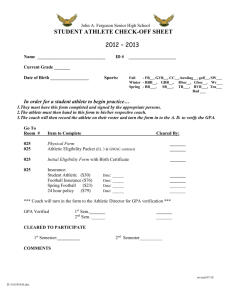
Introduction To Athletic Training
advertisement

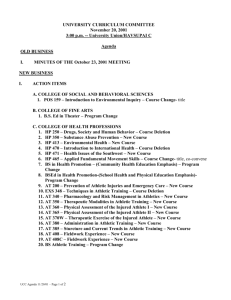
James W. Robinson Athletic Training Program 2013-2014 Nottingham Athletic Training Center Room 535 Robinson Athletic Training Staff Jeff Perry, MS, VATL, ATC jgperry@fcps.edu • Office: 703-426-6818 • Cell: 703-932-1950 Deb Cassidy, VATL, ATC dkcassidy@fcps.edu Karen Conboy, MS, VATL,ATC keconboy@fcps.edu Have both numbers and Email addresses saved. Robinson Athletic Training Support Staff Team Physicians: Dr. Marc Childress, Family/Sports Medicine, DeWitt), Dr. Matt Levine, Orthopedics/ER, INOVA Fairfax GMU AT Student Intern:Sandy Tanloet JWR Student Aides: Giselle C., Idil Y., Hope O., Alsiha C., Tyler H. Related Acronyms • • • • • • • • • • • • • • • • AED AT ATC ATC/ATR ATP DO Dx EAP ECC LNP MD OTC PA PPE Rx Tx automated external defibrillator athletic trainer certified athletic trainer (not to be used as a noun) athletic training center/room athletic training program doctor of osteopathic diagnosis emergency action plan emergency care card licensed nurse practitioner medical doctor over-the-counter physician assistant pre-participation physical exam or “physical” prescription treatment Athletic Trainer Responsibilities • Prevention of injuries/ re-injury • Recognition, evaluation, and assessment of injuries and conditions resulting • Immediate care of injuries • Rehabilitation and reconditioning of injuries • Organization and administration • Professional development and responsibility • Visit www.nata.org for more information Coach as First Responder Sports First AID and CPR Course • To be completed once--during first year of coaching in FCPS. Register on-line and www.fcps.edu/coach complete online portion before course date: • January • February 12 McLean • June 23rd Woodson HS • Concussion Education for Coaches info on concussion slide below. Athletic Trainer Coverage Athletic Training Room Coverage • The Athletic Trainer will be available for treatments, rehabilitation, and questions from parents / physicians each school day afternoon. • Fall Hours: 12:30 to 7 PM or end of game. Treatment and rehab before and/or after practice. Note: ATC at FB practice during live contact drills and play. • Winter Hours: 12:30 to 8 PM, later on Home Game/Event nights. Weekends: if scheduled Home Events. • Spring Hours: 12:30 to 7 PM, or end of games. ATC available for treatment and rehab before and after practice. • Note: athletic training meetings are on Wednesday’s and may cause delay in opening AT Center later than 12:30. Athletic Event Coverage An Athletic Trainer is present at all contests below. Please consider that an athletic trainer has to be on site when scheduling or re-scheduling events (scrimmages, regular and post games)-especially on weekends and vacation periods. FALL • • • • • WINTER • Wrestling Football, home & away, • Boys and Girls Basketball (all levels) all levels • Gymnastics Field Hockey • Indoor Track Meets (shared) Volleyball • Swim/Dive Playoffs Cross Country meets Spring (shared with FCPS ATCs) • Lacrosse • Soccer Cheer Competitions • Baseball and Softball (on-site, unless only • • • event) Track & Field Meets Tennis (on site), Crew regattas (shared) Please let Athletic Trainer know if ice, supplies, or evaluation of athlete will be needed before your “post-game” team meeting. Athletic Trainer Coverage—Travel, Camps & Tournaments • Utilize the AT for injury evaluations and acute care when possible. Help make the connection of AT to parent of our injured athlete if they are available. • Camps: Since a “standard of care” has been established in FCPS, any team camp should be covered by an AT if game like situations are involved. Same for away games, tournaments, etc. • If you host a tournament on vacation periods, outside of normal schedule, or as a fundraiser, the athletic trainer is paid from the same funds as the officials. If officials paid by school, then AT is not paid. If officials paid by individual sport or booster club, then AT is paid. Usually equivalent of $30/hour. See a Robinson AT for help in arranging AT coverage at least one month in advance. Assumption Of Risk • • • • Participation in any sport presents risk Not all injuries can be prevented Catastrophic injuries can occur in any sport Comprehensive Athletic Training Program care has proven to influence a reduction in injuries and severity of injury. This needs to be presented to parents. You can add it to any preseason team information you give them. Physicals: Correct form? (“Revised March 2013” top left, with VHSL logo, routing box) Exam date after May 1, 2013 and signed and stamped by an MD, DO, PA, or CNP/LNP ONLY Appropriate “Cleared” box checked Completed