iodine prophylaxis: Increased incidence of papillary cancer
advertisement

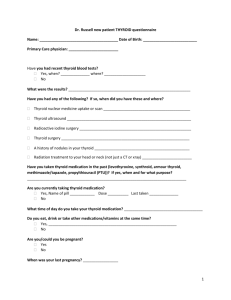
Histological profile of thyroid cancer between 1975-2009.Chernobyl effect and universal iodine fortification of salt THYROID CANCER EVOLUTION OF THE DISEASE EVALUATED IN ONE SETTING VOICHIŢA MOGOŞ1. EUGEN TIRCOVEANU2 1. Clinic of Endocrinology, 1st Surgery Clinici University of Medicine and Pharmacy “Gr.T Popa” Iasi PURPOSE To evaluate the evolution in time of incidence, clinical and histological profile in our setting from 1975 to 2009 taking into account two main events: • The accident from Chernobyl • The role of iodine prophylaxis Data from literature • There was noticed a steady increase of thyroid cancer all over the world • External irradiation in the only well documented cause in papillary thyroid cancer leading to RET/PTC re-arrangements • Iodine deficiency may play a role in the development of follicular cancer and may favor the development of anaplastic carcinoma • Iodine repletion is associated with increased incidence of papillary carcinoma with excellent prognosis There was noticed a steady increase of thyroid cancer all over the world Davies L et al. JAMA 2006, 295, 2164-2167 Between 1973-2002: • 2.4 times increase in thyroid cancer incidence • All thyroid cancer: 3.6/105 to 8.7/105/year (with 5.1/105) • Papillary cancer: 2.7/105 to 7.7/105/year • Small papillary cancer account for 87 % of the cancer • Mortality decreased from 0.57 to 0.47/105/year – External irradiation stopped after 1961 – Most data show that precocious diagnosis by ultrasound and FNB leads to increased incidence but stable mortality – Papillary cancer has a long evolution and excellent survival – Over diagnosis increased the number of radical surgery and its complications Davies L., Welch HG.JAMA 2006,295, 2164-2167 Davies L., Welch HG.JAMA 2006,295, 2164-2167 There was noticed a steady increase of thyroid cancer all over the world Schottenfeld D et al. CA Cancer J.Clin. 1978, 28, 66-86 USA:Connecticut Tumor registry • 1949-1969: 1.4/105/year to 1970-1983: 4/105/year – Papillary: 64 % – Follicular: 18 % – Medullary: 3 % • New York a study on autopsies: – 16.4 /1000 all study – 19.6/1000 in women – 10.4/1000 in men • Microcarcinomas: – USA: 1- 5.7 % – Japan: 17.9-24% There was noticed a steady increase of thyroid cancer all over the world Scheiden P.et al. BMC Cancer 2006, 6, 102-109 Evaluation in an European country – Luxembourg 30 years after Chernobyl in 2 cohorts: 1990-1994 (a) and 1995-1999 (b) • 310 new cases out of which 124 microcarcinomas < 1cm. After 1997 • Increased microcarcinomas from 7 % to 16.6 % – – – • • • 46.5 % papillary 13.3 % follicular 27.3 % medullary Increased incidence from 6.4 to 8.6/105/year Increased incidence in women from 7.4 to 10.1/105/year Increased incidence in men from 2.3 to 3.6 /105/year Mahoney MC et al. Int.Epidemiol. 2005, 34, 714-722 (1970-2001) • Severe exposure: increase incidence in males + 775%, in females:+1925% • Low exposure: increased incidence in males:+54 %, in females: + 250 % Luxembourg Scheider R et al. BMC Cancer 2006, 6, 102-116 There was noticed a steady increase of thyroid cancer all over the world Leehardt L et al. Thyroid 2004, 14, 1056-1060 • FRANCE: 1998-2001 • Increased incidence of thyroid cancer • Increased prevalence of cancer operated among thyroid nodules submitted to surgery due to • increased assessment with ultrasound from 3 to 84 5 • Increased assessment through FNB from 8 to 36 % • In France there was notice no association between cancer incidence and nuclear accident from Chernobyl There was noticed a steady increase of thyroid cancer all over the world Reynolds RM et al. Clin.Endocrinol. (Oxf) 2005, 62, 156-162 Scotish Cancer Registry 1960-2000: • Incresed