Airway
advertisement

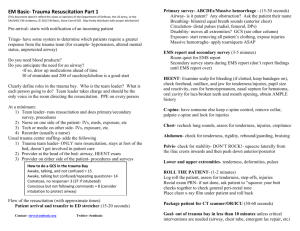
Trauma Resuscitation Shelley Atkinson RN, MSN, ANP-BC, ACNP- BC Objectives • Identify the correct sequence of priorities for assessment of a multiple injury trauma patient. • Identify the principles outlined in the primary and secondary evaluation surveys to the assessment of a multiple injury patient. • Identify guidelines and techniques in the initial resuscitative and definitive-care phases of treatment of a multiple injury patient. Injury Statistics • Leading cause of death for ages 1-44 • $ 500 billion dollar annual cost • Estimated 20-50 million injuries occur per year (40 % of emergency room visits) • Leading causes of trauma are motor vehicle crashes, falls, and assaults Trimodal Death Distribution • Death due to injury occurs in one of three periods or peaks • Care provided during each of these periods impacts patient outcomes Trimodal Death Distribution • First peak – occurs within seconds to minutes of injury • Second peak – occurs within minutes to several hours following injury • Third peak – occurs several days to weeks after initial injury Advanced Trauma Life Support (ATLS) Assess the patient’s condition rapidly and accurately Resuscitate and stabilize the patient according priority Determine if patient’s needs exceed a facility’s resources/or doctor’s capabilities Arrange for transfer (what, where, when, who, and how) ATLS • Assure that optimum care is provided and level of care does not deteriorate at any point during evaluation, resuscitation, or transfer process What is a Level One Trauma Center? A hospital equipped to provide comprehensive emergency medical services to patients suffering traumatic injuries. Level One Criteria Airway/Breathing • Unstable airway/unsecure airway • Patients with severe maxillofacial injuries • Patients requiring immediate airway intervention • Facial burns or burns with significant suspicion of inhalation injury • Moderate to severe Respiratory distress • Sub Q air in face, neck, or chest Level One Criteria Circulation • Systolic BP < 90mmHg or HR > 120 • Witnessed cardiac arrest from trauma • Uncontrolled/Arterial Bleeding with shock • Spinal/Neurogenic Shock Level One Criteria CNS • GCS ≤ 8 • Head injury with LOC > 5 min • Known spinal cord injury • Neurologic deficits with suspected spinal cord injury (any level) Level One Criteria Chest/Abdomen/Pelvis • Chest/Abdominal/Pelvic Injury with shock • Chest wall injury – Flail chest – Sucking chest wound – Subcutaneous air • Pregnancy ≥ 24 weeks with significant mechanism of injury Level One Criteria Extremities • Multiple long bone fractures with shock • Mangled Extremity or Amputation – above wrist/ankle Level One Criteria Mechanism of Injury • Penetrating trauma to the head, face, torso (chest, abdomen, buttocks, back) • Ejection from vehicle • Fall from 20 or more feet with presence of other Level I criteria • Electrocution/Electrical Injury with entry/exit wounds Level One Criteria Mechanism of Injury • Burns > 20% TBSA or burns combined with any other injury • Massive crush injury Pre-hospital care Initial Assessment Primary survey and resuscitation of vital functions are done simultaneously. A team approach Primary Survey ABCDEs • • • • • Airway with cervical spine protection Breathing Circulation with hemorrhage control Disability: Neurologic status Exposure/Environment What is the number one priority during the initial assessment of a trauma patient? A. Airway B. Airway C. Airway D. All of the above Airway Obstruction Recognition Look Listen • • • • • • Normal speech- no obstruction • Noisy breathing – obstruction • Gurgle • Stridor • Hoarseness Agitation/Obtunded Decreased air movement Retraction Deformity Airway debris Inadequate Breathing Look Listen • Cyanosis • “I can’t breathe” • Change in Mental Status • “I am dying” • Chest asymmetry • Stridor, wheezes • Tachypnea • Decreased or absent breath sounds • Neck vein distention • Paralysis Feel • Sub Q emphysema/chest wall crepitus • Tracheal deviation Which way for the Airway? Rapid Sequence Intubation • Be prepared to perform a surgical airway in the event that airway control is lost • Pre-oxygenate patient with 100% oxygen • Administer analgesic / sedative (IV) if feasible • Apply pressure over cricoid cartilage – Debatable • Administer a paralytic IV • Perform chin lift/jaw thrust Rapid Sequence Intubation • After the patient relaxes, intubate orotracheally • Inflate cuff and confirm placement – auscultate and determine CO2 in exhaled air • Release cricoid pressure • Ventilate • CXR Adjuncts to Primary Survey • • • • ECG CO2 detector Pulse oximetry Vital Signs Primary Survey Circulation with Hemorrhage Control • Control hemorrhage • Activate trauma (Massive Transfusion Protocol) – 6U pRBC, 4U FFP, 1 Platelets – MD activation only • Judicious use of crystalloid 6 areas potential blood loss • • • • • • • Chest Abdomen Retroperitoneum Pelvis Long bones / Soft tissue Scalp …the ground Trauma • Majority deaths occur