with insurance company name and parent signatures on page 2, and two places bottom page 4. Physical is good until June 30 of current school year PPE’s at Robinson are scheduled each June. This year June 10, 2014. This is a fundraiser for rams boosters for $50 donations. Encourage getting PPE early for summer conditioning. Check AT website for updates. If you know a medical professional (MD, PA , LNP, EMT, RN, PT, AT) that may want to volunteer, please have them contact us. EMERGENCY CARE CARDS All students participating in athletics must complete the FCPS Emergency Care Information Form. The coach of each sport must have a copy of every athlete’s emergency care card at all practices and competitions. Coaches are advised to keep the emergency care forms in a waterproof container. The athletic trainer, DSA, or another school administrator may keep the second copy. The athletic trainer reviews this form and notes any pertinent information such as allergies, previous injuries, and medical conditions that may be a problem during athletic participation. In the event there is a change in the medical status of an athlete during the school year, (recent diagnosis of asthma for example), a revised emergency care card is required and all appropriate personnel (ATC, Coach, DSA) must be made aware of the changes. The FCPS Emergency Care Card is available to download from the web at: http://www.fcps.edu/DIT/forms/se3.pdf Medications • If an athlete has a systemic condition that requires the use of an inhaler, EpiPen, glucagon, etc., the athlete must have that device at practice or game or not participate. • If any of your athletes requires emergency medication, make yourself familiar with its use. • If an athlete’s health status changes during the course of the season (Dx with asthma, mono, etc.) please notify us as soon as possible. • Discourage the use of OTC pain medications before or during competition. Emergency Action Plan Considerations • EMS should be notified of any upcoming home events • EMS should be familiar with/have directions to the location of the event (including entrances to fields, closest gate to field/doors to gymnasiums/weight room/training room) This information should be coordinated with the 1st and 2nd responding EMS Stations to the school during the first few weeks of school year. • Emergency Care Cards for each athlete MUST BE READILY AVAILABLE for EACH practice and contest, and should include: – Family phone numbers (home/work/cell) – Who to contact if parent/guardian is unavailable. – Any medical alerts (allergies, diabetes, single paired organs) • Emergency plans should be reviewed prior to each season (or school year) for each location in use during that season (or school year) • Write it down. It must be designed with regards to your specific sport, practice locations, and unique situations (i.e. camps), and discussed with entire coaching staff prior to 1st practice. • Inquire about appropriate care/standard of care at camps, tournaments, etc. that your team may attend. To avoid liability a comparable standard of care should be available at away camp or tournament. (i.e.: at least an AT on site as you would have at home event). School: _____________________________________________ Date: ______________ Coach: ________________________________ Sport: ___________________ Contact Number ___________ Game Site Street Address: __________________________________________________________ Specific directions to game site from nearest major intersection: ______________________________ ________________________________________________________________________________ Practice Site Street Address: ________________________________________________________ Specific directions to practice site from nearest major intersection: ___________________________ ________________________________________________________________________________ Directions. Please complete and distribute a copy to all members of your coaching staff, the athletic administrator and ATC. Discuss this plan with your coaching staff. Proper preparation can lead to quick, appropriate action. ______________________________ Where should EMS come to have quick access to the injured athlete? _______________________________ Who will give primary care to the athlete? _______________________________ _______________________________ Where is the first aid kit? Where are the emergency care cards? _______________________________ _______________________________ _______________________________ Who calls EMS? From which cell phone/telephone will the call to EMS be made? Who will notify the parents that the athlete is being transported to an emergency care facility? _______________________________ _______________________________ _______________________________ _______________________________ Who will open any gates or doors for EMS? Who will meet EMS and direct them to the injured athlete? Who will travel with the injured athlete to the emergency care facility? To which emergency care facility will athletes be transported? _______________________________ _______________________________ Who will notify the ATC? Who will manage the rest of the team while care is given to the injured athlete? _______________________________ _______________________________ _______________________________ Who will follow-up with the parents? Who will document the injury? Who will speak to parent in the instance of catastrophic injury? Emergency Telephone Numbers EMS __________________ Certified Athletic Trainer __________________ Emergency Care Facility _______________ Athletic Administrator _____________________ OFF CAMPUS PRACTICE GUIDELINES • • • • • • • • • • • • • • • Due to limitations on the number of practice facilities available at each school, FCPS athletic teams are often forced to conduct practices at sites away from the high school campus. Use this as a guide in developing an emergency action plan to ensure a safe practice environment. Identify means of communication in case of an emergency. Land line, cell phone, radio, etc. Ensure there will be access to this communication device at any time during your practice. Know where AED is, nearby building. Loaner AED is available from ATC as needed. Memorize the exact street address of your practice location, as well as nearby landmarks that would aid an ambulance in finding your location quickly and efficiently. Have a properly developed emergency care plan Identify individuals to “flag down” the ambulance in the event of a 911 call. Anticipate from which direction the ambulance would be arriving. Ensure that every athlete’s emergency care card is readily available at each practice and competition. Identify an individual to retrieve the card if needed. Remember that the head coach is often not able to search for the Emergency Care Card as they must stay with the athlete. Ensure the practice field is free from any natural or artificial hazards: power pole support lines, broken glass, metal spikes, etc. Have readily available a well-stocked first aid kit equipped to handle “typical” sports injuries. Keep abreast of current practices in first aid care through regular communication with your school’s athletic training staff. Remember that each coach is required to successfully complete Sports First Aid Course. Be aware of and prepared to deal with potentially infectious bodily fluids, especially blood. Have readily accessible adequate materials to properly handle these fluids. Follow the procedures outlined in “Universal Precautions”, available from your school’s athletic trainers. Inform your school’s athletic trainer of any and all injuries incurred by your athletes within 24 hours. Have an adequate amount of ice available for the treatment of acute injuries. Ensure drinking water is available and accessible to all athletes at all times during practice. Abide by FCPS Inclement Weather and Heat Guidelines. Have all approved emergency medications (Epi-Pen, inhalers, etc.) readily available for indicated athletes. Emergency Plan Flow Chart Injury Coach (no AT present) Athletic Trainer Present Medical Emergency? Parent notification Coaches Notified Non-Emergency EAP or Provide First Responder Care AT Follow up Activate EMS (911) Physician Referral if needed Notify parents Note from MD AT Evaluation Rehab Program Initiated Coach Who Calls? Phone access? Meet EMS ECC available? Notify Parents Physician Referral? ATC Rehab Program Initiated as needed Coach Return To Practice/Play Coach Injury Prevention As a coach, you probably have more influence and ability to prevent injuries than anyone else. Some tips and things to think about: 1. Facilities: scan area you practice or play in before each session to look for potential hazards left behind by others (objects, standing water, etc.). 