(power) x .5cm (decentration in cm) = 2 prism diopters Optics: Light Rays Rays move from left to right Converging Rays Diverging Rays Prescriptions: Focal Length Calculations Formula: f (in meters) = 1/D Focal length in meters (f) = 1 / D (reciprocal of power in diopters) Example: The focal length of 2.00 D lens: f = 1 / 2.00 D f = .5 meter Major Reference Point The optical center of each lens Also referred to as “prism reference point” Point of intersection of the sphere indicators and cylinder indicators during lensometry Prescription: Prism Prescribed when the two eyes do not align properly Can be induced when the optical centers of the lenses do not line up with the patient’s PD Prentice’s Rule- used to calculate induced prism Lenses: Convex & Concave Plus lenses – prisms stacked base to base Minus lenses – prisms stacked apex to apex Lens Forms Convex Concave Spherical Lens A lens with the same curvature across the surface Toric/Cylindrical Lens A lens that differs in curvature across the surface Flat Meridian Steep Meridian Base Curve The measure of the general shape of the lens Used to determine lens power Prescription Forms Plus cylinder Cylinder is ground on front of lens -2.00 + 1.25 x 090 Minus cylinder Cylinder is ground on back of lens Most typically used form -0.75 – 1.25 x 180 Basic Ophthalmic Lens Types and Styles Single vision Spherical lenses Planocylindrical lenses Spherocylindrical lenses Aspheric lenses Multi-focal lenses Bifocal lenses Trifocal lenses Progressive addition lenses Powers of the lens Bifocal The amount of power needed to be added to the distance correction Example: -2.00 -0.75 x 090 +1.00 add Bifocal power = -1.00 -0.75 x 090 Courtesy of MattisonShupnick & Meister Powers of the lens Trifocal Generally the top segment is ½ the power of the lower segment Progressive Addition Lens Multiple powers increasing upon downward gaze Images courtesy of Mattison-Shupnick & Meister Multifocal Placement Bifocal Seg Height Trifocal Seg Height Lens Materials: Glass Crown glass Flint glass Hi-Index glass n: 1.52 n: 1.65 n: 1.9 Advantages: More scratch resistant, clearer optics Disadvantages: Heavier, less impact resistant Lens Materials: Plastic CR-39 Hi-Index plastic n: 1.49 n: 1.54-1.60 Advantages: Lighter weight, more impact resistant compared to glass, easily tinted Disadvantages: More prone to scratches, less ultra-violet (UV) protection on untreated lens Lens Materials: Polycarbonate Polycarbonate n: 1.54-1.60 Advantages: Lighter weight, more impact resistant compared to plastic, naturally filters UV light. Disadvantages: More prone to scratches, chromatic aberration Lens Materials: Trivex™ Trivex ™ n: 1.53 Advantages: Lightest material available; less distortion; as impact resistant as polycarbonite, highly resistant to cracking around holes when used in drill mount frames; quality optics; natural UV protection. Disadvantages: Cannot be tinted darker than #2 Lenses: Index of Refraction Definition: A comparison, or ratio, of the speed of light in air to the speed of light in another medium Values Speed of light in air: 186,000 mps Air= 1.00 Water= 1.33 Lenses: Index of Refraction Index of refraction (n)= Speed of light in air/speed of light in material Hardening Methods For impact resistance Heat tempering Lens placed in a vacuum and brought close to melting point, then cooled rapidly Chemical tempering Lens placed in hot chemical bath for 15 – 17 hours ANSI Standards American National Standards Institute Regulates the standard of tolerances for ophthalmic lenses Copy of ANSI Standards kept by lensometer Z80.1 Impact resistance standard Impact resistance of lenses subject to individual test shall be measured with a 15.9 mm (5/8 inch) diameter steel ball weighing not less than 16g (0.56 oz) dropped from a height of not less than 127cm (50 inches) or an equivalent impact Z87.1 Basic Impact Standard Impact resistance of lenses subject to individual test shall be