Finding balance: Preventing Medication
advertisement

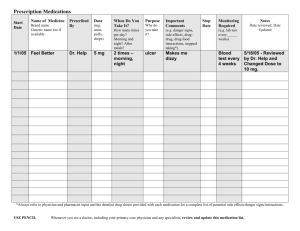
+ Finding Balance: Preventing Medication Related Falls Through Appropriate Medication Use Chanel F. Agness, PharmD, Certified Geriatric Pharmacist cagness@rx.umaryland.edu Stephanie Callinan, PharmD, Geriatric Pharmacy Resident scallinan@rx.umarylande.edu + Session Objectives High Risk Medications in Older Adults • Review age-related changes and medication properties that increase the risk of falls in older adults • Describe potential adverse effects of at least 2 classes of medications associated with falls in older adults. Medication Review Process • Assess medication-related fall risk and recommend fall prevention strategies + High Risk Medications in Older Adults + How the Body Processes a Drug A: Absorption D: Distribution M: Metabolism E: Elimination + Age Related Changes in Distribution Decrease in total body water Monitor water soluble medications Digoxin, lithium Body fat increases and lean muscle mass decreases Lipophilic medications have a longer half life in older adults Long acting benzodiazepines (Diazepam) + Age Related Changes in Metabolism Reduced liver size and decreased blood flow to liver Liver metabolic enzymes function adequately even in the very old + Age Related Changes in Elimination Decline in kidney function Medications that are eliminated through the kidneys can accumulate Morphine Glyburide Digoxin Many others + High Risk Medications in Older Adults Medication classes commonly implicated in falls: Sedative/hypnotics Antipsychotics Antidepressants Anticholinergics Cardiac medications Pain medications Anticonvulsants Older adults are at increased risk of experiencing medication adverse events, including falls related to changes in drug processing in the body. + Sedative/Hypnotics Possible adverse events • Cognitive impairment, delirium, sedation Examples • Non-benzodiazepine hypnotics: • Zolpidem, Eszopiclone, Zaleplon • Benzodiazepines: • Diazepam, Clonazepam, Alprazolam, Lorazepam + Antipsychotics Possible adverse events • Ataxia, impaired psychomotor function, and syncope • Olanzapine can cause orthostatic hypotension Examples • Haloperidol, Olanzapine, Quetiapine, Aripiprazole + Antidepressants Possible adverse events • Ataxia, impaired psychomotor function, and syncope Examples • Fluoxetine, Sertraline, Citalopram, Paroxetine + Anticholinergics Possible adverse events • Sedation, confusion, hypotension, delirium Examples • Tricyclic Antidepressants: • Amitriptyline, Nortriptyline • OTC Antihistamines: • Diphenhydramine, Chlorpheniramine, Hydroxyzine + Cardiac Medications Possible adverse events • Hypotension, dizziness Examples • Beta blockers • Nitrates • Diuretics • Digoxin + BPH/Urinary Retention Medications Possible adverse events • Orthostatic hypotension Examples • Terazosin, Doxazosin, Prazosin + Pain Medications Possible adverse events • Dizziness, syncope, CNS depression Examples • Opioids: • Morphine, Hydromorphone, Fentanyl, Oxycodone + Anticonvulsants Possible adverse events • Ataxia, impaired psychomotor function, syncope Examples • Gabapentin, Levetiracetam, Phenytoin, Valproate + Summary Age related changes in drug disposition can increase older adults risk of falls Several classes of medications increase the risk of falls and should be used cautiously in older adults. + Medication Review Process + Medication Review Process • Medication Reconciliation • Adherence Medication Review Assess Fall Risk • “Red Flag Medications” • Optimize Regimen • Education Fall Prevention + Medication Review Process Up to date medication list/Adherence Identify potentially inappropriate “Red flag” medications Fall Prevention Strategies/Education + Medication Reconciliation: Up to Date Medication List/Adherence Medicines and You: A guide for older adults. http://www.fda.gov/Drugs/ResourcesForYou/ucm163959.htm + Medication Review Process Up to date medication list/Adherence Identify potentially inappropriate “Red flag” medications Fall Prevention Strategies/Education + AGS Beers Criteria Classifies “potentially inappropriate” medications in older adults by: Table 1 • Organ system/Category of Drugs Table 2 • Disease or Syndrome (by organ) Table 3 • Specific drugs, use with caution AGS Beers Criteria for potentially inappropriate medication use in older adults. American Geriatrics Society. http://www.americangeriatrics.org/files/documents/beers/PrintableBeersPocketCard.pdf 3I: Medication/Fall Risk Score Point Value Medicine Class Potential side effects 3 (High) Analgesics/opiates, antipsychotics, anticonvulsants, benzodiazepines, nonbenzodiazepine sedatives*, hypoglycemics* Sedation, dizziness, postural disturbances, altered gait and balance, impaired cognition 2 (Medium) Antihypertensives, cardiac drugs/antiarrhythmics, antidepressants Induced orthostasis, confusion, poor health status 1 (Low) Diuretics Increased ambulation, induced orthostasis Score > 6 Higher risk for fall, medication fall risk evaluation Tool 3I: Medication fall risk score and evaluation tools. Agency for healthcare research and quality. http://www.ahrq.gov/professionals/systems/long-term-care/resources/injuries/fallpxtoolkit/fallpxtk-tool3i.html 3I: Medication/Fall Risk Score Point Value Medicine Class Potential side effects 3 (High) Analgesics/opiates, antipsychotics, anticonvulsants, benzodiazepines, nonbenzodiazepine sedatives*, hypoglycemics* Sedation, dizziness, postural disturbances, altered