CDRH Seminar - University of Pennsylvania School of Medicine

The Pragmatic Clinical Trial in a Learning Healthcare System
University of Pennsylvania
8th Annual Conference on
Statistical Issues in Clinical Trials
Roger J. Lewis, MD, PhD
Department of Emergency Medicine
Harbor-UCLA Medical Center
David Geffen School of Medicine at UCLA
Los Angeles Biomedical Research Institute
Berry Consultants, LLC
1
Financial Disclosures
• Berry Consultants, LLC
– Multiple clients
• Support from
– National Institutes of Health/NINDS
– Venaxis, Inc.
• Prior support from
– Food and Drug Administration
• Octapharma AG
2
Intellectual Disclosure
• This presentation includes the intellectual work of multiple colleagues
– Derek C. Angus, MD, MPH
– Don A. Berry, PhD
– Scott M. Berry, PhD
– Jean-Daniel Chiche, MD
– Jason Connor, PhD
– John Marshall, MD
– Will Meurer, MD, MS
– Alistair Nichol, MD
– Steve Webb, MD
– Leadership from the European PREPARE Consortium
(Herman Goossens, Marc Bonten and others)
– And others!
3
The Learning Healthcare System
“The nation needs a healthcare system that learns.” (IOM 2007)
• Adaptation to the pace of change
• New clinical research paradigm
• Universal electronic health records and clinical decision support systems
• Narrowing the research-practice divide
4
The 3048 Meter View of a
Pragmatic Trial in a LHS
Best standard care
Randomized, adaptive, treatment allocation
Heterogeneous patient population
EHR Data
Ethical integrity
(consent, privacy)
Selected
Outcome Data
Adaptive algorithm with considerations of HTE
5
Key Components
• Healthcare systems with informatics systems, leadership, and commitment to learn
– Veterans Health Administration
– European PREPARE Consortium
– PCORI National Patient-Centered Clinical Research
Network (PCORnet)
• Multiple treatment domains and factors to be investigated
• Flexible, adaptive trial algorithm for assigning treatments, evaluating effects, and drawing conclusions (“platform trial”)
6
Motivation for Adaptive Trials
• When designing a trial there is substantial uncertainty regarding how best to treat subjects in the experimental arm (e.g., uncertainty in optimal dose, best duration, target population)
• This creates uncertainty in the optimal trial design
• Traditionally, all key trial parameters must be defined and held constant during execution
• This leads to increased risk of negative or failed trials, even if a treatment is inherently effective
7
Motivation for Adaptive Trials
• Once patients are enrolled and their outcomes known, information accumulates that reduces uncertainty regarding optimal treatment approaches
• Adaptive clinical trials are designed to take advantage of this accumulating information, by allowing modification to key trial parameters in response to accumulating information and according to predefined rules
8
JAMA 2006;296:1955-1957.
9
Adaptation: Definition
• Making planned, well-defined changes in key clinical trial design parameters, during trial execution based on data from that trial, to achieve goals of validity, scientific efficiency, and safety
– Planned: Possible adaptations defined a priori
– Well-defined: Criteria for adapting defined
– Key parameters: Not minor inclusion or exclusion criteria, routine amendments, etc.
– Validity: Reliable statistical inference
10
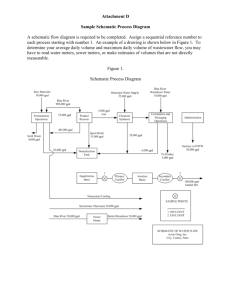
The Adaptive Process
Begin Data Collection with Initial
Allocation and Sampling Rules
Analyze
Available Data
Continue Data
Collection
Revise Allocation and Sampling Rules per Adaptive Algorithm
Stopping
Rule Met?
No Yes
Stop Trial or
Begin Next
Phase in
Seamless
Design
11
Why Do Adaptive Clinical Trials?
• Usual Reasons
– To avoid getting the wrong answer!
– To avoid taking too long to draw the right conclusion
• In the setting of a learning healthcare system
– To learn about effectiveness, and apply what we learn, simultaneously
– To continually improve patient outcomes
12
Selected Adaptive Strategies
• Frequent interim analyses
• Response-adaptive randomization to efficiently address one or more trial goals
• Explicit decision rules based on Bayesian predictive probabilities at each interim analysis
• Enrichment designs
• Extensive simulations of trial performance
13
14
Response-adaptive Randomization
• Response-adaptive randomization to improve important trial characteristics
• May be used to address one or more of:
– To improve subject outcomes by preferentially randomizing patients to the better performing arm
– To improve the efficiency of estimation by preferentially assigning patients to doses in a manner that increases statistical efficiency
– To improve the efficiency in addressing multiple hypotheses by randomizing patients in a way that emphasizes sequential goals
– Includes arm dropping
15
Example Learning Strategy
Standard
Low Dose
Med Dose
High Dose
Start
“Burn in” RAR: Dose
RAR:
Confirmation
Treatment
Rec.
300 400 500 600 700 800 900 1000 1100
Time
1500
16
17
Platform Trial
• An experimental infrastructure to evaluate multiple treatments, often for a group of diseases, and intended to function continually and be productive beyond the evaluation of any individual treatment
– Designed around a group of related diseases rather than a single treatment
– Dynamic list of available treatments, assigned with response-adaptive randomization
– Preferred treatments may depend on health system, patient, or disease-level characteristics
18
JAMA. Published online March 23, 2015. doi:10.1001/jama.2015.2316
19
From: The Platform Trial: An Efficient Strategy for Evaluating Multiple Treatments
JAMA. Published online March 23, 2015. doi:10.1001/jama.2015.2316
Table Title:
General Characteristics of Traditional and Platform Trials a
Date of download: 3/24/2015
Copyright © 2015 American Medical
Association. All rights reserved.
