Evidence-Based Perspectives on Contemporary Approaches to Pain
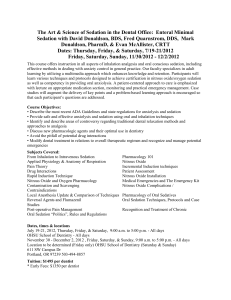
advertisement

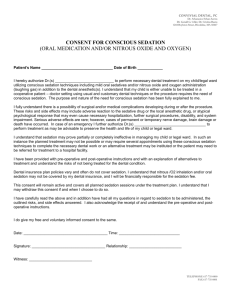
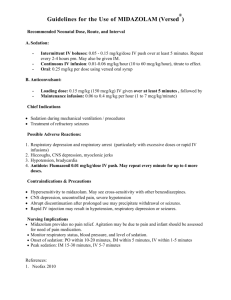
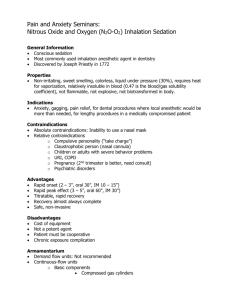
Evidence-Based Perspectives on Pain and Anxiety Control in Dentistry Dr. Arthur Jeske Arthur.H.Jeske@uth.tmc.edu Utah Dental Association, 2/15/08 Today’s Course Topics… • • • • • • • Fundamentals of anxiety management Current guidelines (conscious/minimal sedation) Enteral (oral) sedatives Nitrous oxide/oxygen inhalation sedation Basic emergency drugs Contemporary perspectives on local anesthetics Contemporary perspectives on oral analgesics Disclaimers The opinions expressed in this course are those of the speaker and not necessarily those of the Utah Dental Association. The opinions expressed in this course should not be construed as advice for the care of specific patients. The drugs and techniques contained in this course must be based on the clinical judgment of the individual practitioner. American Dental Association GUIDELINES FOR TEACHING PAIN CONTROL AND SEDATION TO DENTISTS AND DENTAL STUDENTS As adopted by the October 2007 ADA House of Delegates www.ada.org Minimal Sedation A minimally depressed level of consciousness produced by a pharmacologic method that retains the patient’s ability to independently and continuously maintain an airway and respond normally to tactile stimulation and verbal command. Although congnitive function may be modestly impaired, ventilatory and cardiovascular functions are unaffected. Other ADA Guideline Excerpts • Nitrous oxide may be used with “a single enteral drug” • Initial oral dose is “no more than MRD for unmonitored home use” • Combination of nitrous and oral agents “may produce minimal, moderate or deep sedation or general anesthesia” • “Supplemental dosing is a single additional dose” for “prolonged procedures” and “should not exceed ½ the initial dose” (not until the “clinical half-life of the initial dose has passed”) • “total aggregate dose must not exceed 1.5 MRD” Conscious Sedation http://www.ncbi.nih.gov/pubmed/1 7187034?ordinalpos Guidelines Balancing Efficacy and Safety in the Use of Oral Sedation in Dental Outpatients Dionne RA et al. JADA 2006;137:502-13 http://jada.ada.org “ENTERAL ADMINISTRATION OF Benzodiazepines safe but poorly documented in the office setting” Conscious sedation, including incremental triazolam, necessitates…monitoring, documentation, facilities equipment and personnel as described in ADA and AAPD guidelines” Consensus (Dionne et al., 2006) • Oral sedative = wide margin of safety in ADULTS • Most serious events = respiratory depression • State regulation required to ensure safety • More research needed for “incremental dosing” techniques • 0.25 mg triazolam X 2 >>0.5 mg single dose Sedation Modifications. How Will the Proposed Guidelines Affect Your Practice? Lynch, K. AGD Impact July 2007;48-54 AGD White Paper at: http://www.agd.org/members_only/advocacy/priority_issues/ConsciousSedation.doc Here’s What You Thought (AGD Impact July 2007) • • • • • • 74% use N2O 53% combine nitrous oxide and a BZ 67% have patient take sedative at home 43% administer sedative in the office 90% never had an untoward reaction 48% totally understand the difference between minimal and moderate sedtion Conscious Sedation Guidance Coulthard, P. J. Evid. Based Dent., 2006;7(4):90-91 www.scottishdental.org/cep/guidance/dentalsedation.htm The Scottish Dental Clinical Effectiveness Programme Coulthard, 2006 • 48 recommendations total • To be updated 2008 • Included general systematic reviews (Cochrane Library) and specific studies (Medline, Embase & Cochrane Library) Recommendations: Referral • Discuss alternative methods of anxiety management with patient • Ensure that definition of “conscious sedation” is met Recommendations: Assessment and Record Keeping • Discuss all aspects of sedation procedure with patient • Provide written instructions • Obtain informed consent • Maintain and update patient records Recommendations: Environment and Facilities • Ensure that environment is safe • Correct equipment and drugs • Emergency drugs and equipment immediately available Recommendations: Training • All members of team are correctly trained • Training includes monitoring techniques and emergency interventions • “For oral and transmucosal” sedation, “sedationist” trained in other titratable sedation techniques and venipuncture • Teams should provide sedation for patient groups they are experienced in treating Recommendations: Techniques • “Titrated dose of nitrous oxide” • Oral, transmucosal and i.v. “require” pulse oximetry and BP monitoring Recommendations: Aftercare • Monitor patients during recovery • Dismiss patient into care of a responsible adult (who also has written instructions) • Nitrous oxide sedation “might not” required adult escort during recovery Recommendations: Further Research Required For… • • • • • • Fasting before conscious sedation Pediatric conscious sedation Drug combinations Conscious sedation methods Cognitive & behavioural effects of sedation Interaction of pharmacological and nonpharmacologic anxiety management