in 1st few hours after injury • Hemorrhage largest % deaths within 1st hour • Hemorrhagic shock and exsanguination – 80% deaths in OR – 50% deaths 1st 24 hrs after injury • Very few hemorrhage deaths after 1st 24 hours • Only CNS injury more lethal Special Considerations In Diagnosis and Treatment of Shock • • • • • • Age Athletes Pregnancy Medications Hypothermia Pacemakers Vascular Access • 2 large-caliber, peripheral IVs • Central access – femoral – jugular – subclavian • Intraosseous • Obtain blood for crossmatch • Trauma panel – CBC, BMP, coags Hemorrhagic Shock Class I EBL <750 Class II 750-1500 Class III Class IV 1500-2000 >2000 HR <100 >100 >120 >140 BP NL NL LOW LOW UO >30 20 - 30 5 - 15 MIN ACS-COT 1993 Direct Effects of Hemorrhage • Class I – (up to 15% blood volume loss) Exemplified by the patient that has donated one unit of blood • Class II – (15% - 30% blood volume loss) Uncomplicated hemorrhage for which crystalloid fluid resuscitation is required Direct Effects of Hemorrhage • Class III – (30% - 40% blood volume loss) Complicated hemorrhagic state in which at least crystalloid infusion is required and perhaps also blood replacement • Class IV – (more than 40%) Considered a pre-terminal event, and unless very aggressive measures are taken, the patient will die within minutes Fluid Resuscitation • Balance organ perfusion with risk of re-bleeding – may reverse vasoconstriction of injured vessel – Dislodge early clot – Dilute coagulation factors – Cool patient – Induce visceral swelling Too much fluid? Adequacy of Resuscitation Clinical Variables • • • • • • Mentation Pulse, pulse pressure, BP Urine output Clot formation Temperature Lactate/base deficit Primary Survey - Disability Neurologic Evaluation • Baseline neurologic evaluation • GCS scoring • Pupillary response **Observe for neurologic deterioration Head Trauma • Severe CHI (GCS < 9) vulnerable to secondary brain injury • Hypotension doubles mortality • Hypoxia and hypotension increases mortality by 75% • Normovolemia goal (dehydration harmful) • Hypertonic saline or Osmotic Agent (mannitol) Head Trauma • Hyperventilation used cautiously – only used if patient rapidly deteriorates • PCO2 no lower than 30-35 • Prolonged hyperventilation can produce cerebral ischemia and secondary brain injury • Mannitol useful – after adequate volume resuscitation Spinal Cord Injury • Neurogenic Shock – Consider hemorrhage first… • Maintain spine immobilization • Fluid or no fluid? • Vasopressors Septic Shock • Uncommon immediately after injury • May occur several hours after injury (especially if transfer to emergent facility delayed) • May occur in penetrating abdominal injuries – contamination of intestinal contents into peritoneal cavity Primary Survey Exposure/Environmental Control • Completely undress the patient • Prevent hypothermia Deadly Triad • Hypothermia • Acidosis • Coagulopathy Hypothermia (HT) • • • • Frequent in trauma/massive transfusions Trauma-related HT considered poor prognostic sign Mortality directly to degree and duration Inhibits coagulation factor synthesis, prolongs PT and PTT • Severely affects platelet count and function • Attenuates vital CV compensatory responses, predisposes to arrhythmias Re-warming • Aggressive therapy associated with significant decrease in: – blood loss – fluid requirements – organ failure – LOS in ICU – mortality rate Secondary Survey • Begins after ABCDE is completed • Resuscitative efforts underway • Each region of the body is completely examined Trauma imaging • Chest x-ray • Pelvis x-ray • FAST – focused assessment sonography in trauma • DPL (center-dependent) – diagnostic peritoneal lavage • CT scan – Traumagram Adjuncts Secondary Survey • Foley • NGT • ABG/lactate – If actively resuscitating Primary Goal of Initial Operation for a Trauma Patient Damage Control • Hemorrhage Control • Contamination Why Trauma NPs?? High acuity, high volume with seasonal surges. Transition area of 17 beds experiencing delayed throughput Hypothesized that by adding experienced Trauma NPs, we could improve throughput and quality in care. 1 year, compared with 2 years prior Results: • Increased volume of cases by 14.3% • 1.0 reduction in ALOS for entire trauma service • 27.8 million reduction in hospital charges. • Increased direct discharges by 21%. MD/RNs found the addition of ACNPs beneficial, improved patient care, improved workflow, improved communication and throughput. References • Acute Trauma Life Support Course – Retrieved from American College of Surgeons Website http://www.facs.org/trauma/atls/information.html on July 1, 2012. • Guillamondegui, Oscar MD, MPH, FACS, Associate Professor of Surgery, Medical Director, Trauma ICU, Director of Trauma Education, Vanderbilt University Medical Center. • Atkinson, S., Collins, N., Martin, M., Morton, M., Marshall, K. (2012) Outcomes of Adding ACNPs to a Level One Trauma Service with the Goal of Decreased Length of Stay and Improved Patient, Physician and Nursing Satisfaction: A pilot study.