File - Nicole Sandhu

Problem Based
Learning: Group #3
By: Angela Manocha, Nicole Sandhu, Lary Muir, Kate
Montague, Carlita Branion-Calles, & Miranda Noyes
Objective:
1) Look at Maria’s background/ history and at the symptoms she is presenting
2) The potential causes and structures involved in producing these symptoms
3) A design of a rehabilitation intervention for the symptoms/ conditions: includes exercises and preventative techniques)
4) Solutions/ modifications/ activities that could alleviate and prevent the symptoms
1)Maria
Background and Symptomatology :
● Maria is 28 years old, and has been in a wheelchair since she was 14 years old.
● She has noticed some pain in her shoulder when she raises her hands above her head and symptoms continue to worsen
● It was found that her scapula-humeral rhythm is off o with the scapula having reduced upward rotation relative to the humerus movement
● In conjunction to the scapula-humeral impairment, her humerus is riding superiorly in the glenoid during the movement
Objective:
1) Look at Maria’s background/ history and at the symptoms she is presenting
2) The potential causes and structures involved in producing these symptoms
3) A design of a rehabilitation intervention for the symptoms/ conditions : includes exercises and preventative techniques)
4) Solutions/ modifications/ activities that could alleviate and prevent the symptoms
a) Functional Subacromial Impingement
● Accounts for 44-65% of patient shoulder pain complaints in doctor’s offices (Page, 2011).
● 65% of wheelchair users have experienced shoulder impingement (Cooper & Boninger, 1998).
● Common symptoms: o Pain when lying on affected shoulder o Pain when reaching for a seat belt o Pain when reaching behind back or neck o Pain when reaching above shoulder height (Miller,
2014).
● Commonly occurs in people who participate in repetitive overhead motions .
Structures Involved
a) Functional Subacromial Impingement
● Characterized by mechanical compression of the subacromial bursa, supraspinatus tendon, and the long head of the biceps tendon under the coracoacromial arch leading to irritation and inflammation of these structures (Prentice,
2006).
● This diagnosis was decided based on the following symptoms: pain with overhead reaching, altered scapulohumeral rhythm, and the superior riding of the humeral head in the glenoid fossa.
b) Dr. Janda Upper Crossed Syndrome
Commonly attributed as a cause of functional subacromial impingement, featuring the following muscle imbalances :
Weakness :
● Lower and middle trapezius
● Serratus anterior
● Infraspinatus
● Deltoid
Tightness
● Upper trapezius
● Pectorals
● Levator scapulae
Tightness within the Pectoralis Major/Minor
● Tightness in the pectoralis major also creates an anteriorly directed force which impedes upward scapular rotation(Labriola et al. , 2005).
● The pectoralis minor muscle also impedes the upward scapular rotation, external rotation and posterior tilt which is contributing to the decreased subacromial space and ultimately causing further impingement (Page,
2011).
● Tightness in the upper trapezius and weakness of the lower trapezius: o Imbalance causes an alteration in the scapular rotation
● Resulting in an upwardly directed migration in the axis of rotation of the glenohumeral joint (Page, 2011)
c) Muscular imbalance between the deltoid and rotator cuff muscles
● Since Maria is in a wheelchair, she is exerting high amounts of force using her deltoids.
● The upwards force of the deltoid is usually counterbalanced by the rotator cuff muscles, which help keep the head of the humerus in a neutral position
● Maria’s infraspinatus and teres minor muscles are weak
● This is causing an imbalance in force, and therefore, a loss of stability in the glenohumeral joint, which is a contributing factor in impingement.
Objective:
1) Look at Maria’s background/ history and at the symptoms she is presenting
2) The potential causes and structures involved in producing these symptoms
3) A design of a rehabilitation intervention for the symptoms/ conditions : includes exercises and preventative techniques)
4) Solutions/ modifications/ activities that could alleviate and prevent the symptoms
Rehabilitation
Process
Goal of Rehabilitation:
1.
