File
advertisement

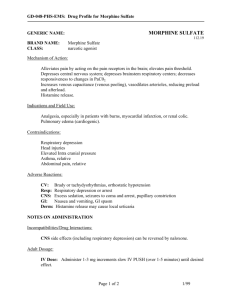
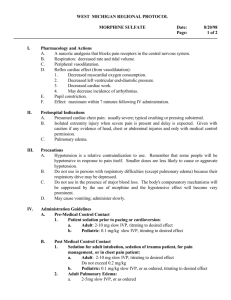
USES OF OPIOIDS IN ANAESTHESIA Mainly used for analgesia ,for both intra-operative & postoperative. As a premedicant. As an inducing agent ( rarely used as it requires very high doses). Blunting cardiovascular response to intubation. Fentanyl is the most commonly used but sufentanil is the agent of choice. For day care surgery (Propofol + Alfentanil is the combination of choice. For painless labor ( Fentanyl + Bupivacaine by epidural route. Pulmonary edema ( Morphine is the agent of choice). Intra-operative myocardial ischemia ( Morphine is used ). To abolish shivering ( Pethidine & Tramadol ). Description Morphine, the most important alkaloid of opium, is classified pharmacologically as a narcotic analgesic. a white crystalline powder, soluble in water. It comes as a generic name – Morphine sulphate. Morphine can be given by IV, IM, subcutaneous, oral , rectal , transcutaneous ,intrathecal & epidural routes. Dose : 0.1- 0.2 mg /kg Mechanism of action Mechanism of action is similar as other opioid drugs as Meperidine. Morphine interacts predominantly with the μreceptor. Morphine produces respiratory depression by direct action on brain stem respiratory centers. Morphine depresses the cough reflex by direct effect on the cough center in the medulla. Morphine causes miosis. Other effects Gastric, biliary, and pancreatic secretions are decreased by morphine. Morphine can cause a marked increase in biliary tract pressure as a result of spasm of sphincter of Oddi. Morphine produces peripheral vasodilation which may result in orthostatic hypotension. Indications and Usage Used in treatment of moderate to severe pain relief. Used in cancer related severe pain. Side effects They include the following major hazards: respiratory depression, apnea, and to a lesser degree, circulatory depression, respiratory arrest, shock, and cardiac arrest. Constipation, lightheadedness, dizziness, sedation, nausea, vomiting, sweating, dysphoria, and euphoria. Urine retention or hesitance, reduced libido and/or potency. Pruritus, urticaria Convulsions Contraindication and Precautions In patients with known hypersensitivity to the drug. In patients with respiratory depression in the absence of resuscitative equipment, and in patients with acute or severe bronchial asthma. Head Injury and Increased Intracranial Pressure. Severe Hypotensive patients. Should be used in pregnant women only when clearly needed. Is not recommended for use in women during and immediately prior to labor. Not used in Breast feeding mothers. Use of morphine has not been evaluated systematically in children. Overdosage Overdosage of morphine is characterized by respiratory depression. Since respiratory arrest may result either through direct depression of the respiratory center, or as the result of hypoxia, primary attention should be given to the establishment of adequate respiratory exchange through provision of a patent airway and institution of assisted, or controlled, ventilation. The narcotic antagonist, naloxone, is a specific antidote. An initial dose of 0.4 mg of naloxone should be administered intravenously, simultaneously with respiratory resuscitation. Naloxone may be repeated at 2 to 3 minute intervals. Meperidine (PETHIDINE) Meperidine hydrochloride is ethyl 1-methyl-4- phenylisonipecotate hydrochloride, a white crystalline substance with a melting point of 186°C to 189°C. It is readily soluble in water and a slightly bitter taste. The solution is not decomposed by a short period of boiling. In foreign countries, it is known as pethidine. Meperidine is not a natural opiate like morphine or codeine, but is a synthetic compound belonging to the phenylpiperidine class. Meperidine is recommended for relief of moderate to severe pain but also has the unique ability to interrupt postoperative shivering and shaking chills Mechanism of action Despite being structurally distinct from morphine and related opiates, meperidine's effects on opiate receptors are similar to those of morphine; both are agonists at mu and kappa receptors. Although the exact physiologic action of opiates is not known, stimulation of opiate receptors ultimately reduces