Labels of Pain Management Is it really addiction
advertisement

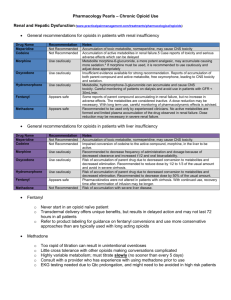
Randall Henthorn, MD Anesthesiology/Pain Management U of Oklahoma Health Sciences Center 5 Oct 2012 In the United States: ~ 8% of population has used an illicit drug in past month ~ 6-15% of the U.S. population have a substance abuse disorder ~ 2.8% of people have used a prescription drug for nonmedical reasons Substance Abuse and Mental Health Services Administration. (2007). Results from the 2006 National Survey on Drug Use and Health: National Findings. Retrieved April 24, 2008, from http://www.oas.samhsa.gov/nsduhLatest.htm SAMHSA Survey 2010 SAMHSA Survey 2010 SAMHSA Survey 2010 SAMHSA Survey 2010 SAMHSA Survey 2010 SAMHSA Survey 2010 Answer: Generally no, excepting those with: • Personal history of substance abuse • Young age- especially 18-23 • Family history with chemical abuse • Preadolescent sexual abuse • ARCH GEN PSYCHIATRY 2000 57;10: 953-9 15.0 Million Substance Use Disorder (SUD) Only 19.3 Million 5.6 Million Serious Psychological Distress (SPD) Only 2006 (SAMHSA survey) 11 Interventional pain management study 500 Patients taking supplemental opioids UDT with rapid drug screen Overall 16% positive for either THC (11%), cocaine (5%), Meth/amp(2%) Age <45 (26%) 45-64(13%) >64 (0%) of the 500. Medicaid> 3rd>Medicare +Medicaid> Medicare w/o 3rd ◦ Pain Physician 2006 9:2 123-129 ALCOHOL ABUSE slightly greater than general population (10-18%) Webster RL and Dove B Avoiding Opioid Abuse While Managing Pain. Sunrise River Press 2007 page 19 GENERAL ADDICTION TO OPIOIDS-1%. Addiction in chronic pain patients in opioid dependent pain patients 2-5% ◦ Pain Med:2005,6(6):432-42 Substance abuse Substance dependence-Addiction Substance specific withdrawal syndrome Tolerance Pseudoaddiction Pseudotolerance Maladaptive pattern of abuse producing significant impairment or distress in a 12 month period with one or more ◦ Recurrent substance use leading to failure to fulfill major role obligations at work, school, or home ◦ Recurrent use in situations in which it is physically hazardous (e.g., driving while being impaired) ◦ Recurrent substance –related legal problems (e.g., arrests for disorderly conduct) ◦ Continue use despite recurrent social and interpersonal problems caused by the effects of the substance (e.g., intoxication-induced arguments, fights) Intentional overuse of the substance during periods of celebration, anxiety, despair, or result of self-medication or ignorance. A maladaptive pattern of substance use that leads to clinically significant impairment or distress. Abusers may or not be addicted, Can often stop use. Frequently stop when harm occurs. According to US Substance Abuse and Mental Health Services Administration Drug abuse is “any non-medical use of a substance.” Any use of medication in defiance of medical direction. ◦ Webster L and Dove Beth: Avoiding Opioid Abuse While Managing Pain. Sunrise River Press 2007 pages 24-27 Opioid addiction is a primary, chronic, neurobiological disease, with genetic, psychosocial, and environmental factors influencing its development and manifestations. It is characterized by behaviors that include one or more of the following: impaired control over drug use, compulsive use, continued use despite harm, and craving. ◦ American Academy of Pain Medicine, American Pain Society, American Society of Addiction Medicine, 2001. Associated with the limbic region of the brain designated as the “reward center” ◦ Opioid as well as other receptors related to potentially other addictive substances are located here and can cause excessive release of dopamine. ◦ Dopamine excess can causes sensitization pathways in the limbic system and reinforce the acquisition of use of substances of abuse. Physical dependence is a state of adaptation that is manifested by a drug class specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug, and/or administration of an antagonist. ◦ It is physiological response prolonged drug exposure. ◦ Many non-abused medications have withdrawal symptoms e.g., clonidine, beta-blockers, and baclofen to name a few. Systems are Dysphoric mood, nausea vomiting, muscle aches, lacrimation or rhinorrhea, pupillary dilation, lacrimation, piloerection, diarrhea, yawning, fever, and insomnia ◦ DSM-TV-TR To avoid, taper the opioid by 10-15% over 48-72 hours over a 2-3 weeks ◦ Wilsey BL and Fishman S: Long-term Opioid Therapy, Drug Abuse and Addiction The Massachusetts Handbook of Pain Management 3rd Ad,2006, Lippincott Williams and Wilkins “Tolerance is a state of adaptation in which exposure to a drug induces changes that result in diminution of one or more of the drug’s effects over time.” Generally periodic opioid dose escalation is needed to sustain analgesia. Many of the non-analgesic side effects disappear as a result e.g, sedation, cognitive impairment, and others. Unfortunately constipation