measured with a 1 inch diameter steel ball dropped from a height of not less than 127 cm (50 inches) or an equivalent impact High-Impact Standard Impact resistance of lenses subject to individual test shall be measured with a ¼ inch BB fired at a rate of 150 feet/second FDA Standards Food and Drug Administration Regulates the pharmaceuticals that are used. Approves methods for disinfection Special Prescription Considerations High Minus/ Myodisc Aphakia / Lenticular Aspheric Fresnel Prisms Industrial / Occupational Tints and Coatings Colors Tint #1 – 65-80 light transmission Tint #2 – 45-60 light transmission Tint #3 – 15-40 light transmission Mirror Edge Coating Sun and Glare Protections Polarized Lens Photochromatic Ophthalmic Lens Coatings Scratch resistant Anti-reflective Ultra-violet Frames Styles Full frame Semi rimless Rimless Frame Materials Materials Zyl Metal Stainless Steel Memory Metals Anatomy of the Frame Frame front Eyewire Bridge Hinge Nosepads Temples Guard Arm Eyewire Frames Verification Do Not Assume… Verify Eyewire size Bridge Temple length Standard Frame Alignment Evaluate frame front Evaluate for X-ing of the bridge Evaluate eyewire for X-ing Make sure frame front is even Temple alignment follows front alignment Evaluate endpieces Evaluate hinges Evaluate temples for 90-degree angles Do temples close evenly Eyewear Dispensing 4 Point touch Tools Used For Frame Adjustments Frame warmer Adjusting Pliers Nose pad adjusting pliers Needle nose Half round/ Flat jawed Angling Dispensing -Frame Alignment Front- Xing Coplanar Face form - positive and negative Frame Tilts Pantoscopic Retroscopic Nosepad Adjustments As viewed from front of frame Vertical Angle Bottoms of pads angled toward frame front Frontal Angle Tops of pads angled inward approximately 15 degrees Nosepad Adjustments Splay Angle Edge of pads angled inward approximately 15 degrees Patient Instructions Frames Place and remove eyewear with two hands Temples should be folded and stored in frame case Frame should be cleaned daily with mild soap and water Patient Instructions Lenses Cleaned as often as necessary with recommended solutions Frame Repair Eyewire screw replacements Nylon chord replacements Realignments Common Frame Adjustment Problems - Vertex Distance Increase vertex - bend both end pieces in Decrease vertex - bend both end pieces out Increasing vertex distance effectively raises multifocal height and vise versa Changing Height or Vertex Distance Moving pad arms up will raise height of frame Moving pad arms down will lower height of frame Lengthening pad arms will increase vertex distance Shortening pad arms will decrease vertex distance Adjustment Problem Unequal Vertex Distance Unequal temple spread Decrease temple spread on side that is closer (In - In) Increase temple spread on side that is farther from face (out - out) Unequal temple tension and bends behind ears Adjustment Problems Crooked Frames One eyewire higher: bend the temple up on that side to lower One eyewire lower: bend the temple down on that side to raise Testing and Procedures (20%) Case History Chief complaint Reason for visit – recorded in patient’s own words History of present illness Detailed information on chief complaint Social history (age-appropriate) Alcohol? Smoke? Occupation? Live alone? Ocular Symptions Ask open-ended questions Itching Burning Tearing Redness Irritation Blurred vision Other symptoms Ocular History Inquire on specific ocular problems or conditions Surgery Injury Vision training Eye medications Refractive history Ocular History Inquire on specific ocular problems and conditions, such as: Glaucoma Cataracts Keratoconus General Health History Rule out specific health problems Current health status Diabetes High blood pressure Heart disease Other Family Ocular History Review Family History of Cataracts Glaucoma Macular Degeneration Other Who has been diagnosed with ? Medications Name Pharmaceutical and Over-the