Utah Dentist and Dental Hygienist Practice Act Rules R156-69-601 Scope of Practice—Anesthesia and Analgesia Permit Conscious Sedation for Dental Anxiety (Protocol) Cochrane Database of Systematic Reviews 2007, Issue 1 Primary Outcomes To Be Assessed • Changes in anxiety scores • Reliability and validity of anxiety measurement instruments/scales Anxiety An internal, emotional response; a specific unpleasurable sense state of tension which indicates the presence of some danger ANTICIPATED Fear: A short-lived feeling that something terrible is going to happen; accompanied by physiologic changes (increased HR, perspiration) and overt behavior signs (jitteriness, shaking) “Fight or Flight” IMMEDIATE THREAT Conscious Sedation • Drugs and/or techniques used should carry a margin of safety wide enough to render loss of consciousness UNLIKELY • Patients who are SLEEPING and whose only reponse to stimuli is reflex withdrawal would NOT be considered to be in a state of conscious sedation “Bottom-Line” Requirements for Minimal/Conscious Sedation • Comfort • Consciousness • Cooperation Adult Preferences for Sedation or General Anesthesia (Survey of 1,101 Canadian Adults) • • • • • • Routine cleaning: 7.2% Fillings/crowns: 18% Tooth extraction: 47% Endodontic procedure: 55% Periodontal surgery: 68% From Chanpong, Haas & Locker, Anesth. Prog. 2005;52(1):3-11 • http://apt.allenpress.com/perlserv Clinical Considerations • Physician consultation recommended for ASA III & IV patients • One member of assistant staff should be present (in addition to dentist) • Direct supervision • Monitoring required for oxygenation, ventilation and circulation • Time-oriented anesthetic record Advantages of Oral Sedation • • • • Universal acceptability Ease of administration Low co$t Incidence of adverse reactions less than some other techniques • No needles, syringes or special techniques • Various drugs, dosage forms available • Allergic reactions less severe than seen in parenteral administration Disadvantages of Oral Sedation • • • • • • • Reliance on patient compliance Prolonged, variable onset of action Unreliable absorption of drug from G.I. tract INABILITY TO TITRATE: WHAT??? Prolonged duration of action Ineffective in anxiety levels > mild Adverse interactions of sedative drugs Idiosyncrasy An unexpected, unpredictable adverse or undesirable drug action Indications for Oral Sedation • Mild to moderate dental anxiety • To assist with restful sleep on night before dental appointment Contraindications to Oral Sedation • • • • • Severe dental anxiety & fear High probability of adverse drug interaction Poor past experience with oral sedation Allergy to drug being used Other drug contraindications (pregnancy, glaucoma, etc.) • Need for rapid onset and/or rapid recovery What causes the sudden death of a patient? • Respiratory arrest with or without airway obstruction • Cellular hypoxia without respiratory depression (CN, CO) • Severe hypotension (hypovolemic, etc.) • Lethal cardiac dysrhythmias • Post-seizure complications (pulmonary aspiration, hypoxia, brain damage) • Organ damage (e.g., APAP/liver) • Behavior aberrations (motor vehicle accidents) Oral Sedation: “Unfilled Expectations” • Pain control, reduced need for local anesthesia • Control of defiant behavior, mentallychallenged patients • Amnesia • Lack of adverse effects • Consistency from appointment to appointment • “A good night’s sleep” the night before the dental procedure Sedation should NOT be used to control pain and does NOT substitute for good local anesthesia Enteral Sedation Light to mild conscious sedation administered not for analgesic effect, but primarily for behavioral management (drug absorbed through GI tract or oral mucosa) Factors Influencing Oral Drug Absorption • • • • • • • • • Lipid solubility pH of gastric tissues Mucosal surface area Gastric emptying time Dosage form of drug Drug inactivation (“first pass effect”) Presence of food in stomach Bioavailability of drug Genetics Alpha Distribution Phase The phase in which sedative activity is initiated & ended, by entry into and removal from the CNS Beta Elimination Phase The phase in which a sedative drug is inactivated by hepatic metabolism & excretion Margin of Safety The difference between the effective therapeutic dose and the dose that produces severe or lifethreatening adverse effects Reasons NOT to used BZs… • • • • • Allergy Narrow angle glaucoma Chronic BZ ingestion…??? Tricyclic antidepressant therapy…??? Adversely interactive drugs (e.g., azole antifungals/triazolam) Characteristics of Benzodiazepines • Facilitate binding of GABA (endogenous inhibitory transmitter) • More favorable therapeutic index than older agents • Can produce anterograde amnesia • Agents differ in onset, duration & metabolism • Agents differ in regard to sedation vs. hypnosis Boxed Warning: BZs “sleep driving” (with no memory) “severe allergic reactions” http://www.fda.gov/bbs/topics/NEWS/2007/NEW01587.html Pharmacokinetics and Clinical Effects of Multidose Sublingual Triazolam in Healthy Volunteers. Jackson DL et al. J. Clin. Psychopharmacol. 