Reduce pain and inflammation
2.
Manage shoulder impingement
Goal of Rehabilitation:
Manage shoulder impingement
How?
Improve scapulohumeral rhythm
• Proper scapulohumeral rhythm requires external rotation of the arm, depression of the scapula, and posterior tilting of the scapula (Ha, 2012)
• 2:1 ratio
• Increase subacromial space
What needs to be done?
1.
Improve upward rotation of scapula
2.
Increase retraction, depression, and posterior tilt of scapula
1.
Stabilize the humeral head into the glenoid fossa during arm elevation
2.
Increase external rotation of arm during elevation
1. Improve Scapular Upward Rotation
Why?
• Increases subacromial space throughout
ROM
• Increases glenohumeral stability for overhead work
• Improves recruitment efficiency of the scapulohumeral muscles
• late firing of the serratus and lower trapezius and over-dominance of the upper trapezius
•
Maintains the deltoid muscle in an efficient length-tension relationship above 90 degrees
1. Improve Scapular Upward Rotation
How?
Strengthen serratus anterior and lower trapezius
• Improve unison of upward rotators
(Loudon, Manske, & Reiman, 2013)
1. Improve Scapular Upward Rotation
How?
Stretch pectoralis minor and levator scapulae
• facilitates upward rotation to help prevent shoulder impingement during arm elevation
(Borstad & Ludewig, 2006)
2. Increase retraction, depression, and posterior tilt of scapula during arm elevation
Why?
• Increases subacromial space
(Escamilla, 2009)
2. Increase retraction, depression, and posterior tilt of scapula during arm elevation
How?
Stretch pectoralis minor
Stretch levator scapulae
Strengthen rhomboids and middle trapezius
Strengthen lower trapezius
3. Stabilize the humeral head into the glenoid fossa during arm elevation
Why?
• prevents superior gliding of the humeral head toward the acromion during arm elevation
• unopposed deltoid force will superiorly glide the humeral head
(Loudon, Manske, & Reiman, 2013)
3. Stabilize the humeral head into the glenoid fossa during arm elevation
How?
Strengthen rotator cuff muscles
• Collectively compress and dynamically stabilize the
GH joint through ROM
• Deltoid-rotator cuff force couple stabilize the GH joint by acting in opposite directions
(Loudon, Manske, & Reiman, 2013)
4. Increase external rotation of arm during arm elevation
Why?
Necessary for the greater tuberosity of humerus to pass under coracoacromial arch without impingement
(Escamilla, 2009)
How?
Strengthen infraspinatus and teres minor
Rehabilitation
Program
Timeline
•
Acute phase
• Reduce pain and inflammation
•
Stretching
•
Exercise Progression
Acute Phase: Reduce Pain and Inflammation
1) Ice can be used to ease the pain and/ or if the injured site becomes hot:
20-30 minutes of application every 2-4 hours (Miller, 2014; Wurnig, 2000)
1) Seeing a doctor in order to attain pain and/ or inflammatory medication
1) In conjunction with oral medication, the physician may give a steroid(glucocorticoid) and local anesthetic mixture via injection to reduce swelling and pain ( Wurnig, 2000)
Acute Phase
1) She should try to not lie on the affected side to augment the impingement; and possibly use a pillow to support the shoulder.
1) Maria may also want to see a physiotherapist in parallel to other treatments (galvanization and infiltration therapy) ( Miller, 2014;
Wuring, 2000).
The acute phase is designed to decrease the pain by reducing/ eliminating movement that could further exacerbate the condition.
Once the pain is in control , Maria is able to go into the rehabilitation/ exercise phase.
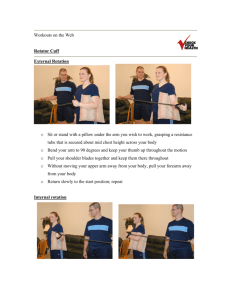
Pectoralis minor self-stretch
Unilateral corner stretch
1.