gait and balance, impaired cognition 2 (Medium) Antihypertensives, cardiac drugs/antiarrhythmics, antidepressants Induced orthostasis, confusion, poor health status 1 (Low) Diuretics Increased ambulation, induced orthostasis Score > 6 Higher risk for fall, medication fall risk evaluation Tool 3I: Medication fall risk score and evaluation tools. Agency for healthcare research and quality. http://www.ahrq.gov/professionals/systems/long-term-care/resources/injuries/fallpxtoolkit/fallpxtk-tool3i.html + Medication Review Process Up to date medication list/Adherence Potentially inappropriate “Red flag” medications Fall Prevention Strategies/Education Evidence-Based Fall Prevention Strategies Summary of the updated American Geriatrics Society/British Geriatrics Society clinical practice guideline for prevention of falls in older persons. J Am Geriatr Soc. 2011;59(1):148-157. Consumer Education Vitamin D Supplementation Minimize use of high risk medications Medication Review Intervention approaches to medications implicated in falls Medication Approach Psychoactive medications Carefully evaluate need and consider tapering or discontinuance as possible by 10-25% of dose per week. Goal – minimize total psychoactive load, use for shortest period of time, taper to avoid adverse withdrawal effects Benzodiazepines/ First-line: sleep hygiene, behavioral intervention Non-benzodiazepine Nonprescription: melatonin? sedative hypnotics Manage underlying causes of insominia Goal – lowest effective dose “intermittently” or “short term” 2 to 4 weeks; taper to prevent rebound insomnia Cooper JW, Burfield AH. Medication interventions for fall prevention in the older adult. J Am Pharm Assoc(2003). 2009;49(3):e70-82 Kamel Insomnia in the elderly: Cause, approach, and treatment. Am J Med 2006 119, 463-469 Intervention approaches to medications implicated in falls Medication Approach Antidepressants Avoid older agents (eg. Tricyclics); use lower doses of newer SSRIs Opiod analgesics Acetaminophen preferred agent for mild-moderate pain (max 3grams/day) Consider topical route for localized pain (eg. topical NSAIDs) Goal – Use lowest effective dose with careful titration/monitoring to manage pain AND limit adverse effects Antihistamines Use non-sedating agents if chronic need (eg. loratadine) Avoid older, more sedating agents (ie. diphenhydramine, chlorpheniramine) Cooper JW, Burfield AH. Medication interventions for fall prevention in the older adult. J Am Pharm Assoc(2003). 2009;49(3):e70-82 + Vitamin D Supplementation Cochrane Review – vitamin D supplementation reduces risk of falls in older adults with clinically low vitamin D levels1 U.S. Preventive Services Task Force (USPSTF) recommends 800 units of vitamin D daily2 Diet, Multivitamin, nutritional supplements, vitamin D supplement, prescription agents Include in medication review and monitor for proper adherence – risk of over treatment and under treatment 1. Gillespie L, Robertson M, GIllespie W, et al. Interventions for preventing falls in older people living in the community. Cochrane database of systematic reviews (Online). 2013;Issue 9. Art. No.: CD007146:8/25/14. 2. U.S. Preventive Services Task Force. Vitamin D and calcium supplementation to prevent fractures, topic page. http://www.uspreventiveservicestaskforce.org/uspstf/uspsvitd.html. + Consumer Education Resources New Drug Facts Label Ten Medicines to Avoid STEADI Toolkit The New Drug Facts Label The new over-the-counter medicine label. http://www.fda.gov/downloads/Drugs/ResourcesForYou/Consumers/ BuyingUsingMedicineSafely/UnderstandingOver-the-CounterMedicines/UCM349215.pdf Medications and Older Adults. www.healthinaging.org + CDC’s evidence-based fall prevention toolkit for healthcare providers and consumer education ASK patients if they’ve fallen in the past year, feel unsteady, or worry about falling. REVIEW medications and stop, switch, or reduce the dose of prescriptions that increase fall risk. RECOMMEND Vitamin D supplements of at least 800 IU/day with calcium. Centers for Disease Control and Prevention, National Center for Injury Prevention and Control, Division of Unintentional Injury Prevention. Stopping elderly accidents, deaths, & injuries tool kit. http://www.cdc.gov/homeandrecreationalsafety/Falls/steadi/about.html. Use medication review process and tools to evaluate fall risk Work with team to manage underlying conditions/medications and maximize use of nonpharmacologic strategies Use high risk medications with caution at the lowest effective dose for the shortest period of time. Provide ongoing education to patients about safe medication use + Helpful Websites/Resources STEADI (Stopping elderly accidents, deaths & injuries) Toolkit for health care providers http://www.cdc.gov/homeandrecreationalsafety/Falls/steadi/index.html Tool 3I: Medication fall risk score and evaluation tools http://www.ahrq.gov/professionals/systems/long-termcare/resources/injuries/fallpxtoolkit/fallpxtk-tool3i.html Beers List Pocket Card, App: iGeriatrics http://www.americangeriatrics.org/files/documents/beers/PrintableBeersPocketCar d.pdf The new over-the-counter medicine label http://www.fda.gov/downloads/Drugs/ResourcesForYou/Consumers/BuyingUsingM edicineSafely/UnderstandingOver-the-CounterMedicines/UCM349215.pdf Medicines and Older Adults. HealthinAging.org www.healthinaging.org + What is one strategy or tool that you can use to prevent falls and promote safe medication use in your practice?