UNIT 1
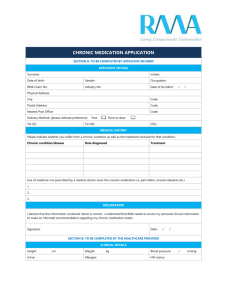
advertisement

UNIT 1
Chronicity: Older Adult
Gordons Functional Health Pattern
Self-Perception and Self-Concept
•
1.
2.
3.
Unit objectives: The student will be able to:
Discuss the effects of aging.
Define chronic illness
Describe characteristics of chronic conditions and implications
for people with chronic conditions and for their families.
4. Discuss four functional health patterns [FHP’s] that most elderly
and/or chronically-ill clients would fit.
5. List measures to promote safe drug use in the elderly.
6. Describe the legal and ethical responsibilities in caring for the
elderly and/or clients with chronic conditions.
8.
Describe the use of effective teaching methods for the elderly.
9.
Identify specific needs of the chronically-ill client as related to
their stage of development according to the last two stages of
Erickson’s psychosocial theory.
10. Describe the components of the Patient Self-Determination
Act.
11. Descibe how nurses should use “people-first” language
12.
Required Reading:
Smeltzer: Chapters: 7,10,12
Eliopoulos: Chapters: 1,6,17,29,32,35,36
Case Studies in this syllabus (end of powerpoint)
Hand in the answers at the first class meeting.
Changes of Aging
• Aging is not a disease
– Intrinsic aging – normal aging, genetically
programmed
– Extrinsic – air pollution, sunlight, occupation
Physical Changes of Aging
• Body composition– Body cells become less able to replace themselves
– Reduced lean body mass
– Decreased in ICF risk of dehydration
– Hair thinning/loss, grey hair
– Body fat atrophies double chin, baggy eyelids,
deepening of intercostals spaces,
– Skin-folds thickness is reduced in forearm & back of
hands, loss of sub q fat “c/o being cold”
– Body shrinkage due to loss of cartilage & thinning of
vertebrae
– Lower normal temperature
Physical Changes of Aging
– Cardiovascular changes• Decreased contractility, impaired coronary blood flow, altered preload &
afterload, increased atherosclerotic plaques, vessels tortuous, heart
valves thick & rigid
– Respiratory events• rigidity of thoracic cage, decreased vital capacity, decreased cough
efficiency , decrease ciliary action
– Renal changes• Decrease bladder capacity, decreased concentrating and diluting
abilities, decreased creatinine clearance & prostate size
– Endocrine changes• Thyroid – fibrosis & increased nodularity, decreased basal metabolism,
• Pancreas - delayed & insufficient release of insulin by beta cells,
• Pituitary - decrease in volume by approx 20%.
Physical Changes of Aging
– Gastrointestinal changes
• Tooth loss, decreased saliva, altered nutritional
digestion, weakening of lower esophageal
sphincter, decrease in blood flow, decrease
size in organs, decrease peristalses
– Nervous system
• Structural changes: decreased neurons &
speed of conduction, brain wt, & peripheral
nerve function,
• Functional changes: decreased reaction time,
impaired thermoregulation, changes in sleep
patterns
Physical Changes of Aging
– Sensory• Vision changes: presbyopia; susceptible to
glare; difficult distinguishing blue & green
• Hearing changes: presbycusis, loss of high
frequency sounds, wax build up
• Taste: decreased sweet, salt & seasoned food
taste
– Reproductive• Female: vaginal mucosa thinning, atrophy,
decreased breast tissue,
• Male: decreased libido
Physical Changes of Aging
• Dermatologic
– Decreased elasticity, decreased secretion of
natural oil & perspiration, decreased heat
regulation, decreased epidermal renewal,
decreased inflammatory
Critical Thinking: Multiple Response
(Select all of the normal age-related physiological
changes)
•
•
•
•
•
•
•
-Decline in visual acuity
-Decreased Respiratory rate
-Increased hear rate
-Increased heart rate
-Increased susceptibility to UTIs
-Decline in long-term memory
-Increased incidence of awakening after sleep onset
Chronic illness
• Occur in people of every age, socioeconomic level, and
culture.
• Medical conditions or health problems with associated
symptoms that require long-term (3 months or longer)
management.
• Conditions that do not resolve or for which complete cures are
rare.