2006;26(1):4-8 • 10 human volunteers • 0.25 mg followed by 0.25 mg at 60 mins and 0.25 mg at 90 mins • Evaluated by observed, bispectral index and plasma triazolam levels • 8 subjects met criteria for deep sedation or general anesthesia at later time point Advantages of Benzodiazepines • • • • • Specificity of effect Well absorbed by the oral route High margin of safety/therapeutic index Effective as single agents Specific reversal agent available (flumazenil) Classification of Benzodiazepines • • • • • • Alprazolam: antianxiety Diazepam: antianxiety Lorazepam: antianxiety/sedative-hypnotic Midazolam: sedative/hypnotic Oxazepam: antianxiety Triazolam: sedative/hypnotic Diazepam (VALIUM) • Usual dose range: 2 - 20 mg, 1 h before appointment (adults) • Onset: 1 hr (peak levels in 2 hrs) • Duration: 1 - 3 hrs • Contraindications: allergy, narrow-angle & untreated open-angle glaucoma • Precautions: sedation intensified by several CYP inhibitors (3A4, 2C19) Diazepam • Active metabolites? Yes • Pregnancy category D • Availability: 2-, 5& 10-mg tabs, 5 mg/ml liquid, rectal gel 5 mg/ml Lorazepam (ATIVAN) • Usual dose range: 2 - 4 mg 1 hr before appointment (adults) • Onset: 1 hr (peak levels in 2 hrs) • Duration: 2 - 4 hrs (use for longer procedures) • Contraindications: allergy, narrow-angle glaucoma • Precautions: greater likelihood of excessive sedation than with other agents, do not use in cases of depressive disorder/psychosis Lorazepam • Active metabolites? No • Pregnancy category D • Availability: 0.5-, 1 and 2-mg tabs Oxazepam (SERAX) • Usual dose range: 10 – 30 mg, 1 hr before appointment (adults) • Onset: 1 hr (peak levels in 1 – 4 hrs) • Duration: 2 – 4 hrs • Contraindications: allergy • Precautions: same as for other agents • Active metabolites? No • Pregancy Oxazepam category D • Availability: 10-, 15- & 30-mg caps, 15-mg tabs Triazolam (HALCION) • Usual dose range: 0.25 – 0.5 mg, 1 hr before appointment (adults) • Onset: 1.3 hrs (peak levels in 0.5 – 4 hrs) • Duration: 1 hr • Contraindications: allergy, pregnancy, do not administer with potent CYP 3A4 inhibitors (e.g., azole antifungals) • Precautions: anterograde amnesia, excessive sedation (especially elderly) Triazolam • Active metabolites? No • Pregnancy category X • Availability: 0.125- & 0.25-mg tabs Triazolam Doses Short-term management of insomnia 0.25mg PO hs Max: 0.5 mg PO hs; Alternative: 0.125 mg PO hs if elderly, hepatic impairment Triazolam Onset: 1 hr. Peak effect: 1.3 hrs. Duration: 2 – 3 hrs. Alprazolam (XANAX) • Usual dose range: 0.25 – 1 mg 1 hr before appointment (adults) • Onset: 1 hr (peak levels in 1 – 2 hrs) • Duration: 1 – 2 hrs • Contraindications: allergy, narrow- and untreated open-angle glaucoma, potent CYP 3A4 inhibitors (e.g., azole antifungals) • Precautions: sedation intensified by CYP 3A4 inhibitors, produces little or no amnesia or somnolence Alprazolam • Active metabolites? No • Pregnancy category D • Availability: 0.25-, 0.5, 1- & 2-mg tabs, 0.5- and 1 mg/ml liquid Midazolam • ALL BRAND NAME FORMS (VERSED) DISCONTINUED BY ROCHE MAY, 2002 • Now available from Ranbaxy Pharmaceuticals as 2 mg/ml cherry syrup (Princeton, NJ) • Usual dosage range: 0.25 – 0.5 mg/kg single dose up to a total maximum of 20 mg (children) • Onset: 10 – 20 min • Duration: 30 – 60 min • Contraindications: allergy, narrow-angle glaucoma Midazolam • Precautions: may cause intense CNS/respiratory depression, use with caution with potent CYP 3A4 inhibitors (e.g., azole antifungals) NOT TO BE ADMINISTERED AT PATIENT’S HOME • Active metabolites? No • Pregnancy category D • Availability: 2 mg/ml syrup Oral BZ Biovailability & Half-lives • • • • • • Diazepam: 100%, 43 ± 13 hrs Oxazepam: 97%, 8 ± 2.4 hrs Lorazepam: 90%, 12 ± hrs Alprazolam: 88%, 12 ± 2 hrs Triazolam: 44%, 2.9 ± 1 hrs Midazolam: 44%, 1.9 ± 0.6 hrs Non-BZ BZ Receptor Agonists • Eszopiclone (LUNESTA) • Zaleplon (SONATA) • Zolpidem (AMBIEN) Melatonin Receptor Agonist: Ramelteon (ROZEREM) • • • • • • • MT1 & MT2 receptor agonist Simulates melatonin (“circadian rhythm) 8 mg Rapid onset, Tmax = 45 min Low bioavailability, 70% protein-bound CYP 1A2 (fluvoxamine caution) Not controlled substance Zolpidem (AMBIEN) • Usual dose range: 5 – 10 mg, 1/2 hr before appointment • Onset: 0.5-1 hr (peak levels in 1.6 hrs)(use when rapid onset needed) • Duration: 2 – 3 hrs • Contraindications: allergy • Precautions: reduce dosage in elderly • Active metabolites? No Zolpidem • Pregnancy category B • Availability: 5- and 10-mg tabs Hydroxyzine (ATARAX, VISTARIL) • Usual dose range: 50 – 100 mg, 1 hr before appointment (adults), 1.1 – 2.2 mg/kg (children) • Onset: 30 min (peak effect 2 hrs) • Duration: 3 – 4 hrs • Contraindications: allergy • Precautions: same as for benzodiazepines, more anticholinergic actions (glaucoma, respiratory disease) • Active metabolites? No • Pregnancy category D • Availability: 10-, 25-, 50- & 100-mg tabs; 10mg/5 ml syrup (ATARAX); 25-, 50-, & 100-mg caps and 25mg/5 ml oral suspension (VISTARIL) • Non-controlled substance Hydroxyzine Promethazine (PHENERGAN) • Usual dose range: 25 – 50 mg, 1 hr before appointment (adults), 2.2 mg/kg (children, when used as SOLE sedative agent) • Onset: 1 hr (peak effect 2 hrs) • Duration: 3 – 4 hrs (may be up to 12 hrs) • Contraindications: allergy, conditions