neurotransmitter release. This effect depends on –the receptor it binds,the binding affinity ,and whether the receptor is activated. Cellular mechanism- alterations in Potassium and calcium condutance. Respiration is depressed by a direct effect on the brain stem respiratory center, and the cough center is also suppressed by meperidine. Nausea and vomiting may be induced from direct stimulation of the chemoreceptor trigger zone. Opiate agonists increase smooth muscle tone, which can affect the intestinal, urinary, and biliary tracts. Digestion is delayed by a decrease in gastrointestinal secretions. Some references state that meperidine causes less biliary tract spasm than does morphine. Vasopressin output is stimulated, which can decrease urine output in conjunction with increased tone of the detrusor muscle. Miosis is another characteristic of the opioid analgesics. Compared with morphine, meperidine causes fewer of these effects. INDICATIONS AND USAGE Management of acute pain episodes of moderate to severe in nature. Treatment of Post anesthesia shiverings. Dosage and routes When changing route of administration, note that oral doses are about half as effective as parenteral dose. Oral route not recommended for chronic pain. Oral: Initial: 50 mg every 3-4 hours as needed; usual dosage range: 50-150 mg every 2-4 hours as needed I.M. : Initial: 50-75 mg every 3-4 hours as needed; patients with prior opiate exposure may require higher initial doses; usual dosage range: 50-150 mg every 2-4 hours as needed Preoperatively: 50-100 mg given 30-90 minutes before the beginning of anesthesia Slow I.V.: Initial: 5-10 mg every 5 minutes as needed ADVERSE REACTIONS The major hazards of meperidine, as with other narcotic analgesics, are respiratory depression and, to a lesser degree, circulatory depression; shock, and cardiac arrest have occurred. The most frequently observed adverse reactions include : Dizziness, sedation, nausea, vomiting, and sweating. Other adverse reactions include: Nervous System: Euphoria, dysphoria, weakness, headache, agitation, tremor, uncoordinated muscle movements (e.g. muscle twitches, myoclonus), severe convulsions, hallucinations and disorientation, visual disturbances. Gastrointestinal: Dry mouth, constipation, biliary tract spasm. Cardiovascular: Flushing of the face, tachycardia or bradycardia, palpitation, hypotension ,syncope. Genitourinary: Urinary retention. Allergic: Pruritus, urticaria, other skin rashes, wheal and flare over the vein with intravenous injection. CONTRAINDICATIONS/PRECAUTIONS Meperidine should be used cautiously in patients with pulmonary depression or pulmonary disease such as acute bronchial asthma or upper airway obstruction. Patients with head trauma or with increased intracranial pressure Patients with cardiac disease or hypotension.(vasovagal syncope or orthostatic hypotension) Meperidine should be used with caution in patients with glaucoma(Increase IOP) Pethidine is absolutely contraindicated in patients on monoamine oxidase inhibitors therapy. Severe excitatory responses like restlessness, hypertension,convulsion, coma & death can occur. It should not be given to patients with myocardial ischemia as it depresses the myocardium & by causing tachycardia increases the oxygen demand. Meperidine should be prescribed extremely cautiously, if at all, to patients with renal disease. patients undergoing biliary tract surgery, although meperidine reportedly causes less biliary tract spasm than does morphine. Meperidine readily crosses the placenta and normally should not be given during pregnancy. OVERDOSAGE Primary attention should be given to the reestablishment of adequate respiratory exchange through provision of a patent airway and institution of assisted or controlled ventilation. The narcotic antagonist, naloxone hydrochloride, is a specific antidote against respiratory depression which may result from overdosage or unusual sensitivity to narcotics, including meperidine. Therefore, an appropriate dose of this antagonist should be administered, preferably by the intravenous route, simultaneously with efforts at respiratory resuscitation. Oxygen, intravenous fluids, vasopressors, and other supportive measures should be employed as indicated.