• Management means that people must learn to live with the
symptoms or disabilities, and carry out lifestyle changes or
treatment regimens.
Causes of the Increase in Chronic Conditions Include:
•
•
•
•
•
Decrease in mortality for infectious diseases.
Longer life spans.
Improved diagnostic and screening procedures.
Improved management of acute conditions.
Chronic illness is more likely to develop with advanced
age.
• Lifestyle factors such as smoking, stress, sedentary
lifestyle, and obesity.
Characteristics of Chronic Conditions
•
•
•
•
The patient must adapt and change physically,
socially, and emotionally.
Usually involve different phases over the person's
lifetime to which the person must adapt.
Require adherence to therapeutic regimen.
One chronic disease or problem can lead to another.
Chronic disorders contribute to higher risk of mortality
and morbidity from other illnesses.
Characteristics of Chronic Conditions
• Affect the entire family.
• Day-to-day management is the responsibility of the
person and/or his/her family.
• Each person’s management of his/her condition and
his/her body’s response to the condition is unique.
• Management is collaborative.
• Management is expensive.
• Ethical issues may be raised; for example, cost
control and quality of life.
• Living with chronic illness means living with
uncertainty.
Question
Which of the following is an inaccurate cause of the increase in
the number of chronic conditions?
a. Lifestyle factors, such as smoking and stress
b. Improved diagnostic procedures
c. Shorter life spans
d. Improved management of acute problems
Implications for Managing Chronic Conditions
• Importance of prevention
• Lifestyle changes/interventions to prevent chronic
disease
• Once the disease occurs, focus shifts to:
– Managing symptoms
– Avoiding complications
– Avoiding acute illness
– Promoting health
– Maintaining functional status
Challenges of Living with Chronic Illness Include:
• Alleviating and managing symptoms.
• Psychologically adjusting to and physically
accommodating disabilities.
• Carrying out treatment regimens.
• Validating self-worth and family functioning.
• Managing threats to identity.
Challenges of Living with Chronic Illness Include:
• Normalizing personal and family life as possible.
• Living with altered time, social isolation, and
loneliness.
• Establishing support networks.
• Returning to a satisfactory way of life.
• Dying with dignity.
• Being aware that the patient may need to deal with
multiple chronic problems at one time.
Use of Nursing Process
•
•
•
•
Identify problems; assessment.
Establish and prioritize goals.
Define the plan of action.
Implement the plan:
– Work with patient and family.
– Adherence to treatment regimen
– Disease and complication prevention
– Deal with psychosocial issues.
• Follow-up and evaluate
Medication Usage
• Yr 2000 – 16% of adults are over 60 and take 40% of
drugs prescribed
– 4.5 drugs / person
• 40 -50% of OTC drugs used by elders
Drug misuse
•
•
•
•
•
•
•
Memory impairment
Failure to accept diagnosis
Unacceptable side effects
Inaccessibility to drugs
Knowledge deficit
Vision impairment
Low literacy
Multiple drug use
• Multiple drug use hospitalizations:
– Decrease absorption, distribution, metabolism &
excretion
– Impaired circulation causes decrease transport to
tissue
– deposit in fat causes high risk for cumulative effects
– ↓ liver & kidney function
Promotion of safe drug use
• Simplify the medication administration process
– Is drug necessary? Smallest possible dose ordered?
Undesirable Side effects? Interactions w other drugs?
Induce malnutrition? Allergies?
• Disseminate knowledge
– Patient & family education: oral & written explanation,
[graphics, info sheets, Rx labels, booklets]
• Teach proper medication management skills
– Written schedule of administration
– Daily/weekly drug containers
– Drug containers: non-childproof; large print; color
coded
M.A.S.T.E.R.
• Minimize the number of meds needed
• Alternate drugs (if possible)
• Start w a low dose and go slow if dose has to be
increased
• Titrate therapy to the individual patient
• Educate the patient
• Review regularly
Legal & Ethical Issues
• Adult Protective Services = refers to range of services –
medical, social, and legal that are provided to the frail
elderly
• Conservatorship – court appointed conservator makes
decision about where an individual lives and how his/her
needs are met
• .