worsened by anticholinergic actions • Precautions: same as for other sedatives, also seizure disorders Promethazine • Active metabolites? No • Pregnancy category C • Availability: 12.5-, 25- & 50-mg tabs; 6.25 mg/5 ml syrup; 25 mg/5 ml syrup fortis • Not a controlled substance Agents NOT Recommended (Adults) • Alcohol • Chloral hydrate • Opioids • Multi-Drug Cocktails Nitrous Oxide Advantages of Nitrous Oxide • • • • • • Rapid onset (almost equal to that of iv) Titratable (up AND down) Depth of sedation readily altered Flexible duration of action Rapid recovery from sedation Safe Advantages of Nitrous Oxide • • • • No injection required Very few side effects No adverse effects on vital organs May substitute for local anesthesia in selected circumstances (e.g., soft tissue procedures) Disadvantages of Nitrous Oxide • Initial co$t of cumbersome equipment is high • Continuing co$ts of gases high • Equipment takes up operatory space • Lack of potency • Requires constant patient cooperation • Chronic exposure of office personnel Indications for Inhalation Sedation • Mild to moderate dental anxiety • Medically compromised patients • Gagging (impressions, radiographs) Relative Contraindications to Inhalation Sedation • • • • • • Severe dental anxiety & fear Compulsive personalities Poor past experience with oral sedation Claustrophobia Pregnancy URI, COPD Concentration Effect The higher the concentration of inhaled gas, the more rapidly the blood level of the gas increases Diffusion Hypoxia (?) When the flow of nitrous oxide is stopped, nitrous oxide rapidly leaves the blood and dilutes the oxygen in the alveoli of lungs Prevention of Diffusion Hypoxia Administer 100% oxygen for 3 to 5 minutes at the termination of the sedation procedure CNS Effects of Nitrous Oxide • All senses are slightly depressed or altered (perioral numbness, etc.) • Amnesia does NOT occur • Mild depression of cerebral cortex • Produces mild sedation, analgesia • Lacks direct respiratory depression Nitrous Oxide Does NOT... • Obtund sharp pain impulses • Substitute for good local anesthesia • Sedate agitated or extremely anxious patients • Produce loss of consciousness when used correctly Why Nitrous Oxide is Associated with Nausea • Not titrated • All patients are given “fixed” concentrations (usually 50%) • Signs and symptoms of impending nausea and vomiting are not recognized • Patients are not given appropriate pretreatment instructions Other Effects of Nitrous Oxide • Cardiovascular: no clinically significant effects at recommended concentrations • Cutaneous vasodilation (flush, warmth) • Respiratory: no clinically significant depression at recommended concentrations • G.I. Tract: no effects liver) Other Effects of Nitrous Oxide • Kidneys: no effect • Blood: inhibition of vitamin B-12 metabolism (chronic administration) • Skeletal muscle: no direct effect (relaxation secondary to sedative effect) Contraindications to Nitrous Oxide • Pregnancy (1st trimester) • Upper respiratory tract infection • Nasal hood unacceptable (claustrophobia, allergy, etc.) • Previous “bad experience” • Drug abuse • Chronic environmental exposure Effects of Pathologic Conditions on Inhalation Sedation • Emphysema: decreased total surface area of alveoli • Pneumonia: alveolar walls thickened • Asthma: increased thickness of bronchial secretions • Anemia/Methemoglobinemia: decreased oxygen-carrying capacity of blood Physiologic Equivalents • Total gas flow (LPM) = minute respiratory volume • Excursion of reservoir = tidal volume • Excursions of reservoir bag/min = respiratory rate = respiratory center “firings” • Collapse of reservoir bag with maximum inhalation = inspiratory reserve capacity Complications and Chronic Toxicity Excessive Perspiration • Etiology: peripheral vasodilation • Management: decrease nitrous oxide concentration (5% per min) Expectoration • Etiology: fluid removal problems, diminished patient coordination and cooperation • Management: efficient vacuum operation, rubber dam Behavioral Problems • Etiology: authoritarian patient, excessive nitrous oxide concentrations • Management: decrease nitrous oxide concentration, allow controlled mouth breathing if necessary Nausea • Etiology: excessive length and/or depth of sedation, over-emotional patient, overeating, frequent changes in patient position (esp. pediatrics), frequent changes in nitrous oxide concentration • Management: avoid etiologic factors, premedicate with anti-emetic drug Vomiting • Etiology: same as for nausea • Management: remove nasal hood, turn patient’s head to assistant, change gas mixture to 100% oxygen, apply 100% oxygen for at least 5 min and inform patient Pre-Operative Instructions • 1. Take pre-operative medications (if indicated) • 2. No heavy meals (or no food intake at all) for 4 hrs prior to sedation • 3. Require an escort (if indicated or otherwise required) Chronic Exposure to Nitrous Oxide Mutagenicity of Nitrous Oxide? • Negative in Salmonella microsome assays • Negative in cultured hamster lung fibroblasts • negative in hamster ovarian cells • negative in Drosophila melanogaster • No human studies Carcinogenicity of Nitrous Oxide? • Negative results in mice • Human studies generally