incidence of thyroid cancer from 1.76 to 3.54/105/year in women • Increased incidence from 0.82 to 1.25/105/year in men • Decreased mortality from 1.05 to 0.28 % in women and from 0.73 to 0.34 in men • Decreased follicular cancer • Stable incidence of medullary carcinoma • Increased survival External irradiation was the only well documented cause in papillary thyroid cancer leading to RET/PTC rearrangements Data from internal irradiation are related to the best studied nuclear plant accident from Chernobyl Thyroid irradiation The role of external irradiation in induction of thyroid cancer was first noticed by Duffy and Fitzgerald in 1953, in those who received external irradiation for different diseases. 36 % of children who developed thyroid cancer had neck irradiation in their personal history The role of radioiodine was largely studied after Chernobyl Contamination: • Internal irradiation by inhalation or ingestion of: radioactive iodine 131I, 132I, 135I, 131mTe (tellurium). 133 Te • External irradiation X ray, gamma Irradiation due to radioactive material deposits on the ground1 • Belarus: cancer in children: 1/106 before and 100/106 after Chernobyl2. The risk in children less than 1 year is 30 fold greater3 Cardis E et al. J.Natl.Cancer Inst. 2005, 97, 724-732 Nagatachi S et al. Thyroid 2002, 12, 899-896 Boltze C et al. Oncology 2009, 22, 459-467 Thyroid irradiation Questions: • Which is the role of the previous iodine intake in the contaminated area • Which are the factors that modify the risk of thyroid cancer after exposure to irradiation: – contamination level – individual factors Total dose of exposure: – 365 mGy in Belarus (7- 3109 mGy) – 40 mGy Rusian Federation (max. 10.2Gy) – Dose of exposure to radioiodine: 1-2 mGy Cardis E et al. J.Natl.Cancer Inst. 2005, 97, 724-732 Thyroid irradiation • The risk to develop thyroid cancer after irradiation in individual who previously consumed stable iodine after an exposure to 1 Gy is reduced 5 fold • Low level of iodine in the soil is correlated with a 3 fold increase of risk to develop cancer compared with residents in areas with naturally more iodine in soil • At doses of contamination between 1.5-2 Gy there is no linear correlation between exposure and risk of cancer • Previously ingestion of iodine reduces radioactive iodine intake • Increased iodine supply reduces thyroid volume and multiplication of thyroid cell and risk of occurrence of mutations Cardis E et al. J.Natl.Cancer Inst. 2005, 97, 724-732 Cardis E et al. J.Natl.Cancer Inst. 2005, 97, 724-732 Cardis E et al. J.Natl.Cancer Inst.2005, 97, 724-732 Thyroid irradiation 1986-1995 in Bellarus 472 patients among which 97.7 were differentiated cancers • median age: les than 14 years • median age at exposure: 4.4 in children and 8.9 in adolescents Italy and France after Chernobyl: 369 patients Mean age in children more than 14 years Follicular cancer: 15.2 % compared with 5.3 % in Bellarus Most effected children were exposed at less than 5 years1 Most cancers occur 5-30 years after irradiation but the risk last to 50 years2 Pacini F. et al. J.Clin.Endocrinol.Metab. 1997, 82, 3563-3569 Greenspan FS JAMA 1977, 237, 2089-2091 Thyroid irradiation Differences among cancers developed after Chernobyl and those developed in Italy1 • Extrathyroidal extension: 49.1% vs 24.9 % • Lymph node involvement: 64% vs 53.9 % • Distant metastasis: 7.8 % vs 17.3 % • For more latent forms of papillary cancer a new pick of incidence may be expected 20 years after Chernobyl accident 5000 cases of thyroid cancer were diagnosed. 60-70 % had N1 and 10-15 had M12 1. Pacini F. et al. J.Clin.Endocrinol.Metab. 