2. Equipment: in good condition? Is it being used properly? (Headgear worn in wrestling practice? Helmet on for BP? Warming up or practice without protective eyewear? e.g.) 3. Strength and Conditioning: Every sport. Provide opportunities and teach proper techniques. Age and skill level appropriate. Gradual increase. Encourage them to get in shape to play sport--as opposed to playing to get in shape as young “athletes” often do. 4. Encourage proper nutrition and hydration. (provide adequate time to hydrate during practices) 5. Recognize signs of dehydration, heat illness, and concussion 6. Encourage proper rest/sleep. (Provide enough rest between sessions—2+ hours rec.) 7. Be aware of athletes or team becoming fatigued (i.e. “dead-legs,” unfocused) or stale 8. Recognize injury or overuse patterns (unusual number of… “shin splint” problems in your sport? ankle sprains? ACL sprains? concussions? Infections? ), then… 9. …Do something about it. Consult with and utilize the athletic trainers. (For example: Can you incorporate ACL or ankle sprain prevention exercises into your team warm-up?) 10. What else? ___________________________________________________ When Injury Does Happen You can assist your athlete by encouraging them to… … Immediately Breathe! Help to relax, calm down … Later..Accept responsibility, this happened to you! … report injury if not obvious, … be compliant with treatment plan, … stay involved with team … … … … … Approach the injury as a challenge Keep a POSITIVE attitude Be compliant with treatment or rehab plan Set Goals, (work with AT and Coaches) Ask Questions By understanding the injury and what to expect, the athlete will feel less anxiety and a greater sense of control, which does enhance the healing process ACUTE INJURY TREATMENT RICES The immediate care of any sprain, strain, or contusion (bruise) is the same. Please adhere to the following guidelines and apply “RICES” to help prevent further injury or discomfort. R = Rest - Sometimes there is no substitute for it--allow the injured area to begin the healing process. This may take one to 10 days, depending on the severity of the injury. I = Ice - after the initial evaluation, apply ice for 20 minutes. During the next 72 hours (minimum), apply ice for 20 minutes or soak the injured body part in ice water for 10 minutes, no more than five (5) times per day. Apply no heat to the injury during the first 72 hours after the injury has occurred. C = Compression - apply a “snug” elastic wrap around the injured body part, being careful not to cut off circulation. Advise not to wear elastic wraps overnight, but keep the injured body part elevated above the heart. E = Elevation - keep the body part above the level of the heart whenever possible. For example, with an ankle sprain, raise the bottom of the bed 8-12 inches by placing an object between the mattress and the box spring, under the foot area. S = Support - support the injured body part if possible (crutches, brace, splint, sling, etc.). Note: heat application of any kind is not advisable for a recent (acute) injury. Injury Reporting • • • • • • • • • • All injuries must be reported to the school athletic training staff asap. Injuries that cause any time loss from sports participation must be reevaluated by the school athletic training staff prior to returning to activity. Report every injury or illness occurring on your team to the athletic training staff Please do not assume the AT was notified by athlete or parent If AT is not immediately available please email or leave a phone message. The athletic trainer must also evaluate athletes that are unable to participate in practice or competition due to injury or illness regardless of doctor intervention. When an athlete is restricted from participation by a physician, the physician AND the AT must clear athlete before they can return to participation. Our goal is to return athletes as soon as possible. Recommendations on participation status and modification of activity will be provided. Return to play decisions are based on evaluation and functional testing by the ATC, and when appropriate, input from athlete, parents, coach, physician, and team physicians. Follow AT recommendations to prevent re-injury or prolong healing process, and avoid taking on that liability. When to see the doctor? When injury occurs a referral to a MD is warranted when: • Signs and symptoms indicate probable fracture, • Possible fracture or complication • 2nd or 3rd degree sprain (pain level, amount or swelling, degree of laxity, loss of function, etc.) • When reasonable progress is not made with rest and conservative treatment • Unexplained symptoms, uncertainty, athlete disposition • When mom or dad say so! Medical Referrals • It is best if coaches do not refer kids to a doctor or say things like “you have to see a doctor.” • At the same time, do not discourage athlete or parent from seeing a physician if that’s what they already plan to do. (i.e. While you may suggest they see us first, Please do not say they “must” see athletic trainer first). • Physicians – If athlete goes or are referred by us, they should bring our “Response Form” to their appointment, or bring in a note from doctor that informs us of diagnosis, what rehab or treatment the physician would like, and playing status. • If do visit MD, PT, chiropractor, acupuncturist, etc., Let us know! Bring our form to appointment so we may better communicate with