negative Teratogenicity of Nitrous Oxide • Definite teratogenicity in rats • male rodents show chromosomal damage (not heritable, significance?) • INCREASED RISK OF SPONTANEOUS ABORTION IN HUMANS • Effects require chronic exposure Dental Office Exposure to Nitrous Oxide Sources of Environmental N2O • Normal gas flow to patients • Patient (talking, “washout” during recovery) • Equipment (leaks) • Air conditioning (recirculation) Office Levels of N2O Depend on • • • • Frequency of use Size of operatory Ventilation of operatory Type of operatory (open vs. closed) Detection of Office N2O • Visual inspection (rubber goods, connections) • Application of soapy water • Air analysis (by outside service company) (infrared spectroscopy) • Monitoring cartridges (Porter “Peace of Mind” cartridges) Minimizing Office N2O » Test for leaks • • • • • Vent waste gases to outside SCAVENGE waste gases Air sweep (oscillating fan) Minimize patient talking Monitor office air quality Effects of Scavenging Systems Nitrous Oxide Levels (ppm) of Breathing Zones in Offices Without & With Scavenging Systems (from • • • • Whitcher et al., JADA, 1977) WITHOUT • WITH General dentist: 775 • General dentist: 21 (+/- 63) (+/-2) Pedodontist: 940 (+/• Pedodontists: 33 (+/92) 4) Oral Surgeon: 1000 • Oral Surgeon: 36 (+/(+/-130) 4) Abuse of Nitrous Oxide Mechanism of Chronic Toxicity • Oxidation of vitamin B-12 (cobalamin; bound co-factor for methionine synthetase and methylmalonyl CoA mutase) • Interferes with folate metabolism and DNA synthesis (decreased thymidine) Clinical Effects of Chronic Toxicity • Bone marrow suppression, anemia, leukopenia • Suppression of neutrophil chemotaxis • Alterations in reproductive cells • Peripheral neuropathy with subacute degeneration of spinal cord • Layzer, R.B. Lancet 2:1227, 1978 Flumazenil (ROMAZICON) • Competes with benzodiazepine for receptor site • Used to reverse CNS depressant effects of overdose and to decrease recovery time • REVERSAL OF RESPIRATORY DEPRESSION NOT PREDICTABLE • Short half-life (readministration often required) Sublingual Injection of Flumazenil? • Average time to reversal with IV route = 2 minutes • Average time to reversal with SL route = 4.33 minutes Flumazenil • Only BZ antagonist available • Can produce agitation, confusion, dizziness & nausea • Can precipitate withdrawal syndrome (chronic BZ use) • Can produce seizures & cardiac arrhythmias in patients taking tricyclic antidepressants • Usual dose: 0.2 mg iv in 15 secs, evaluate in 45 secs. Add additional 0.2 mg if needed • Repeat q. 5 min until recovery or total dose of 1 mg Fundamentals of Emergency Preparation • 1. Training (BLS, ACLS, PALS, TSBDEapproved courses) • 2. Development and implementation of an emergency plan • 3. Purchase and maintenance of emergency equipment and drugs • 4. Periodic mock emergency drills • 5. Training new staff members What Your EMS Personnel Want and NEED! • An accurate medical history of the patient/victim • A concise description of everything that happened • Doctor remains with patient/victim Pre-Emptive Strategies for Dental Office Emergency Preparation and Management • • • • • • Painstakingly detailed health history Medical risk classifcation Avoid potential drug interactions Calculate dental drug dosages carefully Monitor, monitor, monitor!!! IMPLEMENT AN OFFICE EMERGENCYN PLAN A General Paradigm for Assessing and Managing ASA II-IV Patients • Monitor vital signs at every appointment • Know patient’s medications and why they are taking them • Consult the physician to determine degree of disease control, compliance and ability of patient to tolerate dental procedure • Utilize the stress-reduction protocol • Plan for likely emergencies Stress-Reduction Protocol (Medically Compromised Patients) • • • • • • • • 1. Recognize medical risk 2. Consult patient’s physician(s) 3. Pharmacosedation, as indicated 4. Short appointments 5. Morning appointments 6. Excellent intraoperative pain control 7. Minimize waiting room time 8. Excellent post-operative pain control Range of Dental Office Emergencies • • • • • • • • • • Syncope Nausea, vomiting Hyperventilation Acute bronchial constriction/asthma Seizures Acute elevations in BP and HR Acute depressions in BP and HR Hypoglycemia Acute CNS/respiratory depression Swallowing/aspirating foreign object Adverse events associated with outpatient anesthesia in Massachusetts D’eramo EM, Bookless SJ, Howard JB J. Oral Maxillofac. Surg. 2003;61:793800 Methods and Outcomes from D’Eramo et al. • Morbidity data from 157 oral surgeons for year 1999 • Syncope was most common complication (1 in 160 patients receving local anesthesia) Types of Emergency Drugs and Drug Kits • • • • None (or expired) Custom (“homemade”) Pre-assembled, commercial Complete medical emergency “crash carts” • Published lists • ACLS “Core Drugs” Office Emergencies and Emergency Kits ADA Council on Scientific Affairs JADA 2002;133(3):364-365 “Proprietary emergency drug kits are available, but none of these kits is compatible with the needs of all practitioners.” ADA Council on Scientific Affairs 2002 Minimum Emergency Drugs Recommended by ADA CSA • • • • • • • Epinephrine 1:1,000 Injectable antihistamine 