usually stays. Opioid-Induced Hyperalgesia is a rare phenomenon whereby the tolerance mechanisms are excessive and making the pain worse. In this case restoration of analgesia requires either the opioid be reduced or anther opioid given. Process is thought to largely involve facilitated NMDA activity and hopefully specific antagonist will be developed against it. Pharmacologic Tolerance OIH 1 5 Large dosage increase is frequently needed to restore analgesia 10 Analgesi a 5 0 0 2 3 Dose 4 5 Kinetics of chronic drug action Cox B: Mechanisms of tolerance. Opioids In Pain Control Christopher Stein, ed., Cambridge University Press, 1999. Associated with the under treatment of pain Manifested by behaviors similar to addiction ◦ ◦ ◦ ◦ Clock watching Focus on obtaining drug Aberrant behaviors Behaviors resolve with increase opioid dosage other intervention that relieves the pain ◦ American Academy of Pain Medicine, American Pain Society, & American Society of Addiction Medicine. (2001). Public policy statement on definitions related to the use of opioids in pain treatment. Retrieved October 5, 2007, from http://www.ampainsoc.org/advocacy/opioids2.htm Need to increase the dose for reasons other than pharmacologic tolerance Reasons may include: ◦ ◦ ◦ ◦ ◦ ◦ Disease progression New disease Anxiety Increased activity Adherence issues Addiction Jimmy is 36 year-old male mechanic drove his truck off the road and hit utility pole. He barely missed a pedestrian in the crosswalk at 2100. ESMA transported him to trauma center. He sustained multiple rib fractures on left chest, pelvic fracture, and spleen laceration. Chest tube was placed for small hemopneumothorax. Apart from sinus tachycardia vitals were normal and SPO2 95 on mask at 40 % oxygen. Glasgow Coma Score is 14 and CT neck free of fractures. Hg is 10.2 Blood alcohol is 0.17 and urine positive for opioids and cannabinoids. No allergies Medical history: Hypertension, BMI-38, sleep apnea, lumbar laminectomies and fusion at L4-5 and L5-S1. Medications: Oxycontin 40-mg tid, oxcodone 10-mg/APAP 325mg qid along with Neurontin 300-mg tid has been prescribed for 1 year for back and leg pain. Reports running out of pain meds 2 days ago. Takes 10 x 200 mg OTC Ibuprofen daily. Takes Linsinopril 10 mg daily and Zoloft 50 mg daily two months ago for depression. 3 months ago he underwent divorce has 2 teenage middle school children in spouse’s custody. Jimmy has been temporarily living with mother who is an alcoholic in recovery. Mother states he has been upset but states he drinks only 2 beers nightly. Jimmy never knew father. Older sister states Jimmy has been addicted to pain killers for years, consequently avoids interaction. Jimmy smokes and chews tobacco. Surgeons elect to observe in ICU. He was given a total 10-mg of IV morphine during the first hour in ER. Reports pain > 10/10, mainly in left chest at chest tube site. He reports it hurts to breath and cries out frequently “Can’t you see I ‘m hurt”. Morphine is prescribed 2- 4 mg IV P.R.N. pain every 30 min. Surgeons “don’t want to mask the exam or slow the respirations” with too much morphine. They do allow fentanyl-mcg 50-100 IV bolus every 2-hours if he is alert. Lidoderm patches are placed over the rib fracture sites. IV acetaminophen 1000 mg is given q 8 hours. When the nurse gives IV medication, Jimmy insists that she hurry it up and five fast. 2 hours after admission the pain score is still greater than 10/10 on numerical scale. Screams frequently vulgarities with small bodily movements. He is diaphoretic, hurts all over, and nauseated, despite Zofran 4-mg every 6 hours. RR is 26/min and breathing pattern is shallow. He has to be restrained for trying to get out of bed. Mother is furious about inadequate treatment of pain. She has been worried for weeks about his low mood and energy, wishing at times death. Pain consult requested by surgeons. 6-hours after admission serum creatinine is 2.5 mg and BUN is 30. K+ is 5.6 and Hg is 9.5 Answer: Start IV PCA with 2-3 mg of morphine loading doses up to 10-mg within 30 minutes. In this case convert the prehospital Oxycodone to IV morphine equal and give it as basal infusion. An estimate of daily pre-hospital Oxycontin plus Perocet conversion is: ◦ PO Oxycodone 20-mg = 30 mg PO morphine ◦ Then the total 160 mg Oxycodone x 1.5 = 240 mg PO morphine ◦ P0 divided by 3 (3:1 rule) divided by 24 hours/day = 3.3 mg per IV per hour Oral (mg) Parental (mg) Morphine 30 10 Dilaudid 7.5 1.5 (2) 20 ------- hydromorphone Oxycodone Comment Duration (hr) MSIR, 3-6 MS-ER, 8-12 Exalgo 24 hour Oxycodone SR slow-release Fentanyl Patch 0.1 mg 8-12 25 mcg/hr = 45 mg/24 American Pain Society Equianalgesic Conversion 6th Edition -2008 PCA Morphine with 1.5 mg every 10 mg with hourly limit of 12 mg. Set basal at 3 mg to cover the oxycodone to morphine conversion. Hydromorphone could work as well but 5x more potent. Continue Fentanyl 50 mcg