other healthcare professional. Care by Third Parties • “In no event shall the medical care of an athlete within Fairfax County Public Schools facilities involve the manipulation, massage, diagnosis or adjustment of an injury or condition without the approval of a member of the Sports Medicine Team.” –FCPS Risk Management Athletic Trainer—Athlete meetings Athletes need to meet with ATC before each season to go over Local ATP, VHSL Policy, and State Law in the following areas: 1. Following AT Center Rules 2. AT Philosophy and Expectations of Athletes 3. Reporting Injury and Illnesses 4. Available treatments/therapy 5. Treatment Cards—Note to away AT 6. Hygiene. Proper cleaning habits; uniform and equipment care disinfecting, water bottles 7. MRSA etc., Video and “Communicable Diseases and Info Sheet,” etc. 8. Importance of proper nutrition, hydration and heat related illnesses, and sleep 9. Supplements and Steroids ( VHSL Video/Facts plus FCPS Policy) 10. Concussion: Updates, Clarifications, management protocol, etc., ImPACT, concussion testing for athletes, schedule all freshmen & juniors for baseline testing, also test students new to school, or if recent concussion, takes 30 minutes to test a group of 25 to 30. Other: for Coaches Each team should have a first aid kit with them during games and practices in the absence of an AT. Sign out kits or get yours restocked in the training room. Familiarize yourself with contents and read directions if necessary. Please don’t leave in hot or cold car as this can quickly ruin supplies. Return first aid kits and coolers at end of season. Clean and store coolers/bottles in TEAM Storage rooms during season. Enlist managers, water boys, or athletes to get water ready for practice or games--including visitors as well. AT will assist. Return ice chests daily Please don’t borrow items or equipment from the athletic training room without asking FCPS Exposure Control Plan and Training Coaches are required to complete training and have documentation on file with FCPS Office of Risk Management. VHSL rules indicate that there will be blood clean–up supplies at every contest; Coaches will be responsible for clean up of blood spills on equipment and uniforms. Please use gloves on both hands to avoid the school getting an OSHA fine Rehabilitation and Taping • Athletes are better served if they are provided a specific rehabilitation program, which may or may not include the application of tape as short-term additional support. • Tape or brace? If athlete is using it, they should also be doing Rehab daily. Be prepared each day to work towards getting better and not needing to rely on taping/brace. • Coaches should not tape injured athletes—even if you are good at it! • We stock some braces for convenience and resale to athletes at cost • We have the tools and time to work with athletes on daily basis • Coordinate with ATC and each athlete when best time is to perform rehab-before during, or after practice Return To Play • Parent, Coach, Family Physician, Athlete, Administrator, ATC, or Team Physician can exclude an athlete from participation. • All 7 of these individuals must agree that the athlete can and should play • The role of the Athletic Trainer is also to make sure athlete is safe to return to play. AT must “clear” athlete to play regardless if doctor has also “cleared” you. PRE-GAME SEVERE WEATHER ANNOUNCEMENT This announcement should be read over the public address system at the beginning of each contest when the National Weather Service (NWS) predicts the possibility of thunder/lightning in your area, and/or when local conditions indicate severe weather is possible. The announcement should be repeated at the first indication of thunder or lightning in the distance. Announcement Local forecasts indicate a potential for thunder & lightning storms for this area. In the event the presence of lightning causes a delay in this athletic contest, it will be requested that you exit the stadium in an orderly fashion, and seek shelter inside the school building. All spectators and players should seek safe shelter within the school building at that time. The contest will resume 30 minutes after the last evidence of ground to cloud lightning, please remain in the school until that time. Clear The Area Order FCPS Lightning Guidelines indicate when the decision has been made by the designated individual to suspend the contest due to lightning, the following clear-the-area order shall be read: DUE TO LIGHTNING IN THE AREA, ALL INDIVIDUALS SHOULD RELOCATE TO AN AREA INSIDE THE SCHOOL BUILDING, IN AN ORDERLY FASHION, AT THIS TIME. (Repeat as necessary) WET BULB TEMPERATURE RECOMMENDATIONS Level FWBT Duration Attire 1 Less than 60° 2 hours Full gear 2 2 hours