Patient Self Determination Act
• Mandated by Congress in 1990 to preserves an
individuals right to decisions related to personal
survival
• Relates to any medical situation in which the
individual becomes unable to communicate their
choices
• Written info is given at time of admission
Advance directives
• Power of attorney – affords assistance in handling
legal affairs; valid if the person granting PoA is
capable of doing so; time limits must be specified
• Durable P of A for health care – appointed by the
individual to make decisions regarding care in acute
illnesses; may be family, friend, or significant other;
must be notarized.
Advance directives
• Living will – a personal statement of how one wishes
to die. Sets forth choices and instructions for end of- life care.
DNR
DNR is an order written by a physician when a client
has indicated a desire to be allowed to die if the client
stops breathing or the client’s heart stops beating.
Elder abuse
• Abuse & neglect of the elderly are used to describe
elders > 65 experiencing battering, verbal abuse,
exploitation, denial of rights, forced confinement,
neglected medical needs at the hands of people
responsible for assisting them w their ADL’s.
– Estimated 1 – 2 million per yr.
– Mandatory reporting
Psychosocial
• Erickson’s Development Tasks
– Generativity vs. Self-absorption
– Integrity vs. Despair - one could look back on life
with integrity or despair
Psychosocial
• Learning/education
– The normal aging process
– Lifestyle changes to stay healthy
– Their chronic illness
– Organizations/services to help w independence,
• AARP, Gray Panthers, senior citizen center, assisted
living centers, day care programs, home delivered meals,
long term care facilities, hospice
Psychosocial
• Sexual
– Lack of a partner
– Psychological barriers
– Physical barriers
– Cognitive impairment
• Economic
– Retirement issues
• Intrafamily problems
• Cultural
– Ageism- prejudice against or dislike of older people purely
because of their age
Modification of Strategies Specific for the Elderly
• Slower pace of presentation of material
• Adjust time for learner condition and attention span
• Use repetition/reinforcement
• Avoid distractions; modify the teaching environment
• Large print, non-glare paper, use of color
– Difficulty seeing and difficulty with color perception
• Voice
– Difficulty hearing
• Involve family and significant
IMPLEMENTATION
• education
– Address client’s needs, and let the needs ‘direct” the
content.
– Focus on the “must know” information
– Be specific & unambiguous
– Teach at every opportunity
– Seek frequent feedback
– Respect and build on the elder’s experience
Guidelines for effectively teaching older adults
• Vision – large easy-to-read typeface; emphasize black &
white; avoid blues & greens; use non-glare paper, write
short simple paragraphs, make sure glasses are clean &
in place.
• Hearing – speak slowly; enunciate clearly; lower pitch of
your voice, eliminate background noise; face the learner;
use nonverbal cues; have hearing aid in place & working
correctly
Guidelines for effectively teaching older adults
• Energy level / attention – use short teaching sessions,
offer liquid refreshments & bathroom breaks, promote
comfort
• Information processing/memory – present most
important info first, clarify information w use of examples;
motor skills – teach one step at a time {have written easy
to understand instructions}; be concrete & specific,
eliminate distractions; correct wrong answers/ reinforce
correct answers; offer praise & encouragement
Questions to Ask to Ensure Quality Care
• Does the patient require or prefer special
accommodations?
• Are special accommodations made to communicate
with the patient?
• Are efforts made to direct all conversations to the
patient rather than to others who have accompanied
the patient?
Accessibility of Health Care
• Are health care facilities accessible as legally
required?
• Has accessibility been verified by a person with a
disability?
• Is a sign interpreter, other than the family, available?
• Does the facility have appropriate equipment to
provide heath care for a person with disabilities?
Health Promotion
•
•
•
•
•
Do not neglect health promotion issues.
Need for healthy diet
Exercise
Social interaction
Preventive health screening
Importance of Language
• Use “people-first” language.
• The person, not the illness or disability, is most
important.
Question
Tell whether the following statement is true or false.
An example of people-first language is “the person with
a disability.”
Case Study, Unit 1 , Health Care of the Older Adult
The nurse is completing the admission assessment for a patient scheduled for cataract
surgery in the outpatient center. Because the patient is over the age of 70 and has several
chronic conditions, including hypertension and congestive heart failure, the nurse focuses
on completing a thorough medication history.
What questions should the nurse include in the medication history?
The patient states that she stopped taking one of her medications due to cost, since
her health insurance would not reimburse for the medication. What are other
reasons that older adults may be noncompliant with ordered medications?
How does aging affect drug absorption, metabolism, distribution, and excretion?