q 5 min to 100 mcg every 2 hour p.r.n. for movements bed significant bodily moves. Fentanyl is great for quick short but short duration analgesia, but not so good IV for IV PCA because its higher fat solubility which allows for rapid redistribution from the CNS effect site of action. Does he have pseudoaddiction? He wants the IV meds given fast. Is trying to get high? Did he show signs of opioid withdrawal syndrome. Does he have alcohol abuse disorder? What about the cannabinoids screen? What is the detection window for marijuana? Does positive test indicate he has addiction to it? What opioids or other addictive drugs can a routine hospital urine toxicology? Is he at risk for suicide and need psychiatric consult? Oklahoma Narcotics Prescription Monitoring check shows multiple doctor prescriptions for hydrocodone besides that of the family physician in the last 2 months and one prescribed alprazolam at 1.0 mg every hours p.r.n. anxiety x 60 tablets The family doctor office nurse was contacted the next morning and reports that ◦ last month came up 5-days short on the Percocet. ◦ last year lost half of his medication being stolen from glove compartment ◦ the doctor has not used the prescription monitoring system. ◦ the doctor did get a standard urine drug screen 3 months ago, it showed opiates and no illicit drugs. ◦ consent for continued opioid therapy is not in the chart. Pain controlled better with PCA regimen to 7/10. James escapes needing spleenectomy but the pelvis required ORIF on Post MVA day 3. Anesthesia does bupivacaine intercostal nerve blocks for 4 fractured ribs and gave Fentanyl 350 mcg intraoperative for pelvic surgery. Endotracheal tube extubation is OR. Report pain score 5/10 in PACU. Home CPAP used in the PACU and back in ICU. Post Operative IV PCA morphine was 1.5 mg q 10 min and basal at 2.0 mg/hour to total maximum hourly dose of 11. Chest tube removed 5 days after MVA and PO was started. Off his CPAP device and on nasal oxygen support. Hg 9.0 after 2 PRBC transfusion, and Cr decreased to 0.9. PCA morphine decreased to 1.0 mg q 12 and basal decreased to 1.0 mg. Analysis of last 8 hour shift showed 36 mg used. Pain worse in area of old back pain more than major injury sites. Reported score of 5/10 and taking deep breaths. James was started on MSContin rather than Oxycontin because potential cost savings as future outpatient. IV PCA removed. Estimated IV dose 90 mg/24 hours. Therefore according 3:1 rule would require about 270 mg daily PO. Speaker at this point would use MS Contin 75 mg tid with MSIR 15 q 8 hours for breakthrough. Pain score manageable at 5/10. Infrequently, requested breakthrough fentanyl injection. Patient progressively walked the halls progressively and lost 20 lbs during 2 weeks of hospitalization. Does not feel as depressed but worried about costs. Needs to get back to work. He was readied for discharge after urine catheter removed 8 days after MVA. Confront him that he has exhibited a series of aberrant drug seeking behaviors before the accident and explore what motivated that behavior suggest treatment. Suggest to PCP to refer to pain management specialist after discharge unless more is done to monitor the opioid abuse and diversion. Social services consult for financial aid while recovering from surgeries and get back to work in 2-3 months. Suggest exploring adequacy of depression treatment. Spiritual counseling? AA meetings? Chemical dependency consult? Perhaps ultimate detoxification from opioids in 3-4 months. Multidisciplinary Team Physician Addictionologist Nurse Patient Psych Sponsor Social Worker Counselor Monitor behaviors that seem “manipulative” ◦ ◦ ◦ ◦ Favoring one nurse over another Complimenting staff to obtain needs Exhibiting anger when needs are unmet Requesting IV medications be given “fast” Suspicious behaviors ◦ That arise after friends or families visit where the patient becomes unusually euphoric or cognitively impaired. Network with persons who can help these uniquely ill persons. Educate the family to supportive as substance abuse is notoriously difficult problem to treat. Educate that improvement in function is the best goal and not just reduction in the numerical pain score. Reassure that everything will be done to minimize distress or pain or combination thereof. Encourage the patient while in the hospital to stay focused on goals to improve function and self worth. Inadequate knowledge and fear of addiction hinder pain management in all patient populations Diagnosis requires ongoing assessment of aberrant behaviors along a continuum Goals of pain management include improving analgesia and activities of daily living, and controlling adverse events and aberrant behaviors Pain management requires effective communication and a multimodal approach including drug and nondrug strategies Patients with an addictive disease present unique challenges but deserve appropriate pain management