Abduct arm 90 degrees; flex elbow 90 degrees; externally rotate arm
2.
Place palm on a flat vertical surface
3.
Rotate trunk away from elevated arm
4.
Hold stretch
(Borstad & Ludewig, 2006)
Actions of pectoralis minor:
• protract scapula
• depress scapula
• downward rotation of scapula
Levator scapulae self-stretch
3.
4.
5.
1.
2.
Stretch technique for left levator scapulae
6.
Sit upright and stabilize core —tighten back and abs
Reach behind with right hand and grab side of wheelchair
Slightly lean upper body to the left
Rotate your head 45 degrees to the left
Place your left hand on the back of your head and gently pull it down in the direction you are facing
Hold stretch http://www.humankinetics.com/excerpts/excerpts/levator-scapulaestretch
Levator scapulae actions:
•
Elevates scapula
• Downwardly rotates scapula
• Retracts scapula
Lower Trapezius
• Grade 2:
• laying prone with arms by side
• retract and depress scapula
• move each into the contralateral pant pocket
• Grade 3:
• sitting with arms by side
• moving arm into extension to contralateral pant pocket
• Grade 4:
• sitting with arms by side
• moving arm into contralateral extension
• resistance band, dumbbells
• Grade 5:
• Maria should be able to perform movements with the muscle at a grade 4 level and then move into the functional exercises (refer to functional exercises)
Serratus Anterior
• Grade 2:
• place arm in horizontal protracted position
• place hand on a ball on a table and roll the ball forward and back
• Note the table height should be below 90 degrees due to pain while lifting arm above
90 degrees
• Grade 3:
• supine upward scapular punch
• shoulders horizontally flexed at 45 degrees & elbows flexed at 45 degrees
• Grade 4:
• scapular punch
• shoulders horizontally flexed at 45 degrees & elbows flexed at 45 degrees
• with resistance band
• Grade 5:
• Maria should be able to perform movements with the muscle at a grade 4 level and then move into the functional exercises (refer to functional exercises)
Infraspinatus & Teres Minor
•
Grade 2:
• externally rotating arm at shoulder
• on table with forearm flexed at elbow
• Grade 3:
• laying on side
• external rotation of arm at shoulder with forearm flexed at elbow
• Grade 4:
• prone horizontal abduction of arm at shoulder thumbs up
• flex forearm at elbow progression to extended forearm
• pulling on a resistance band or holding dumbbells
• Grade 5:
• Maria should be able to perform movements with the muscle at a grade 4 level and then move into the functional exercises (refer to functional exercises)
Supraspinatus
• Grade 2:
• laying in prone abducting arm with thumbs up (full can) to about 30 degrees - progress to about
120 degrees
• activating retracting scapula muscles
• begin with forearm flexed at elbow to reduce lever arm - progress to forearm extended
•
Grade 3:
• scaption with thumbs up (full can) abducting arm to about 30 degrees - progress to about 120 degrees
• activating retracting scapula muscles
• forearm flexed at elbow to reduce lever arm - progress to forearm extended moving ball up and down wall
• Grade 4:
• scaption with thumbs up (full can) abducting arm to about 30 degrees - progress to about 120 degrees, activating retracting scapula muscles with dumbbells
• progressively increasing weight
•
Grade 5:
• Maria should be able to perform movements with the muscle at a grade 4 level and then move into the functional exercises (refer to functional exercises)
Functional Movements
•
Scaption
• sitting with arms above 120 degrees externally rotated and thumbs up (full can)
• with resistance band or dumbbells
•
Flexion
• sitting with arms above 120 degrees externally rotated and thumbs up (full can)
• with resistance band or dumbbells
Objective:
1) Look at Maria’s background/ history and at the symptoms she is presenting
2) The potential causes and structures involved in producing these symptoms
3) A design of a rehabilitation intervention for the symptoms/ conditions : includes exercises and preventative techniques)
4) Solutions/ modifications/ activities that could alleviate and prevent the symptoms
a) Acute Phase Modifications
● Pain/ inflammatory management
ice treatment (20-30 minutes every 2 to 4 hours)
-heat application- used after inflammatory stage.