1997, 82, 3563-3569 2. Tuttle RM et al. Clin.Oncolocy 2011, 23, 268-275 Relationship between the degree of iodine contamination and number and percentage of new cases of thyroid cancer in children and adolescents after Chernobyl nuclear reactor accident Pacini F et al. J.clin.Endocrinol.Metab. 1997, 82, 3563-3569 Pacini F et al. J.clin.Endocrinol.Metab. 1997, 82, 3563-3569 Iodine deficiency may play a role in the development of follicular cancer and may favor the development of anaplastic carcinoma Iodine and thyroid cancer • The relationship between thyroid cancer and dietary iodine is controversial • There are some data that could demonstrate that iodine deficiency may increase thyroid cancer in some areas • Iodine may act as adjuvant factor for carcinogensis and may have a role in the hystological profile of thyroid cancer • Is obvious from all statistics that increased dietary iodine is associated with an increase of incidence of thyroid cancer1 • Sicilia: – Thyroid malignancies: IDA – 2.96%, ISA 5.48 % – Follicular cancer: IDA; up to 127/105, – Anaplastic cancer: 93/105 1. Knobel M et al. Arq.Bras. Endocrinol.Metab. 2007, 51, 701-712 2. Belfiore A et al. Cancer 1987, 60, 3096-3192 Iodine and thyroid cancer Iodine deficiency is associated with a relative risk (RR) of cancer as follows (Sweden)1 • 0.92 for all histological types • 0.80 for papillary cancer • 0.87 for anaplastic carcinma • 1.98 for follicular cancer The risk for follicular cancer is 1.3-15 in iodine deficient areas and depends of the time of residence in these areas2 1. Petterson B et al. Int.J.Cancer 1996, 65, 13-19 2. Galanti MR et al. Int J.Cancer 1995, 61, 615-621 Iodine and thyroid cancer Frequency of thyroid cancer by tumor type in Salta, Argentina before and after iodine prophylaxis Total number of cases Years after iodine prophylaxis 10 years 59 11-26 85 Papillary 26 46 Follicular 15 15 Anaplastic 9 13 Ratio between Papillary and follicular cancer 1.7 3.1 Harach C et al. Clin.Endocrinol. 1995, 61, 615-621 Iodine and thyroid cancer Histologic pattern of thyroid tumors in two areas of Sicily, Italy with low and adequate iodine intake Total number of cases submitted to surgery Low intake 911 (126) High intake 2437 (419) Papillary 11 103 Follicular 11 27 Anaplastic 5 9 Belfiore A et al. Cancer 1987, 60, 3096-3102 Iodine prophylaxis and thyroid cancer Incidence of different forms of thyroid cancer before and after iodine prophylaxis Papillary: pre prophylaxis 44% vs post prophylaxis: 60 % Papillary/follicular ratio: 1.7/1 to 3.1/1 1 Ratio papillary to follicular cancer according to iodine intake2 IDA: 0.1/1, moderate intake: 1.6/1-3.7/1, high intake: 3.4/1-6.5/1 1986-1999: 1500 new cases: Incidence: 3.86 to 6.08/105 After prophylaxis: papillary to follicular ratio: 5.323 1. Harach H et al. Endocr.Pathiol. 2002, 13, 175-181 2. Lind p et al. Thyroid 1998, 8, 1179-1183 3. Szybinski Z et al. Wiad Lek 2001, 54, 106-116 Iodine prophylaxis and thyroid cancer Incidence of different forms of thyroid cancer before and after iodine prophylaxis 1974-1976 and 1992-1994 • Increased percentage of thyroid cancer on thyroidectomies • Papillary: 54.3 % • Follicular: 27 % • Anaplastic: 11.1 % • Medullary: 4.6 % Papillary to follicular ratio: 1974-1976: 0.60 1992-1994: 6.88 Deandrea M et al. J.Endocriol.Invest. 1997, 20, 52-58 Iodine prophylaxis and thyroid cancer iodine prophylaxis: • Increased incidence of papillary cancer • Decreased incidence of follicular cancer • Decreased incidence of anaplastic cancer • Improved prognosis Histology of thyroid cancer in iodine deficient areas (Algeria) Improvement of socio-econimc status from 1966-1981 and 1982-1991 Bakiri et all.Cancer 1998, 82, 1146-1153 Bakiri et all.Cancer 1998, 82, 1146-1153 Histological profile of thyroid cancers in an iodine sufficient area ( Connecticut - USA ) Schottenfeld D, Gersman ST. Epidemiology of thyroid Cancer 2008 There is a trend to