100% oxygen with positive-pressure ventilation Nitroglycerin (sublingual/aerosol) Bronchodilator (inhaler) “Sugar” (or glucose) Others “as training and needs mandate” “Essential” Emergency Drugs (Haas, Dent. Clin. N. Am., 2002:46:815-830) • • • • • • Oxygen Epinephrine Nitroglycerin Antihistamine Beta agonist (bronchodilator) Aspirin “Supplementary” Emergency Drugs (Haas, 2002) • • • • • • • • Glucagon Atropine Ephedrine Hydrocortisone Morphine (or nitrous oxide) Naloxone Lorazepam or midazolam (seizures) Flumazenil “Proprietary emergency drug kits are available, but none of these kits is compatible with the needs of all practitioners. The Council on Scientific Affairs does not recommend any specific proprietary drug kit.” JADA 2002;133(3):364-365 Oxygen Cylinders and Volumes • E: 625 liters • H: 6,909 liters Time Available at 15 L/min Flow Rate (from 2,000 psi fill) • E cylinder = 41 minutes • H cylinder = 460 minutes • Reduce times by ½ at 1,000 psi Appropriate Use of Oxygen • Any suspected cardiopulmonary emergency • Complaints of shortness of breath and suspected ischemic pain • For patients with suspected stroke or unknown blood oxygenation • May be administered to patients who are not hypoxemic Precautions: Oxygen • Observe closely when using with patients known to be dependent on hypoxic drive (COPD; very rare) • Pulse oximetry may provide a useful method of assessing oxygenation (may be inaccurate in low cardiac output, with vasoconstriction or with CO poisoning) Oxygen Flow Requirments (ACLS) • Nasal cannula: 1-6 L/min, 21-44% • Venturi mask: 4-12 L/min, 24-50% • Partial rebreather mask: 6-10 L/min, 3560% • Nonrebreather mask with reservoir: 6-15 L/min • Bag-mask with nonrebreather “tail”: 15 L/min, 95-100% Positive-Pressure Ventilation A nitrous oxide nasal hood CAN NOT provide positive-pressure ventilation Supplementary Oxygen vs. Positive-Pressure Ventilation with 100% Oxygen Epinephrine • Only injectable agent which should be available in ALL dental offices • Use pre-loaded syringes (not ampuls) • Use 1:1,000 by sublingual or I.M. route only • Adult dose = 0.3 mg, q. 5-10 min & monitor CV status before re-dosing • Produces bronchodilation, cardiac stimulation and vasoconstriction Epinephrine Precautions • Elevations of BP and increased HR may cause ischemia, increased O2 demand and dysrhythmias • Avoid accidental injection of rescuer Whenever epinephrine or another emergency drug is administered, medical assistance must be summoned Other Bronchodilators • Beta-2 Agonists • Terbutaline Beta-2 Adrenergic Agonists • • • • Albuterol (VENTOLIN)(first choice) Metaproterenol (ALUPENT) Terbutaline (BRETHAIRE) Peak onset = 30-60 minutes Albuterol (PROVENTIL, VENTOLIN) • Use by inhalation route for emergency airway constriction • May produce sympathomimetic CV effects (tachycardia, palpitations, elevated BP) • May be ineffective or partially effective if patient taking beta blockers Nitroglycerin • • • • Available in 0.4 mg sublingual tabs Decreases cardiac work load Administer 1 tab q. 5 min up to 3 times Also available in spray form (more stable)(1-2 sprays q. 5 min up to 3 sprays) • May produce hypotension (do not use if hypotension present) Nitroglycerin Precautions • Avoid in patients taking drugs for ED • May cause excessive decrease in BP with syncope (patient should be in sitting or reclined position when taking) Aromatic Spirits of Ammonia • Irritates respiratory mucosa, causes muscle contractions, improves venous return • Dose = inhaled vapors of one crushed ampul • Supplied as 0.3 ml “vaporole” Glucose/Sucrose • Acceptable forms of sucrose include soft drinks, orange juice & candy bars • Glucose also available • Do not use oral dose forms in unconscious patient • Long onset (10 min) Antihistamines • Diphenhydramine (BENADRYL) (50 mg/ml) • Chlorpheniramine (CHLOR-TRIMETON) (10 mg/ml) • DO NOT subsitute for epinephrine in anaphylaxis Aspirin • Indicated in all patients with ACS • Any person with symptoms of “pressure, “heavy weight”, “squeezing”, or “crushing” (suggestive of ischemia) • DO NOT administer in aspirin-allergic patients • Relatively contraindicated in ulcer disease or asthmatics Aspirin Dosage • 160 – 325 mg non-enteric coated tablets ASAP • Chewing is preferred • May use rectal suppository form (if available) Atropine • • • • Indicated for bradycardia Rapid onset, short duration 0.5 mg i.m. q. 3-5 min up to total of 3 mg Avoid excessive reductions of heart rate and use in patients susceptible to adverse anticholinergic effects • Also used for organophosphate poisoning References • Malamed, Sedation: A Guide to patient management, 4th edition, 2003 • Jackson & Johnson, Conscious sedation for dentistry: risk management and patient selection, Dent. Clin. N. Am. Vol. 46, 2002 • American Dental Association, Guidelines for the use of conscious sedation, deep sedation and general anesthesia, 2007. Local Anesthetic Dosages • ALWAYS calculated on basis of body weight (mg/kg) • Absolute maximum dosage reached at body weight of 70 kg (150 lbs) • Apply to a single appointment • Adjusted downward to compensate for drug interactions, medical conditions Maximum Doses of Selected Local Anesthetics • • • • • Lidocaine (4.4 mg/kg, 300 mg absolute) Mepivacaine (4.4 mg/kg, 300 mg absolute) Prilocaine (6 mg/kg, 400 mg absolute) Articaine (7 mg/kg, 500 mg absolute) Bupivacaine (1.3 mg/kg, 90 mg absolute) Other Informational Resources • Mosby’s Drug Consult, 800-545-2522 • Mosby’s Dental Drug Reference, www.elsevierhealth.com • Drug Interaction Facts, Facts & Comparisons, 800-223-0554 • www.rxlist.com • www.drugfacts.com • www.med.umich.edu/1lib/aha/umherb01 Local Anesthetics Approaches to Failed IABs… • Reinject (if lower lip not numb)? • Increase local anesthetic concentration (prilocaine, articaine)? • Increase the vasoconstrictor concentration? • Wait? • Apply the “Volume Rule”? • Apply the “Real Estate Rule”? How long should you wait? Varies with anesthetic and tissue Lip = 5-7 minutes Pulps = 10-15 minutes >15 minutes (~1 in 4 patients) >30 minutes (~1 in 10 patients) Longer-acting anesthetics have longer onsets (Marcaine) Malamed et al., JADA 2000, 2001 • 2% lidocaine with 1:100K epi vs. 4% articaine with 1:100K epi • 882/443 articaine/lidocaine subjects • Used “simple” (single extractions, etc) and “complex” (alveolectomies, etc) for evaluations • Articaine “is an efffective agent acting in the standard lidocaine-mepivacaine range” • Clinical performance not sufficiently different to qualify it as a replacement for lidocaine Articaine vs. Other Agents • Absolute max dose (carts) < lidocaine (7.3 vs. 8.3) • Pregnancy category C (lidocaine B) • Available with 1:100,000 and 1:200,000 epinephrine Anesthetic Efficacy of Articaine for IABs in Patients with Irreversible Pulpitis Claffey E. et al. J. Endo. 2004;30:568-71 Claffey et al./Articaine • 72 cases of irreversible pulpitis • Compared 4% articaine 2.2 ml vs. 2% lidocaine with 1:100K epi 2.2 ml • All patients had “numb lips” • Endo access started 15 min post numbness • Success rates = 24% for articaine & 23% for lidocaine Results from Nusstein et al., J. Endo. 2003 • 33 emergency patients with irreversible pulpitis (mandibular posterior teeth with failed conventional IAB) • X-tip injection of 1.8 ml (2% lidocaine with 1:100K epi) • 18% “backflowed” (no success) » 82% of remaining injections successful Review of Intraosseous Injection Systems: ADA Professional Product Review, Volume 2, Issue 1, Winter 2006 • • • • • • Stabident X-Tip Intraflow (not evaluated) “Clinical performance” best feature X-Tip easiest to use Tachycardia most common concern Results from Replogle et al. (1999) • 67% of ASA I patients receiving IO injections of lidocaine 2% with 1:100K epi experienced significantly increased HR • Tachycardia averaged 28 bpm & lasted average of 4-5 min • Systolic & diastolic BP unchanged • No increased HR observed with 3% mepivacaine Paresthesia “An altered sensation of numbness, burning or pricking that may reflect an alteration in the sensation of pain in the distribution of a specific sensory nerve.” Proposed Causes of Paresthesia • • • • Direct nerve trauma by needle Barbed needles (“fish hook effect”) Intraneural hematoma Chemical toxicity of local anesthetics/high concentration local anesthetic (4%) • Surgical procedures following local anesthetic injection • Neural ischemia (vasoconstrictor???) “An inferior alveolar nerve block can cause occasional peripheral nerve damage. The exact mechanism is unknown and there is no known prevention or treatment.” Pogrel MA, Thamby S. JADA 2000;131:901-907 Haas, D. J. Am. Coll. Dent. 2006 • Focused on NON-SURGICAL cases • Evaluated in vitro and human clinical outcomes • All agents have potential for neurotoxicity, probably dose (concentration)-dependent • Nerves with fewer fasicles may be more susceptible (e.g., lingual) • RCTs not likely to discriminate differences between various local anesthetics Summary of Findings in IAB-Related Paresthesias • ~50% of patients experience “electric shock” sensation • 85-94% of cases recover in 8 wks or less • Tongue (79%) and lower lip most frequently affected • No difference between right and left sides • Nerve damage cannot be visualized or corrected surgically • Overall incidence of permanent paresthesia = 1:785,000 Conclusions of Haas (2006) • Data are “strongly suggestive” that paresthesia more likely with 4% agents • “Concentration, not drug per se” cause • Cited Royal College of Dental Surgeons (Ontario, 2005) (risks may outweigh benefits of 4% solutions for inferior alveolar and lingual blocks) Avoiding Paresthesia… • Use the lowest practical anesthetic and vasoconstrictor concentrations • Use the atraumatic injection technique • Check your cartridges • Don’t subject your cartridges to temperature extremes • Avoid operative neural trauma (careful use of forceps, elevators, rubber dam clamps, etc.) New Perspectives on Pain Control in Patients With Cardiovascular Disease E-References, Antiplatelet Drugs • Antman EM et al. Use of Nonsteroidal Antiinflammatory Drugs. An Update for Clinicians. A Scientific Statement from the American Heart Association. Circulation, February 26, 2007 • http://www.circ.ahajournals.org/cgi/content/full/1 15/6/813 NSAID Classes • • • • • • • • Salicylic acid derivatives (diflunisal/DOLOBID) P-Aminophenols (acetaminophen/TYLENOL) Indole acetic acids (etodolac/LODINE) Aryl