counter Quantity Frequency Prescribed for Does the patient take the medication as directed? Allergies Medications True allergies vs. side effects Environmental How does patient gain relief? Refractive History Past history of corrective lenses Current corrective wear Age of correction State of correction Quality of vision Visual Acuity: Snellen Fraction Numerator Represents the testing distance in feet or meters 20/_____; 6/______ Denominator Represents the distance at which the letter subtends a 5-minute angle of arc in distance or meters. Also referred to as the letter size. Visual Acuity: Techniques for Testing Monocular and binocular With and without Rx Distance and near Pinhole acuity Testing errors Types of Acuity Charts Snellen Metric (Bailey-Lovie) Low vision vharts Illiterate vharts Landolt “C” or rings Tumbling “E” Lighthouse charts Pinhole Acuity To determine if reduction in vision is due to refractive error Vision Acuities Testing Distances Distance testing 20 feet or 6 meters is customary Or Mirror method to assimilate equal distance Recording Results The smallest line patient can read If patient is able to read all of one line and one two of next, then 20/25 +2 or 20/25+ If patient is consistently misses one letter, then 20/20-1 or 20/20- Interpupillary Distance Measurement Distance and near 1 PD measuring ruler 2 3 4 5 6 7 1st measurement 60 mm Pupillometer 1 2 3 4 5 6 7 2nd measurement 64 mm Monocular PD measurement Near Point of Convergence Measure of the ability of both eyes to work together Blur/break/recovery Measured in centimeters from the bridge of the nose to the point of blur/break Near Point of Accommodation Ability of the eyes to focus at near Binocular measurement Amplitude of accommodation Binocular or monocular measurement Distance measured in cm Extra-Ocular Muscle Testing Pursuits Movement of the eyes while following a moving target Saccades Jumping movements from one target to another Cover Test Assess heterophoria and heterotropia Two separate tests - unilateral and alternate Tests are performed at distance and near Unilateral test is performed first Unilateral Cover Test Determines heterophoria or heterotropia Heterophoria = tendency Heterotropia = constant Determines frequency (constant or intermittent) Unilateral or alternating Alternating Cover Test Determines the direction and magnitude of the tropia or phoria Eso - in Exo - out Exo Hyper - up Hypo - down Hyper Eso Hypo Eye Dominancy Eye preference Eye used for monocular viewing or sighting Testing methods Reasons for recording Monovision contact lenses Fusion / Suppression Fusion Blending of 2 images, one from each eye Suppression Subconscious inhibition of an eye’s retinal image Associated with strabismus Worth 4 Dot Maddox Rod Dissociating test One eye sees a red line, the other a white light Pupillary Responses Assure that the sensory pathway is working Direct and consensual responses to light Response to accommodation Pupillary Response Recording Example #1 P= pupils are E= equal R= round R= react to L= light and A= accommodation -/+RAPD (relative afferent pupillary defect Example #2: 5mm/4mm 2+ (reaction time) R & R (round & reactive) -/+ RAPD (also called Marcus Gunn pupil) Confrontation Fields Screening for gross visual field defects Comparison of examiner’s visual field (known) to the patient’s (unknown) Color Vision Types of color vision tests Pseudoisochromatic plates (PIP) Farnsworth D-15 Farnsworth 100 hue Nagel Anomaloscope Color Vision: Method for Testing Monocular vs. binocular Test distance 75 cm (30 inches) Illumination Macbeth daylight lamp Illuminant C lamp Pseudoisochromatic Plates Ishihara 14, 24, or 38 plates Plate #1 can be read by anyone, even those with color defects Pseudoisochromatic Plates Hardy-Rand Ritter (HRR) Screening test to separate those with defective color vision from those with normal color vision Classifies the type of defect Indicates the extent of the defect (mild, medium, strong) Courtesy of Richmond Products Farnsworth Dichotomous (D15) Used to separate medium and strong color defect vs. normal Courtesy of Richmond Products Farnsworth Dichotomous (D15) Patient color disk selection is shown in color, test results are plotted and diagnosis is recommended. Courtesy of Richmond Products Farnsworth 100 Hue Test 93 Colored Discs Tray Scoring Template Calculates a numerical score Courtesy of Richmond Products Anomaloscope The software provides capability for data analysis and display. Courtesy of Richmond Products Color Vision Classifications Trichromatism Normal color vision Protanope Red deficiency Deuteranope Green deficiency Tritanope Blue-yellow deficiency Normal Dichromat (red insensitive) Stereopsis Highest degree of depth perception Purpose of test Types of stereo tests Titmus stereo fly Randot Reindeer Butterfly Stereo Testing: Method for Testing Illumination (well-lit room light) Testing distance 40 cm (16 inches) Patient wears habitual Rx for near Recording - in seconds of arc Cat = 400 seconds of arc Rabbit = 200 seconds of arc Monkey = 100 seconds of arc Exam Equipment Retinoscope Phoropter Keratometer Exam Equipment Monocular Direct Ophthalmoscope Binocular Indirect Ophthalmoscope Biomicroscope Exam Equipment Optical Coherence Tomographer Special Procedures (17%) Hard Contact Lens Materials 1940s, 50s, 60s Polymethylmethacrylate (PMMA) 1970s Rigid Gas-permeable (RGP) Silicone Acrylate Fluoro-Silicone Acrylate Parameters Gas Permeable Lenses Overall Diameter Optical Zone Diameter Back Vertex Power Base Curve Radius Peripheral Curves Edge and Center Thickness Parameters Overall Diameter (OAD) Secondary Curve Width (SCW) Optical Zone (OZ) Secondary Curve (SC) Peripheral Curve Width (PCW) Peripheral Curve (PC) Contact Lenses Materials 1970s Soft Hydrogel (water-absorbing) Silicon Hydrogels Comparison of Soft and GP Lens Advantages Soft Lens Good initial comfort Variable wearing time Occasional wear Ability to enhance or change eye color Stability in sports Comparison of Soft and GP Lens Advantages Gas Permeable Clear, sharp vision Long-term comfort Stability/durability Ease of care Good ocular health Corrects small and large amounts of astigmatism Care and Handling Hygiene Hands Case Evaluate lens Tears Inverted Lint Solutions Soft contact lens solution for soft contact lenses Hard contact lens solution for RGP’s Soft Contact Lens Insertion Place lens on finger tip Verify lens is not inside out Taco Test Manipulate lids for aperture Place lens on eye Release lower lid, then upper lid Soft Contact Lens Removal Pull lower lid down Pinch lens off the white part of eye Remove Reverse hand positions for second eye Hard & GP Contact Lens Insertion Place the lens on the tip of middle finger of the dominant hand Looking down, pull up the top lid with the other hand, pressing it against the bony margin of the top brow Looking ahead, pull down the lower lid with the first or third finger of the “lens” hand. Place the lens on the center of the eye Hard & GP Contact Lens Removal Bend head over table and look straight ahead, opening eyes as wide as possible Place the fingertips of your index finger at the outer corner of the eye Pull the lids laterally toward the ear, blink, and catch the lens in the other hand held close to the eye Contact Lens Wearing Modalities Daily wear Flexible wear Extended wear Contact Lenses Wearing Schedules Soft lenses 4-6 hours plus 2 each day to full time wear Gas Permeable lenses 4 hours plus 1-2 each day to full time wear What is “Normal” Adaptation? Appearance Comfort Vision Lens Care Regimens Soft lens care systems clean rinse disinfect & store protein removal Gas permeable care systems clean rinse disinfect & store protein removal Blurred Vision – Soft Lenses Residual astigmatism Switched lenses Inverted lens Coated lens Dry lens Poor fit Wrong prescription Blurred Vision – Gas Permeable Non-wetting lens surface