Gas Prices on the Rise….
Misty Ellis, MSN, APRN
2015 Annual SPCS Conference
Disclosure Statement
I do not have any relevant financial
relationships with any commercial
interests to disclose.
Pulmonary Hypertension
Definition
Elevation in pulmonary artery pressures (PAP) and
pulmonary vascular resistance (PVR)
Systolic pulmonary arterial pressure >35 mm Hg or a
mean PAP >25 mm Hg
Often we compare the PAP to the systemic blood
pressure; if the systolic PAP is >1/2 the systemic blood
pressure, the patient is at higher risk for a pulmonary
hypertensive event crisis
*Simple definition: elevated BP in the lungs*
Suesaowalak, et al, 2010
Pulmonary Hypertension
Pathophysiology
Endothelial cell dysfunction creates increased vascular
tone and pulmonary artery vasoconstriction
Increased pulmonary venous pressure may be due to
mitral valve disease, left ventricular systolic or diastolic
dysfunction
Increased pulmonary blood flow through the
pulmonary vasculature may be due to congenital heart
defects with left-to-right shunt
Hazinski, 2013
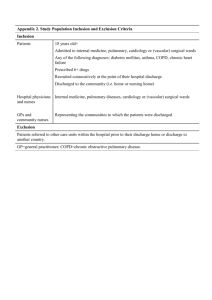
Pulmonary Hypertension
Event vs Crisis
Condition
PHT Event
PHT Crisis
Definition
Acute rise in PAP but stable BP
Acute event in which PAP systolic
pressures match or exceed systemic
pressures, causing RV failure and a
fall in LA preload and systemic
hypotension
HR
Increased
Increased; late bradycardia
BP
Stable
Decreased
O2 sats
Decreased or Stable
Cyanotic
CVP / RT atrial pressure
Stable or slightly Increased
Increased
LA pressure
Stable
Decreased to increased as
LV end diastolic pressure
rises
Lactic Acid
Normal
>2.0
Perfusion
Decreased
Severely decreased
Hazinski, 2013
Pulmonary Hypertension
Epidemiology
Incidence of congenital heart disease is approximately
8/1,000 live births
It is estimated that 3 million children worldwide are at
risk for the development of pulmonary vascular
disease due to congenital heart disease.
Adatia, et al, 2010)
Question: What patient would you
anticipate to be most at risk for pulmonary
hypertension post operatively?
A. 1 year s/p ASD repair
B. 5 day old s/p CoA repair
C. 4 month old Down’s Syndrome
boy s/p CAVC repair
Pulmonary Hypertension
At Risk Populations
Congenital heart disease
Highest risk- cyanotic lesions with increased pulmonary blood flow at
high pressure (ex. Truncus Arteriosus)
Lesions with increased pulmonary blood flow at high pressure
without cyanosis (ex. Unrestrictive VSD, large PDA)
Pulmonary venous outflow obstruction (ex. Mitral stenosis
pulmonary vein obstruction (TAPVR), cor traiatriatum)
Neonates in first 2-6 weeks of life are still transitioning from fetal
circulation ie. Elevated pulmonary venous pressure
Premature infants with bronchopulmonary dysplasia
Children with abnormal pulmonary reactivity (ex. Trisomy 21)
Suesaowalak, et al, 2010
Pulmonary Hypertension
Most common anatomic lesions and conditions associated
with PH after surgical repair and Cardiopulmonary bypass
Unrestrictive VSD in children > 6 months
AVC in children > 6 months
TAPVR in infants < 8 weeks old
TAPVR with obstruction
Truncus arteriosus
Cardiac transplantation
Did your patient have a pre-op cardiac catheterization?
PVR?
> 3 Wood
units concern
for PHT
Checchia, P. et al. 2011
Date of download: 6/1/2015
Copyright © American College of Chest Physicians. All rights reserved.
From: Pulmonary Arterial Hypertension: Baseline Characteristics From the REVEAL Registry
Chest. 2010;137(2):376-387. doi:10.1378/chest.09-1140
Epidemiology of
PHT
Figure Legend:
World Health Organization (WHO) Group I pulmonary arterial hypertension classification of REVEAL patients at enrollment. (A) WHO
Group I PAH classification. (B) Breakdown of associated pulmonary arterial hypertension subgroup. APAH = associated PAH; CHD
= congenital heart disease; CVD/CTD = collagen vascular disease/connective tissuedisease; FPAH = familial PAH; HT =
hypertension; IPAH = idiopathic PAH; PAH = pulmonary arterial hypertension; PCH = pulmonary capillary hemangiomatosis; PPHN
= pulmonary hypertension of the newborn; PVOD = pulmonary venoocclusive disease; REVEAL = Registry to EValuate Early And
Long-term PAH disease management.
Management of Post operative
PHT
• First is ..Prevention!
• Anticipate the patients that are at risk for PHT
• Avoid the following in high risks patients
• Hypoxia
• Acidosis
• Hypoventilation
• Endotracheal Suctioning
• Second.. Encourage factors that LOWER PVR by pulmonary
vasodilation
• Oxygen
• Alkalosis / Hypocarbia
• Sedation: Fentanyl
• Normal FRC
• Nitric Oxide
Nitric Oxide
• What is it?