increase the incidence of thyroid cancer as well as an increase of papillary thyroid cancer Burges JR et al.J.Clin. Endocrinol.Metab.2000, 85, 4, 1513-1517 Histology and age are the best predictor factors for survival Scheiden P et al.BMC Cancer 2006, 6, 102-106 5 years survival: • Papillary: 96 % • Follicular: 88.9 % • Medullary: 90.9 % Hundahl Sa et al. Cancer 1998, 83, 2638-2648 10 years survival: • Papillary: 93 % • Follicular: 85 % • Hurthle cell: 76 % • Medullary: 75 % • Anaplastic: 14 % Histology and age are the best predictor factors for survival Passler G et all.Endocrine-Related Cancer 2004,11, 131-139 Radioactive elements release after CHERNOBYL 1986 What happened in Romania? It partially remains in the area of suppositions CONTAMINAREA RADIOACTIVA DUPA CERNOBIL 1986 - ROMANIA RET/PTC in the key mutation seen in radiation-induced thyroid cancer and activation of BRAF is associated with sporadic forms of differentiated thyroid carcinoma Xing s et al Endocrine reviews 2007, 28, 742762 Data from literature • Elisei has demonstrated that clinical and histological profile of thyroid cancers was modified during the last 35 years through: • Increased incidence of papillary cancers from 80,5 % to 91% during these years • Decreased follicular cancers from 19,5 % to 9 %; • Increased incidence of cancer with diameter of less than 1 cm. from 7,9% in the firs half of the interval to 28,7 % in the second • Reduced incidence of macro-invasive cancers from 7 % to 1,9 %; • Reduced incidence of cancers with distant metastases from 5,4 la 2 %; • Reduced incidence of cases with lymph node metastases from 34,2 % to 22, 4%; • Reduced incidence of cases in advanced stages according to TNM VI, for stage III 10,8 to 7,4 % and for stage IV from 4,2% to 1,7 %. Elisei R., et all.J.Clin. Endocrinol.Metab. 2010, MATHERIAL AND METHOD • Data from files of patients with thyroid tumors submitted to surgery between 1975-2009 (35 years) were divided into 5 years intervals and analyzed for: • New cases for each interval • Histology • Clinical appearance • Stage of the disease according to TNM classification and tumor stage grouping TNM VI • Ratio between papillary and follicular cancer as indirect signs for the role of supposed external irradiation and modification due to iodine prophylaxis MATHERIAL AND METHOD • From 1981 most patients were assessed based on fine needle biopsy performed within the Department of Endocrinology of our hospital • Our data were compared with data from the Department of Endocrinology analyzed between 1971 and 2000 for patients admitted in this setting including those operated in other surgery clinics Algorithm of diagnosis for thyroid nodules used after 1981 in the Clinic of Endocriology IASI THYROID NODULE CYST ULTRASOUND SOLID OR MIXED LESSION FNB BENIGN ABC SCINITIGRAPHY FOLLICULAR NEOPLASM MALIGN EVACUAATION, SCLEROZING SOLVED T4 WARM COLD LOW RISK RECURREN CE HIGH RISK THIROIDECTOMY FOLLOW-UP E.Zbranca et.al.Symp.Nat.Endocrinol.1995, Endocrinologie Clinica 1997 EPIDEMIOLOGICAL BACKGROUND Moldova is situated in the northern part of Romania Different studies provided data that show a decrease of prevalence of goiter and a mild to moderate iodine deficiency assessed by urinary iodine determination, except for same areas where urinary iodine is still low Urinary Goiter % Iodine g/dL 1975 Suceava 6.55 60 Botosani 8.62 COUNTY Neamt Iasi <5 9.93 1986 1999 Thyroid ultrasound examination 53.7 33.3 30.4 30.7 22.2 24.7 31.8 16.1 23.4 6.4 Interval Number of cases Age Females Males 1975 - 1979 19 45.7 ± 10.9 18 1 1980 - 1984 18 52.9 ± 14.9 15 3 1985 - 1989 17 49.5 ± 15.6 13 4 1990 - 1994 37 48.6 ± 16.8 32 5 1995 - 1999 52 51.5 ± 15.8 43 9 2000 -2004 71 53.1 ± 15 53 18 2005-2009 131 51.8 ± 14.2 109 22 1975 - 2009 345 51.3 ± 14.8 283 