Switched lenses Warped lens Poor optical quality Coated lens Poor fit Wrong prescription Poor Lens Comfort Soft Lenses Tear Poor edge Dryness Poor fit Dirty lens Gas Permeable Poor wetting surface Poor blend Bad edge Redness Adverse reaction to solutions Uncomfortable edge Wrong solutions used on lenses Foreign body Excessive movement Improper application Contact Lenses Verification Lensometer measures the vertex power Contact Lenses Verification Radiuscope measures the base curve Contact Lenses Verification Hand Magnifier - measures the overall diameter (OAD), optic zone (OZ), peripheral curve widths (PCW, SCW) Contact Lenses Verification V-Gauge or Slot Gauge - measures the overall diameter (OAD) Contact Lenses Verification Shadowgraphmagnifies and projects the contact lens Special Lens Designs and Uses Ballast Toric Truncation Tints Bifocal Ordering Procedures CONTACT LENS ORDER FORM Patient Name: John Doe Specifications Ordered Date 2/23/01 O.D. B.C.R 7.89 S.C.R./W 8.90 /.3 I.C.R./W P.C.R./W 110.9 /.3 O.Z.D. 8.0 Dia 9.2 Power - 2.50 C.T. .16 Blend Med Tint Blue Dot O.D. Additional Information Accepted Rejected Reason for return/reorder Specifications Verified Date O.S. 7.81 8.80 /.3 10.8 /.3 8.0 9.2 - 2.50 .16 Med Blue O.D. B.C.R S.C.R./W I.C.R./W P.C.R./W O.Z.D. Dia Power C.T. Blend Tint Verified by Returned for Credit Date Returned O.S. Tonometry Tonometry is the measurement of intraocular pressure (IOP) Tonometer Types Indentation - Schiotz Applanation - Goldmann; Tonopen Non Contact Schiotz (Indentation) Goldman Applanation Tonopen Perkin’s Hand-held Applanation Tonometer Non-contact Tonometer Classification of Visual Field Defects Nerve Fiber Layer Optic Chiasm Optic Tract to Visual Cortex Arcuate Scotoma Heteronymous Bitemporal Hemianopsia Homonymous Hemianopsia Paracentral Scotoma Congruent Nasal Step Incongruent Monocular Visual Field Boundaries 60 Degrees superiorly 75 Degrees inferiorly 105 Degrees temporally 60 Degrees nasally Physiological Blind Spot 15 Degrees temporal to fixation Absolute scotoma Types Of Visual Field Testing Confrontation Types Of Visual Field Testing Tangent Screen Types Of Visual Field Testing Autoplot Types Of Visual Field Testing Amsler Grid Types Of Visual Field Testing Goldmann bowl perimeter Types Of Visual Field Testing Automated Visual Field Procedures Test Distance Automated – set Tangent Screen – 1 meter or 2 meters Goldmann Bowl – set Amsler Grid- 28 cm – 30 cm Confrontation fields – 2 feet (approx 1 meter) Patient Positioning Forehead touching bar Trial lens very close to the eye Scotoma Absolute Brightest and largest target is unseen Relative Target is seen based on size and brightness Sphygmomanometry (Blood Pressure Measurement) Incidence of hypertension Patient position Critical Time Factors in Measuring How Is The Test Performed? Wrap the blood pressure cuff around the upper arm about 1 inch above the bend of the elbow Place the earpiece of the stethoscope into your ears Place the head of the stethoscope over the brachial artery Make sure that the valve is closed on the cuff. How Is The Test Performed? Inflate the cuff to approximately 20-30 mmHg (millimeters of mercury) higher than the systolic pressure Open the valve slowly Record the number from the sphygmomanometer when the pulse is first heard This is the systolic pressure How Is The Test Performed? Continue releasing the valve The pulse will disappear Record this number This is the diastolic pressure Release the rest of the air and remove the cuff Readings Normal The “normal” for adults is approximately 120mmHg /between 70-80mmHg Abnormal Mild Hypertension - 145-159mmHg/90104mmHg Severe Hypertension - 160mmHg or more/100mmHg or more Hypotension - Below normal blood pressure First Aid/CPR Emergencies Non-ocular involvement Fainting, seizures, CPR Ocular involvement Triage Certification of Health Care Providers Low Vision Define legally blind 20/200 BCV or less than 200 VF in best eye