acetic acids (diclofenac/VOLTAREN, ketorolac/TORADOL) Propionic acids (ibuprofen/MOTRIN, naproxen/ANAPROX, ketoprofen/ORUDIS, flurbiprofen/ANSAID) Fenamates (mefenamic acid/PONSTEL) Alkanones (nabumetone/RELAFEN) Diarylheterocycles (selective COX-2 inhibitors) Beneficial Effects of NSAIDs • Analgesic (relieve pain) • Antipyretic (reduce fever) • Anti-inflammatory • Available OTC The Oxford League Table of Analgesic Efficacy www.jr2.ox.ac.uk/bandolier/booth/ painpag/Acutrev/Analgesics/lftab. html Oxford League Table of Analgesic Efficacy/NNTs (www.jr2.ox.ac.uk/bandolier)(moderate-severe pain) • • • • • • • • • • • Valdecoxib 40 mg: 1.6 Ibuprofen 800 mg: 1.6 Ketorolac 20 mg/60 mg: 1.8 Diclofenac 100 mg: 1.9 Rofecoxib 50 mg: 1.9 APAP 1,000 mg + codeine 60 mg: 2.2 APAP 500 mg + oxycodone 5 mg: 2.2 Naproxen 440 mg: 2.3 Ibuprofen 600 mg: 2.4 Ibuprofen 400 mg: 2.4 Morphine 10 mg i.m.: 2.9 Relative Efficacy of Oral Analgesics After Third Molar Extraction Barden J, Edwards, JE, McQuay HJ, Wiffen PJ, Moore RA British Dental Journal 2004;197:407-411 NNTs from Barden et al. • • • • • • • • • Valdecoxib 40 mg (BEXTRA): 1.6 Diclofenac 100 mg (VOLTAREN): 1.6 Ibuprofen 400 mg: 4.7 Ibuprofen 200 mg: 4.6 Ibuprofen 600 mg: 1.9 Celecoxib (CELEBREX): 4.8 APAP 1,000 mg: 3.8 APAP 600 mg + codeine 60 mg: 2.5 APAP 300 mg + codeine 30 mg: 3.3 Contraindications to NSAIDs • • • • • • Stomach problems Aspirin Allergy Bleeding Pregnancy Kidney disease CARDIOVASCULAR DISEASE/RISK OF THROMBOEMBOLISM Conditions With Risk for NSAIDInduced Nephropathy • Volume depletion/dehydration (diarrhea, vomiting) • Renal insufficiency • Heart failure • Diabetes • Advanced age • Kharasch, E. Anesth. Analg. 2004;98:1-3 COX-2-Selective Inhibitors Selecting new drugs for pain control: evidence-based decision or clinical impression? Jeske, AH. JADA 2002;133:1052-6 Conclusions • VIOXX = 400 mg ibuprofen • VIOXX has 50% “rescue” rate within 24 hrs • Ibuprofen = VIOXX G.I. problems for 30 days • VIOXX not OTC Single dose oral celecoxib for postoperative pain (Barden J et al. Cochrane Review: Issue 3, 2004)** Similar in efficacy to aspirin 650 mg and APAP 1,000 mg Evaluated 200-mg dose (more studies needed for 400-mg dose) Moderate to Severe Post-Op Pain 4-6 Hours The Use of COX-2 Inhibitors for Acute Dental Pain: A Second Look Huber, MA and Terezhalmy, GT. JADA 2006;137:480-7 Unresolved Issues: NSAIDs • COX-2 constitutively expressed in some tissues (brain, kidney, ovary & uterus) • COX-2-synthesized PGs are pro-inflammatory early, may reduce inflammation & promote healing later • Is opioid-sparing effect significant? • Cardiovascular side effects? (prostacyclin vs. thromboxane A-2, salt and water retention) COX-2 inhibitors • • • • Celecoxib (CELEBREX) Rofecoxicb (VIOXX) Etoricoxib (ARCOXIA) Lumiracoxib (PREXIGE) (Thromboxane antagonist???) • Valdecoxib (BEXTRA) Effects of NSAIDs on Platelet Aggregation • Thromboxane A2 = vasoconstrictor, promotes platelet aggregation • PG I2 = Vasodilator, inhibits platelet aggregation • COX-2 inhibitors prevent synthesis of PG I2 but have no effect on TX A2, resulting in a prothrombotic state Use of NSAIDs. An update for clinicians. A Scientific Statement from the American Heart Association Antman, E. M. et al. Circulation February 26, 2007 AHA Recommendations 2007 for Patients With Cardiovascular Disease • Acetaminophen, aspirin and opioid analgesics (incl. tramadol) preferred for short-term pain management • If NSAID is needed, naproxen “appears to be the preferred choice” • Prescribe at lowest effective doses for shortest possible period of time • Diclofenac not recommended as NSAID in this group of patients • Ibuprofen should be given 30 mins AFTER low-dose aspirin or 8 hrs before (if use concomitantly) PRECISION…coming to a journal near you! Prospective Randomized Evaluation of Celecoxib Integrated Safety vs Ibuprofen or Naproxen www.clinicaltrials.gov No. NCT00346216 Single Dose Oral Acetaminophen for Postoperative Pain (Barden J et al., Cochrane Review, Issue 3, 2004)** 325 mg, 500 mg, 650 mg, 975-1,000 & 1,500 mg doses vs. placebo 1,000 mg = 1,500 mg (NNT 3.8 vs. 3.7) Adverse Effects of 9751,000 mg = placebo (!) Preferred Oral Opioid Analgesics • Tylenol with codeine #2: (2 or 3 q. 4 h.) • Hydrocodone 2.5 or 5 mg with 500 mg APAP (1 or 2 q. 4 - 6 h.) • Oxycodone 5 mg with 500 mg APAP (e.g., TYLOX) (1 or 2 q. 4 - 6 h.) • Oxycodone 5 mg with 400 mg ibuprofen (COMBUNOX)** Other Oral Opioid Analgesics • Tramadol (ULTRAM): 50 100 mg q.4 -6 h. (now available with APAP as ULTRACET, 35/325) • VICOPROFEN: 1 tab q. 4 – 6 h. • Pentazocine (TALWIN COMPOUND, TALACEN) • Propoxyphene (DARVON COMPOUND, DARVOCET) • VOPAC (650 mg APAP + 30 mg codeine) MAGNACET® (March, 2007) • • • • • • Oxycodone + acetaminophen 400 mg (?) 2.5, 5, 7.5 and 10 mg oxycodone (?) Schedule II “Moderate to moderately-severe pain” “Gives physicians flexibility” Compare with PERCOCET, TYLOX & COMBUNOX Results from Dionne, R. J. Oral Max. Surg. 57:673, 1999 • Compared 400 mg ibuprofen + 2.5, 5 and 10 mg oxycodone • Only 10 mg oxycodone was superior to 400 mg ibuprofen alone • Opioid adverse effects were dose-related • 65% drowsy, 20% nauseated & 16% vomited at 10 mg oxycodone