62 Demographic data of patients with thyroid tumors admitted in the Ist Surgery Clinic of Iasi RESULTS: thyroid tumors submitted to surgery between 1975-2009 in the 1st Surgery Clinic of Iasi- 345 cases Mumber of thyroid tumors operated between 19752009 131 140 120 100 80 60 40 20 0 71 52 37 19 18 17 1975- 1980- 1985- 1990- 1995- 2000- 200509 05 99 94 89 84 79 interval New cases of thyroid tumors operated for each 5 years interval in the 1st Surgery clinic of Iasi 140 Nr.of tumors % 120 100 80 60 37.97 40 20 5.5 5.2 4.9 10.72 15.1 20.57 0 1975-79 1980-84 1985-89 1990-94 1995-99 2000-05 2005-09 WHAY WE FOCUSED OUR RESEARCH ON CHANGES OF HYSTOLOGICAL PROFILE OF TUMORS DURING TIME? • Histology, age and stage at diagnosis are the best predictive prognostic factors for thyroid cancers • All these factors are influenced by at least two major events that happen in Romania: • Hypothetical external irradiation after Chernobyl with increase of papillary forms • Important modification of iodine supply due to active and universal salt iodination also with increase of papillary form and decrease of incidence of goiter that may mask a carcinoma Survival in thyroid cancers acording to histology Clinic of Endocirnology Iasi 1993 120 100 80 Papillary Follicular Medullary 60 Anaplastic 40 20 0 0 5 years 10 years 15 years Survival in thyroid cancers acording to age at diagnosis Clinic of Endocrinology Iasi 120 100 80 <45 years 60 > 45 years 40 20 0 0 5 years 10 years 15 years Survival in thyroid cancers acording to tumor staging Clinic of Endocirnology Iasi 120 100 80 Stage Stage Stage Stage 60 40 20 0 0 5 years 10 years 15 years I II III IV Histological profile of thyroid cancers Ist Surgery Clinic Iasi 6.08 21 % Anaplasic 4.05 14 Nr.of cases MTC 4.05 14 Foll less dif 6.66 Other 23 17.97 Foll 62 4.92 17 Pap/Foll 56.23 Papill 0 50 194 100 150 200 250 Cancers derived from follicular epithelium (1st.Surgery Clinic) 100 All 4.32 Anaplasic 4.32 MTC % 7.09 Foll less dif Nr.of cases 19.13 Follicular 5.24 Papil/foll 59.9 Papillary 0 50 100 150 200 250 300 350 Taking into account only cancers derived from follicular epithelium the percentage of papillary and follicular cancers in more obvious among al tumors Others 5.82 Anaplastic 8.7 MTC 6.14 Foll less dif 15.21 Follicular 14.88 23.62 Pap/fol Papilary 25.56 0 5 10 15 20 25 30 Histological profile of thyroid tumors in the Clinic of Endocrinology of Iasi % 1975 - 2000 Expectation after external irradiation and improved iodine supply • Increased incidence of papillary carcinomas in younger age, but the risk after exposure persists long life after exposure • Increased incidence of aggressive forms in children and young adult immediately after irradiation • Normal iodine intake is associated also with increase of papillary cancers with good prognosis even in advanced forms and increased papillary to follicular ratio • Decrease incidence of follicular cancer with a less good prognosis • Decrease incidence of anaplastic carcinoma • Diagnosis made in less advanced stages of the disease Interval Papillary 19751979 21.05 Pap/fol 19801984 19851989 19901994 19951999 20002004 20052009 33.3 23.5 21.6 30.76 61.97 85.5 11.1 11.7 2.7 17.3 2.8 0.8 3.81 Follicular 63.2 44.5 23.5 35.13 25 9.85 Foll less dif. 19.5 11.1 29.4 27.02 5.76 1.4 MTC 5.26 3.84 5.6 3.8 1.92 9.85 1.52 Anaplastic 11.76 13.5 Striking features noticed during the analyzed interval: increase incidence of papillary cancers, decrease of follicular forms, decrease of anaplastic carcinomas – all seems to be related with a better iodine prophylaxis and perhaps to external irradiation due to Tchernobil accident Clinical data of thyroid cancers 1st Surgery Clinic Others MNG+Lym ph node MNG Sol.Nod+ Lym ph node Solitary nodule Anaplastic MTC Foll less dif