Full gear 3 60.1° 65.9° 66° - 74.9° 2 hours Full gear 4 75° - 76.9° 2 hours, every 45 minutes of work > 15 minutes of rest each hour Remove helmets unless active in drill 5 77° - 78.9° 2 hours, every 45 minutes of work > 15 minutes of rest each hour 6 79° - 80.9° 7 81° - up Fluid Consumption Recommendations Insist that adequate water be ingested Insist that adequate water be ingested Never restrict water consumption Provide minimum of 2 water breaks per hour Insist that 4 - 6 oz minimum water be ingested every 20 minutes Insist that 6 – 8 oz minimum water be ingested every 20 minutes Provide minimum of 3 water breaks per hour Remove protective equipment for non-contact drills Insist that 8 – 10 oz minimum water be ingested every 15 minutes Remove helmet unless active in drill, remove pads (i.e., shoulder pads) when teaching or non-contact portions of practice exceed 10 minutes in length 2 hours, every 45 minutes of work > 15 minutes of rest each hour Shirt, shorts only. Remove helmets, pads and other equipment Insist that 8 – 10 oz water be ingested every 15 minutes. Reduce intensity of activity, no equipment or helmets NO OUTDOOR PRACTICE The Heat Policy also applies to indoor practice Re-hydrate 24 oz for every pound of body weight lost per day. Follow the Heat Policy for practices conducted indoors Remove helmet unless active in drill RED ALERT DAYS - When the Council of Governments (COG) issues a RED ALERT all outside athletic activities will be suspended between 11 am and 6 pm unless the air quality improves. RECOMMENDATIONS: Replace fluids at a rate of 24 fluid ounces for every pound of body weight lost after exercise. Encourage athletes to wear light colored, loose clothing during activity in hot weather. Encourage athletes to wear sunscreen on exposed skin during hot, sunny conditions. Make readily available an adequate fluid supply to athletes at all times during activity in hot weather. Recommend replacement of sodium (sports drinks, salty foods) if dehydrated, or with activity over multiple days of heat stress conditions Discourage athletes from taking caffeine, energy, and/or dietary supplements such as ephedra containing products as they may cause an increase in dehydration and heat related illness and/or injury. The following athletes are at increased risk for heat related illness/injury and should be monitored closely or placed on a modified participation schedule •Individuals poorly acclimatized, overweight, or poorly conditioned •Athletes having a pre-existing dehydrated state (recent fever or gastro-intestinal illness) or pre-existing heat injury •Athletes taking certain medications including diuretics, antihistamines, beta blockers and anticolinergics •Overweight athletes Nutrition Nutrition should be a priority Breakfast / Lunch / Dinner EAT ALL THREE! Eat Good Calories, AVOID JUNK FOOD! 60-70% CHO, 20-25% K, 10-15% Fat Sodium Helps avoid cramping Sprinkle extra table salt on food Eat a small bag of pretzels before practice Proper Hydration is essential --Top choices Good ol’ H2O (WATER), 64 Gatorade / Sports Drinks Chocolate Milk oz per day! Nutrition + • Adequate Sleep is also essential for athletic performance • There is no quick fix…real food is far better than pills or supplements Supplements : • are often not recommended for under 18 • are NOT regulated, therefore may be impure, and contain ephedra, steroids, e.g. • Don’t make expensive URINE! ENERGY DRINKS ARE BANNED by the VHSL This is only a Partial List: Any new product sold as an energy or performance enhancer is banned Steroids • Signs and Symptoms: Severe Acne, mood swings, aggression, depression, very fast strength gains, change in physical characteristics, organ damage, and others. • Unlawful: • The consequences for being caught using steroids is 2 years disqualification from sports. (Virginia state law) • Are Banned by VHSL, NFHS, NCAA, USOC • Side Effects are Unappealing and Unhealthy (Can be even be Deadly) • Don’t confuse Steroids with supplements or “corticosteroids” Hygiene • Clean Practice Clothes Daily • Clean and Disinfect Gym Bag(s) or Item(s) You Use to Carry Shoes & Practice Clothes • Wash Hands Often(Use Hibiclens if available) • Avoid touching face, eyes • Shower After Practices & Games • Do NOT Share Towels or Personal Hygiene Items • Report All Cuts, Abrasions or Any lesion that Concerns You to the Athletic Trainer and/or your Doctor Immediately • All Cuts, Scrapes, Abrasions or Any lesion of Concern MUST be Covered and Cleaned Before Practice • Use ALL of your Rx Meds. Throw away expired meds. • Keep Finger Nails Trimmed Play Safe and Clean: How to prevent the spread of communicable and infectious diseases in secondary school sports Immediately shower after each practice