● Electric wheelchair
● Kitchen reorganization
● Reach extender
b) Chronic Phase Modifications
● Kitchen renovation focused on accessibility and smooth navigation
● Re-introduce manual wheelchair gradually with technique monitored
● Analyze office ergonomics a) Desk height b) Degree of side to side reaching needed c) Amount of overhead reaching
● Analyzing manual chair ergonomics a) Components of the chair b) Frame and wheel quality c) Seat and wheel height
Activities
1. These activities are to be done once she has completed the acute treatment phase
----Adapted physical activities such as swimming, stretching, yoga, and meditation.
Modified horseback riding if interested.
2. Social events that will help to focus on the mental and psychological state
----Spending time with family and friends, taking part in social events at work, making new friends in her building.
References
Berg, K. (2011). Prescriptive stretching. Champaign, IL: Human Kinetics
Borstad, J. D., & Ludewig, P. M. (2006). Comparison of three stretches for the pectoralis minor muscle.
Journal of Shoulder and Elbow Surgery, 15 (3), 324-
330..doi:10.1016/j.jse.2005.08.011
Cooper, R.A., & Boninger, M.L.( 1998). Heavy handed: Repetitive strain injury among manual wheelchair users.
Escamilla, R. F., Yamashiro, K., Paulos, L., & Andrews, J. R. (2009). Shoulder muscle activity and function in common shoulder rehabilitation exercises.
Sports Medicine, 39 (8), 663-
663. doi:10.2165/00007256-200939080-00004
Ha, S., Kwon, O., Cynn, H., Lee, W., Park, K., Kim, S., & Jung, D. (2012). Comparison of electromyographic activity of the lower trapezius and serratus anterior muscle in different arm-lifting scapular posterior tilt exercises.
Physical Therapy in Sport : Official Journal of the Association of Chartered Physiotherapists in Sports Medicine, 13 (4), 227. doi:10.1016/j.ptsp.2011.11.002
Kuhn, J. E. (2009). Exercise in the treatment of rotator cuff impingement: A systematic review and a synthesized evidence-based rehabilitation protocol.
Journal of Shoulder and
Elbow Surgery, 18 (1), 138-160.
doi: http://dx.doi.org.ezproxy.library.uvic.ca/10.1016/j.jse.2008.06.004
Labriola, J. E., Lee, T. Q., Debski, R. E., & McMahon, P. J. (2005). Stability and instability of the glenohumeral joint: The role of shoulder muscles.
Journal of Shoulder and Elbow
Surgery, 14 (1, Supplement), S32-S38. doi: http://dx.doi.org/10.1016/j.jse.2004.09.014
Lippert, L., 1942. (2011). Clinical kinesiology and anatomy. Philadelphia, PA: F.A. Davis. Loudon, J.K, Manske, R.C., & Reiman, M.P. (2013). Clinical mechanics in kinesiology.
Champaign, IL: Human Kinetics
Miller, J. (2014). Shoulder Impingement . Retrieved October 13th, 2014, from http://physioworks.com.au/injuries-conditions-1/rotator-cuff-impingement
Page, P. (2011). Shoulder muscle imbalance and subacromial impingement syndrome in overhead athletes. International journal of sports physical therapy , 6 (1), 51.
Spiegl, U. J., Warth, R. J., & Millett, P. J. (2014). Symptomatic internal impingement of the shoulder in overhead athletes.
Sports Medicine and Arthroscopy Review, 22 (2), 120-129. doi:10.1097/JSA.0000000000000017
Wurnig, C. (2000). Shoulder impingement.
Der Orthopäde, 29 (10), 868.