Follicular Pap/fol Papill 0 10 20 30 40 50 60 70 80 NEW CASES OF THYROID CANCER 1971 – 2000 CLINIC OF ENDOCRINOLOGY IASI 96-2000 80 91-95 55 86-90 87 81-85 46 76-80 29 1971-75 12 0 20 40 60 80 100 70 papillary 60 follicular mixt/pna 50 anaplastic medullary 40 30 20 10 0 solitary.nod SN+lymphnode MNG MNG+L DM Bmet Interval Unilateral tumor 19751979 19801984 19851989 19901994 19951999 20002005 20052009 63.15 94.4 88.23 86.48 86.5 94.4 89.3 Bilateral tumor 36.7 5.6 5.88 13.5 13.4 5.63 10.6 Lymph node involvement 26.3 5.5 35.3 72 42.3 31 22.9 Developed on goiter 52.6 55.5 47.05 71.8 74.46 83 16.7 The trend of thyroid cancer derived from follicular epithelium during 35 years is a slightly reduce of tumors diagnosed in later stages : bilateral, with lymph node involvement. Only in the last 5 years the histology did not reveal surroundings of goiter in the proximity of tumors due to active iodine prophylaxis 1975Interval 1979 19801984 19851989 micro carcinoma 19901994 19951999 20002004 20052009 5.4 4.5 6.25 0.8 TI 31.6 27.8 5.88 18.9 20.45 35.93 34.44 T II 57.9 55.5 58.8 32.4 43.2 26.6 25.6 T III 10.5 16.7 23.5 27.2 29.5 18.8 32.8 11.76 13.5 2.27 12.5 6.4 T IV Tumor staging at time of diagnosis show that after 1990 there were discovered microcarcinomas, stage I tumors increase and stage IV tumors obviously decrease (TNM classification VI) 1975Interval 1979 19801984 19851989 19901994 19951999 20002004 20052009 TI 52.7 44.4 29.4 51.35 43.18 48.43 53.6 T II 47.36 44.4 35.3 24.32 27.3 18.75 24 11.2 23.5 10.8 27.3 26.56 20.8 11.7 13.51 2.2 6.25 1.6 T III T IV Grouping of tumor stage according to histology, tumor extension and age at diagnosis show that after 1990 slightly more tumors were discovered in less advanced stages even through the mean age at diagnosis does not change during the analyzed interval (TNM classification VI) Papillary to follicular ratio an indirect marker of iodine deficiency 1st Surgery Clinic 25 22.6 Pap/foll ratio 20 15 10 5 5.75 0.73 0.8 0.66 0.39 1.56 0 1975-79 1980-84 1985-89 1990-94 1995-99 2000-04 2005-09 Changen in percentage of different forms of thyroid cancers derived of follicular cells 1975-2000 Clinic of Endocrinology Iasi Papillary Follicular 70 MixedFPA 62 60 50 Anaplastic 53.8 47.36 42.1 40 30 25.2 18.5 20 15.9 10.52 11.7 8.6 10 3.4 0 1971-1980 1981-1990 1991-2000 EVOLUTION of RATIO BETWEEN PAPILLARY AND FOLLICULAR CANCER 1971 – 2000 Clinic of Endocrinology Iasi (309 cases) 3.5 3.5 3.14 3 2.5 2.21 1.86 2 1.5 1 1 0.5 0 <1980 1981-85 1986-90 Lind P. 1998: this ratio depends of iodine supply 6,5/1 - 3,8 /1: increased iodine supply; 3,7/1 - 1,6/1: moderate iodine supply 1,6/1 - 1,19/1 iodine deficiency 1991-95 1996-2000 8 7 The ratio between papilary and follicular cancer according to iodine supply in the studied area compared with other reported data*Deandrea 1997, ** Lind 1998 1971-1980 1981-1990 6.88 1991-2000 6.5 6 5 3.7 4 3 2.48 2 1 3.4 2.9 1.78 1.4 0.88 1.7 1.6 0.6 0.19 ly* * * pp su ne or m al io el y er at N di ne in Io d M od io di de f ici c fic ie n de e in cy * cy ** x* ila st pr of Po ro fil ax * Pr ep 82 ia n am D C hi ri cu ta Ia s '84 i 0 CONCLUSIONS Our data on patients with thyroid cancers analyzed over a period of 35 years indicate that: • It is an important increase in each 5 years interval, of number of new cases • There is an important increase of papillary cancer and the ratio between papillary and follicular cancer and a decrease of anaplastic carcinoma • There is increase of cases discovered in earlier stages of the disease • We cannot assume that this events are due to the external irradiation because of lack of genetic and clinical evidence • We believe that the afore mentioned evolution of histological profile of thyroid cancer in our setting is due to a better iodine prophylaxis