Microscopes and magnifiers Large Print Materials Training Psychological impact – patient motivation Surgery Refractive PRK LASIK LASEK Cataract (phacoemulsification) Yag Laser Posterior capsulotomy Iridotomy Refractive Status of the Eye and Binocularity (13%) Myopia (Nearsighted) Axial Myopia: Axial length of eye is too long, causing the rays of light to come to a point of focus before hitting the retina. Hyperopia (Farsighted) Axial Hyperopia: Axial length of eye is too short, causing the rays of light to come to a point of focus after hitting the retina. Astigmatism Light rays focus at different points. Cornea is not equal in all meridians football vs. baseball Types of Astigmatism Simple - one ray is focused on the retina; the other is focused either in front of (myopic) or behind (hyperopic) Compound - both rays are focused in front of (myopic) or behind (hyperopic) Mixed - one ray is focused in front (myopic) and one ray is focused behind (hyperopic) Oblique - the axis lies in a position that is not vertical (900) or horizontal (1800) Irregular - cannot correct with eyeglass lens Presbyopia Reduction in the ability to accommodate Occurs normally with age Reduction in lens elasticity Reduction in strength of the ciliary muscle Refractive vs. Axial Refractive causes of myopia, hyperopia and astigmatism refer to the fact that the “error” lies within the shape of the cornea and/or the lens Axial causes refer to the length of the eyeball itself being the cause of the “error” Aphakia Absence of the crystalline lens Cataract Most common cause of surgical removal of the lens Correction Intraocular lens implant (IOL): Pseudophakia Contact lenses Spectacle lenses Anisometropia Condition of unequal refractive state of the two eyes An- not iso- same metric- measure Aniseikonia Difference in the size of the two retinal images Inherent and acquired Amblyopia Reduced visual acuity No apparent cause Not correctable with refractive means Strabismic - Amblyopia Ex Anopsia Abnormal binocularity, resulting in suppression of one eye Refractive Uncorrected refractive error that remains uncorrected for a significant period of time Eye Movements Binocularity Teaming of the two eyes Versions Parallel movement of both eyes Ductions Range of movement in one eye, independent of the other eye Eye Movements Pursuits Slow movement of both eye that allow for following an object Saccades Rapid movement of both eyes in the same direction Eye Movements Convergence Inward movement of both eyes towards each other Divergence Outward movement of the eyes Eye Movements Fusion Ability of the two eyes to create one image Suppression Unconscious mechanism to avoid double vision EYE MOVEMENTS Phorias Latent tendency of the eye to deviate Prevented by fusion Occurs only when fusion is broken Tropias Constant deviation of the eye Accommodation Crystalline lens Maintains focus as objects come closer (accommodation) Basic Ocular Anatomy and Physiology (17%) The Globe Three spheres or “tunics” Fibrous Vascular Nervous Courtesy: National Eye Institute, National Institutes of Health Fibrous Tunic Sclera Episclera Cornea Courtesy: National Eye Institute, National Institutes of Health Vascular Tunic Iris Ciliary body Choroid Courtesy: National Eye Institute, National Institutes of Health Nervous Tunic Retina Courtesy: National Eye Institute, National Institutes of Health Orbit Orbit Bony socket that contains the eye and most of the accessory organs Seven bones Sutures Foramen Sinuses Orbital Bones Frontal bone Ethmoid bone Palatine bone Zygomatic bone Lacrimal bone Maxillary bone Sphenoid bone (Located further behind the zygomatic bone-hidden from view) Anterior Adnexa 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. Upper eyelid Lower eyelid Lateral canthus Medial canthus Caruncle Limbus Iris Pupil Puncta Sclera Plica Semilunaris National Library of Medicine (NLM Anterior Adnexa Eyelids Distribute the tear film across the front