• Endogenous gaseous cell mediator involved in
neurotransmission, inflammatory cell activation, and
vascular smooth muscle relation
• Therapeutically, inhaled NO (iNO) is a Selective
Pulmonary Vasodilator
• Enhances V/Q matching
• Treats pulmonary arteriolar hypertension (PPHN in
newborn babies)
• Reduces pulmonary vascular resistance and right
ventricular cardiac work ie.. Post op heart patients
Nitric Oxide
Pharmacology
• Nitric oxide activates guanylyl cyclase
(GC)
• GC takes GTP and turns it into cGMP
• Increase in cGMP activates to cellular
signaling pathways which lead to
DECREASE in intracellular calcium
levels
• Decreased calcium leads to smooth
muscle relation and pulmonary
arteriolar vasodilation
**potent pulmonary vasodilator without systemic vasodilatory
effect**
Googleimages.com
Nitric Oxide
• Delivery Method
• Intubated patients
• Can be delivered to non-intubated patients with a
tight-fitting face mask or nasal cannula
• Injected directly into the inspiratory limb of the
ventilator circuit in synchrony with each inspiratory
breath
• Half- life is only 15-30 seconds so, to ensure flow is not
interrupted in the event of a disconnected ventilator, a
separate connector is used to facilitate iNO delivery via
a manual bag system
Nitric Oxide
• Dosing
• Doses between 5 and 20 ppm should produce
a clinically apparent response in oxygenation
or pulmonary vascular resistance
• Doses > 40 ppm do not produce greater
benefit and it puts patients at greater risk for
methemoglobinemia and raises levels of
nitrogen dioxide
Suesaowalak, et al, 2010
Nitric Oxide
• Complications
• Methemoglobinemia
• A condition in which the iron within hemoglobin is oxidized from the
Fe2+ state to the Fe3+ state
• Iron needs to be in the Fe2+ state to allow hemoglobin to bind
oxygen
• Methemoglbinemia results in cyanosis because the Hgb can’t bind
oxygen
• Methemoglobin > 10% results in clinical cyanosis
• Rebound PHTN
• Typically occurs when weaning the final 5 ppm
• Associated with elevation of PA pressure, difficulty with ventilation,
severe hypoxia, and cardiovascular instability
Nitric Oxide
• Rebound HTN Mechanism
• iNO actually leads to down regulation of guanalyl
cyclase so stopping iNO causes acute reduction in
cGMP levels, an increase in intracellular calcium and
can lead to pulmonary arteriolar vasoconstriction until
cGMP levels become naturally replete (over a few
hours)
• There is also a reduced production of endogenous NO
during iNO administration
Nitric Oxide
• Rebound PHT Prevention
• Slow weaning of nitric oxide may ameliorate rebound
PHTN
• Evidence shows progressive rebound of symptoms can
occur if patient has had long-term treatment with iNO
• Slow weaning can be done with a weaning protocol
Nitric Oxide: Protocol
• Why have a protocol?
• Determine if the patient is a responder or not
• This prevents use of potentially dangerous or
expensive drug on patients who will no benefit
• Utilize the drug only when it is needed
• Reduces practice variation
• Limit costs attributable to unnecessary use of nitric
U gotta be
oxide
kidding
• At our institution it costs $175 / 30 minutes
me!$!$
Simsic ,et al 2014
Nitric Oxide: Protocol
Nitric Oxide: Protocol
Barr, et al, 2010
Nitric Oxide: Protocol
• Key Components
• Avoid metabolic & respiratory acidosis
• If the patient becomes unstable at any time notify
MD/NP to evaluate
• Be proactive in asking / using the Protocols
• RN to avoid doing other “things” during the weaning
process or doing any unnecessary suctioning
• Do not wean FiO2 during weaning
• The most critical time in weaning iNO is the last 5ppm,
can potentially see rebound PHT during this weaning
phase
Summary
• CHD lesions that predispose children to PHT are: VSD,
PDA, ASD, truncus arteriosus, TAPVR and AVC
• Be prepared; know the pre-op cath data
• Clinical s/s PHT: HR, CVP, BP, O2 sats,
perfusion
• One management strategy for PHT is to start iNO
• Use iNO to ensure the patient really benefits from it,
reduce provider practice variation, and reduce cost
References
• Adatia, I., Kothari, S., & Feinstein, J. (2010). Pulmonary Hypertension Associated with
Congenital Heart Disease. Pulmonary Vascular Disease: The Global Perspective. CHEST
137(6) (Supple):52S-61S.
• Barr, F., & Macrae, D. (2010). Inhaled Nitric Oxide and Related Therapies. Pediatr Crit
Care Med 11 (2 Suppl): S30-S36.
• Checchia, P., Bronicki, R., & Goldstein, B. (2012). Review of Inhaled Nitric Oxide in the
Pediatric Cardiac Surgery Setting. Pediatr Cardiol 33:493-505
• Simsic, J., Harrison S., Evans, L., et al. (2014). Reducing Variation in the Use of Inhaled
Nitric Oxide. Pediatrics 133: 31753-e1758
• Hazinski, M.F. (2013). Pulmonary Hypertension. In Nursing Care of the Critically Ill
Child. (3rd ed.) (pp265-273). St. Louis, Missouri: Mosby Elsevier.
• Tzanetos, D.T., Housley, J., et al. (2015). Implementation of an Inhaled Nitric Oxide
Protocol Decreases Direct Cost Associated With Its Use. Respiratory Care 60(5) 64450.