20
Initial Usual Care
1 st Generation “A”
2 nd Generation “A”
Drug B
“A + B”
Platform Trial
Time
21
Platform Trial
Initial Usual Care
1 st Generation “A”
2 nd Generation “A”
Drug B
“A + B” Subtype A
Initial Usual Care
1 st Generation “A”
2 nd Generation “A”
Drug B
Subtype B
Time
22
Platform Trial Terminology
• Domain
– A domain of treatment
– Ex: ventilator management
• Factor
– One particular approach within a domain
– Ex: 6cc/kg tidal volume ventilation
• Regimen
– The assigned collection of factors from multiple domains
23
Framing the Possible
Conclusions of a Platform Trial
• The number of regimens can be very large
– Very difficult to show an individual regimen has a very high probability of being best within a patient subgroup
• May draw a conclusion when
– There is a very high (or low) probability that a given factor is included in the best regimen(s)
– This allows you to reduce the complexity of the problem over time and improve the treatment and outcomes of patients
24
Randomized Embedded, Multifactorial,
Adaptive Platform (REMAP) trial
• Randomized
• Embedded
• Multifactorial
• Adaptive
• Platform
Thanks to Derek C. Angus, MD, MPH, University of
Pittsburgh Medical Center, for “REMAP”
25
Examples
27
28
Embedding the Clinical Trial
29
Research Processes
30
Response-adaptive Randomization
31
The PREPARE Consortium
• P latform fo R E uropean P reparedness
A gainst ( R e)emerging E pidemics
– 25 million euro FP7 strategic award
• Work Package #5 – ‘PREPARE CAP’
– An adaptive trial platform to determine best care for severe acute respiratory failure of presumed infectious origin
• Endemic - severe CAP
• Epidemic – severe respiratory viral illness (e.g.,
H1N1)
32
The PREPARE Consortium
33
Scope of PREPARE CAP
• Simultaneously considers
– Anti-infective strategies (i.e., antibiotic choice)
– Host response modulation (i.e., steroids)
– Organ support strategies (i.e., mechanical ventilation)
• Design stratifies by different subgroups
– Shock or not
– Severe vs. moderate hypoxemia
• With five “yes/no” strata (treatments and subgroups) there are 2 5 = 32 “cells”
• Additional complexity
– Add or drop factors by region, country, patient subgroup, and season (e.g., “influenza flu season”)
34
Embedding the Trial into Routine Care
• For EVERY patient who presents with severe CAP, clinical team calls IVRS for the patient’s unique order set
35
Starting Conditions/Burn In
#4
#5
#6
#7
Regimen Anti-infective
#1 Quinolone
#2
#3
Quinolone
Quinolone
Quinolone
Combination Rx
Combination Rx
Combination Rx
Immunomodulation Ventilation strategy
Hydrocortisone 6cc/kg
Hydrocortisone
None
4cc/kg
6cc/kg
None
Hydrocortisone
Hydrocortisone
None
4cc/kg
6cc/kg
4cc/kg
6cc/kg
#8 Combination Rx None 4cc/kg
• Equal randomization for first 200 patients (burn-in)
• RAR driven by a full factor statistical model
• Factor for each single factor
• Interactions of two factors
• 3-way interactions
• Priors expecting low interactions, allows for learning
36
Trial Schematic
Domain 1 Domain 2 Domain 3
37
Trial Schematic
Domain 1 Domain 2 Domain 3
Data
Data
Base
Statistical
Model
38
Trial Schematic
Domain 1 Domain 2 Domain 3
Data
Data
Base
IVRS
Statistical
Model
39
Trial Schematic
Domain 1 Domain 2 Domain 3
Data
Data
Base
IVRS
Statistical
Model
40
Trial Schematic: Adding a Factor
Domain 1 Domain 2 Domain 3
Data
Data
Base
IVRS
Statistical
Model
41
Trial Schematic: Adding a Domain
Domain 1 Domain 2 Domain 3 Domain 4
Data
Data
Base
IVRS
Statistical
Model
42
Trial Schematic: Selecting a Factor
Domain 1 Domain 2 Domain 3
Data
Data
Base
IVRS
Statistical
Model
43
Trial Schematic
Domain 1 Domain 2 Domain 3
Data
Data
Base
IVRS
Statistical
Model
44
Trial Schematic
Domain 1 Domain 2 Domain 3
Data
Data
Base
IVRS
Statistical
Model
45
Trial Schematic
Domain 1 Domain 2 Domain 3
Data
Data
Base
IVRS
Statistical
Model
46
Trial Simulation
Virtual
Patients
Assumed
“Reality”
Execution
Variables
“Observe”
Single Trials
Operating
Characteristics
(error rates & power)
48
49
Opportunity
51
Conclusions
• Adaptive trial designs can be used to create a seamless process in which new evidence about effectiveness is immediately used to improve patient care
• A platform trial can extend this process beyond a single treatment or few treatments
• Current work is focused on embedding this approach into the health care infrastructure
• Patients will benefit if we merge clinical trials and decision support into a single, continuous process
52