surface of the eye Protect the eye from light and debris Reflex blinking versus blepharospasm Lacrimal System Lacrimal gland Punctum Canaliculus Nasolacrimal sac Nasolacrimal duct National Library of Medicine (NLM Tear Film Layers Lipid Meibomian glands Aqueous Lacrimal gland Mucus Goblet cells of conjunctiva Cornea First and most powerful refracting medium of the eye 5 Layers Epithelium (anterior) Bowman’s membrane Stroma (middle) Descemet’s membrane Endothelium (posterior) Courtesy: National Eye Institute, National Institutes of Health Crystalline Lens Nucleus Cortex Capsule Accommodation Cataract Courtesy: National Eye Institute, National Institutes of Health Vitreous Gel-like substance found in the eye (in the vitreous chamber). Helps to keep the shape of the eye. Courtesy: National Eye Institute, National Institutes of Health Extraocular Muscles Rectus (4) Medial (in-adduct) Lateral (out-abduct) Superior (up-elevation) Inferior (down-depression) Oblique (2) Superior (down & in) Inferior (up & in) National Library of Medicine (NLM The Visual Pathway Optic nerve Optic chiasm Optic tract Lateral geniculate body Optic radiations Visual cortex Image courtesy of Posit Science Conjunctiva Translucent membrane that lines the inner surface of the lids (palpebral) and the outer surface of the globe (bulbar) Fornices - where the palpebral and the bulbar conjunctiva meet National Library of Medicine (NLM) Retina Macula Fovea Cones Peripheral retina Rods Optic disc Cup Courtesy: National Eye Institute, National Institutes of Health Common Pathological & Functional Disorders Entropion Eyelids turn inward Ectropion Eyelids turn outward Ptosis Drooping of the eyelid Common Pathological & Functional Disorders Conjunctivitis Also called “pink eye” Inflammation of the conjunctiva Bacterial Allergic (contact) Vernal (seasonal) Giant papillary (associated with CTL wear) Viral Eyemaginations Common Pathological & Functional Disorders Glaucoma Characterized by increase in intraocular pressure, increased size of optic cup and visual field defects Chronic open-angle Acute angle-closure Congenital Narrow angle Low tension Secondary Courtesy: National Eye Institute, National Institutes of Health Common Pathological & Functional Disorders Cataract Opacity of the crystalline lens Nuclear sclerosis Cortical Secondary Traumatic Congenital Posterior subcapsular Courtesy: National Eye Institute, National Institutes of Health Common Pathological & Functional Disorders Corneal problems Ulcers Dystrophy Abrasion Common Pathological & Functional Disorders Dry eye Also called “Keratitis sicca” or “Keratoconjunctivitis sicca” Pathological condition of corneal and conjunctival dryness due to decreased production of tears Common Pathological & Functional Disorders Retinal Disorders Detachment Retinopathy Diabetic Hypertensive Degeneration Lattice Macular Macular Degeneration Courtesy: National Eye Institute, National Institutes of Health Ocular Pharmacology Diagnostic agents Therapeutic agents Ocular Pharmacology Mydriatic - dilates the pupil Phenylephrine Miotic - constricts the pupil Pilocarpine Cycloplegic - paralyzes the ciliary muscle Cyclogyl Tropicamide Ocular Pharmacology Routes of delivery Solutions Suspensions Ointments Courtesy: National Eye Institute, National Institutes of Health What’s Next? Today Lightly review the material Get a good night’s sleep Arrive a little early to test Future Look for details about the CPOT test - begin studying the Self-Study Course for Paraoptometric Assistants and Technicians Request a copy of the Practical Examination Video from the CPC Questions? Study Materials The AOA Paraoptometric Section (PS) may assist with questions concerning PS Membership, staff development, and study materials 800-365-2219 ext. 4108 Certification The Commission on Paraoptometric Certification may assist with questions concerning examinations, certification, and re-certification 800-365-2219 ext. 4210