or competition. Wash all athletic clothing worn during practice or competition daily. Clean and disinfect gym bags and/or travel bags, if the athlete is carrying dirty workout gear home to be washed and then bringing clean gear back to school in the same bag (note: this problem can also be prevented by using disposable bags for practice laundry). Wash athletic gear (such as knee or elbow pads) periodically and hang to dry. Clean and disinfect protective equipment such as helmets, shoulder pads, catcher’s equipment and hockey goalie equipment regularly Do not share towels or personal hygiene products with others. All skin lesions should be covered before practice or competition to prevent risk of infection to the wound and transmission of illness to other participants; only infections that have been properly diagnosed and treated may be covered to allow participation of any kind. All new skin lesions occurring during practice or competition should be properly diagnosed and treated immediately. Playing fields should be inspected regularly for foreign objects and debris that could cause cuts or abrasions, and for animal droppings that could cause bacterial infections of cuts or abrasions. Athletic lockers should be sanitized between seasons. Rather than carpeting, locker or dressing rooms should have tile floors that can not only be cleaned, but also sanitized. Wrestling and gymnastics mats should be sanitized daily. Weight room equipment – including benches, bars and handles – should be cleaned and sanitized daily. Water Bottles 101 • Bring a case of water bottles with you to away games as not all schools will have cups available • Teach How to properly drink out of a Gatorade Bottle: Do not touch the cap with your mouth or hands! Squeeze the Green part of the bottle to dispense fluid. Place bottle back in the Orange carrying tray. Please Don’t Waste Cups when available MRSA: What Is It? • Methicillin-Resistant Staphylococcus Aureus • Form of “Staph” Infection that does not respond to common antibiotics • Approximately 25-30% of healthy people may carry staph aureus, and only 1% carry MRSA • MRSA is Treatable! • Early recognition and treatment is important MRSA: What Does It Look Like? Mild infections may look like a pimple or boil and can be red, swollen, painful, or have pus or other drainage and are usually mildly infectious and easily treated. More serious infections may cause pneumonia, bloodstream infections, or surgical wound infections. Prevention of Skin Infections ☺ Treat Uniforms with Anti-Microbial detergent “FabricAide,” Mats and equipment with SurfaceAideXL (See AT to arrange this) Encourage Proper Hygiene Washing hands frequently Using alcohol based hand gel when sink is not available is a good practice Clean equipment (helmets, headgear, pads) regularly (i.e. daily) LysolR, Clorox AnywhereR, or 100:1 diluted Bleach Do not share personal clothes or items Wear clean practice and game clothes Shower soon as possible after participation Any skin lesions must be evaluated by the ATC Wash and dry thoroughly any soiled clothes or linens that may have contacted infected area Perform routine skin checks to catch skin conditions as early as possible Skin Lesion and Participation? • Protect your team, remove the athlete with suspect lesion from participation • Immediately refer the athlete to the AT • Do not allow an athlete to participate with a wound that is not covered-whether it is infected or not • Maintain confidentiality – Encourage your athletes not to “talk too much,” to avoid rumors about who may have an infection or skin disorder Return to Play • The athlete’s return to play status will be determined by the ATC in consultation with the parent and treating physician. • Having an infection does not necessarily mean the athlete will be excluded from participation for an extended period of time. Information sheet to hand out to athletes This form along with others can be found on athletic training web page as well. It does not need to be signed and turned in as in past since we added this to concussion ed. presentation. FCPS Athletic Training Program Communicable Disease Information Sheet Because most sports involve both physical contact and shared equipment and facilities, athletes have an increased risk of contracting a communicable disease, particularly a skin infection. Transmission of disease and skin infection can be minimized when athletes take part in diligent and proper hygiene practices. Skin infections include, but are not limited to, ringworm (fungal infection), staphylococcus including MRSA and impetigo (bacterial infections), herpes (viral infections), and conjunctivitis (pink eye). Most skin infections are treatable by a health care professional, although some forms of skin infections can not be cured. Following the guidelines below will reduce the potential for contracting a communicable disease: All athletes should shower with soap and water immediately following practices or competitions. Athletes should not share clothes, towels, soap, razors, etc. Sports equipment in direct contact with skin (helmets, headgear, etc.) should be cleaned and sanitized after each use using a bleach solution mixed daily or a commercial EPA-approved product. All clothes worn during practice and competition should be washed daily. All towels should be washed daily. Athletes should carefully and thoroughly inspect all areas of their bodies for lesions or signs of skin disorders daily. This includes the entire scalp area in sports such as wrestling. Lesions that are identified during self-inspection are to be brought immediately to the attention of the coach and the school’s certified athletic trainer. Athletes with skin infections must follow the direction of the certified athletic trainer regarding participation in practices and competition. ---cut and retain the top portion, return lower portion signed to the certified athletic trainer--- Complete the portion below and return it to the certified athletic training staff at your school. The undersigned understand and accept the risk of the skin infections associated with participation in sports. We agree to follow the guidelines provided regarding practicing good hygiene and reporting all lesions to the certified athletic trainer. ________________________________ Printed name of student athlete Sport you will participate in this season: ________________________________ Signature of student athlete ____________________________________ ________________________________ Printed name of parent or guardian ________________________________ Signature of parent or guardian Date_______________ MRSA Video http://www.google.com/url?sa=t&rct=j&q=mrsa%20video&source=web&cd=9&ved=0CFkQFjAI&url=http%3A%2F%2Fw ww.hibiclens.com%2Fmrsa_video%2Findex.html&ei=m1rFTrO2ITq0gHEh5nfDg&usg=AFQjCNFXNbeBGc7RDVJIxmben7iPr5Li_g What Was The Main Message In The Fight Against MRSA? Concussions • • • • A concussions is an injury to the brain Concussions can alter a student’s ability to learn Concussions can be life threatening Signs & Symptoms include: Headache, confusion, dizziness, change in personality, difficulty sleeping, difficulty concentrating, loss of appetite, loss of memory, and many others. • Treatment is REST and hydration. Other treatments may be used for cases of prolonged recovery • Parents and students need to complete concussion education each year to comply with state law. www.fcps.edu/sports • Coaches need to review concussion education course each school year before season. Either course below is acceptable. – http://brain101.orcasinc.com/4000/ – http://www.nfhslearn.com/electiveDetail.aspx?courseID=15000 – Print certificate for DSA • Concussion Management Tool • ImPACT baseline testing helps monitor safe RTP • Obtain Baseline Results (for all Freshmen & Juniors, new students, concussion previous year) • Retest if Injury Occurs • Video (9 min) students watch • http://web1.ncaa.org/web_video/health_and_safet y/concussion/concussion.html HEAD INJURY FOLLOW-UP This is a follow-up sheet for the health and safety of your child. Quite often significant signs and symptoms of a head injury do not appear for several hours following the injury. This fact sheet is to alert you to those signs and symptoms that may not be readily apparent, but may materialize over time. DO NOT give your child aspirin, Tylenol, Advil, etc following a head injury unless directed to do so by a physician. • • • • • • • • • • • • • • • • • • • • • If any of the following signs or symptoms become WORSE over time, please contact a physician immediately. Difficulty remembering recent events or meaningful facts Severe headache Stiffening of the neck Mental confusion or feeling of strangeness Nausea Irritability Changes in emotional status/mood swings Dizziness, poor balance, or unsteadiness Abnormal drowsiness or sleepiness Loss of appetite Continued ringing in the ears Slurring of speech If any of the following appear, contact Emergency Medical Services immediately. Blood or yellowish/clear fluid from nose or ears Vomiting Alterations in breathing patterns Double or blurred vision, photophobia Convulsions or seizures Weakness in either arm or leg Unequal pupils or uncontrolled eye movements Have healthy season. Good luck! If you have any questions or need assistance please Visit the Athletic Training Center Thank you. Visit the Robinson Athletic Training Page or FCPS ATP for more information. www.robinsonathletics.com or www.fcps.edu/sports