Click here to read her PowerPoint presentation
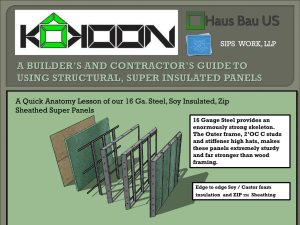
advertisement

Soy-based Infant Formula: Concerns and Recommendations Suha Khoury, RD Purpose of Presentation To explore safety issues related to the use of soy-based infant formula as the main source of nutrition To present international regulations on the appropriate use of soy-based infant formula Topics of Discussion 1. Historical background 2. Safety issues and potential adverse effects 3. Views of regulatory bodies 1. Historical Background1 1909 First use of soy-based infant formula 1929 Soy-based formula was proposed for intolerance of cow’s milk Mid 1960’s Soy protein isolate (SPI) used instead of soy flour Early 1970’s Supplementation of soy-based formula with Lmethionine 1. American Academy of Pediatrics Policy Statement, Pediatrics, 1998 2. Safety Issues and Potential Adverse Effects 2.1. Nutritional adequacy 2.2. Presence of phytoestrogens 2.3. Presence of potential carcinogens 2.4. Aluminum content 2.5. Manganese content 2.6. Allergicinity of soy 2.7. The use of genetically modified (GM) soy protein isolate (SPI) 2.1. Nutritional Adequacy 2.1.1. Presence of soy phytates 2.1.2. Presence of protease inhibitors 2.1.3. Other nutritional factors 2.1.1. Soy Phytates Soybean contains highest phytic acid content of all legumes 1 “…soy protein isolate formulas still contain 1.5% phytates” 2 Phytates affect absorption of following minerals: Calcium & Phosphorous: Until 1980, “mineral absorption from soy formulas was erratic” partly due to “the presence of excessive soy phytates in the formula” 2 30% phosphorus bound to phytates2 3,4,5 Soy infant formula may result in decreased bone mineralization Zinc: Absorption highest (41%) from human milk, lowest (14%) from soy formula 6,7 Manganese: Absorption doubled after dephytinizing formula8 Iron: bioavailability by removing phytic acid9 Copper: copper absorption and status by phytate content7 Vitamins: Use of SPI requirements for vitamins E, K, D & B1210 1. Chitra U et al, Plant Foods Hum Nutr, 1995 2. American Academy of Pediatrics Policy Statement, Pediatrics, 1998 3. Steichen et al, J Pediatr, 1987 4. Chan et al, Am J Dis Child, 1987 5. Hillman et al, J Pediatr, 1988 6. Sandstrom et al, Am J Dis Child, 1983 7. Lönnerdal B et al, Am J Clin Nutr, 1999 8. Davidsson L et al, Am J Clin Nutr, 1995 9. Davidsson L et al ,Pediatr Res, 1994 10. Rackis J, J Am Oil Chem Soc, 1974 2.1.2. Protease Inhibitors Definition: Antitrypsin, antichymotrypsin, antielastin1 Exposure estimates: 80% to 90% of protease inhibitor activity is removed when SPI is heated1 Trypsin inhibitor content of soy protein isolate can vary as much as fivefold2 Soybean products retain 2.5-12.5% trypsin inhibitor activity of the whole soybean3 Health concerns: Trypsin inhibitors account for 40% of the growth inhibition of raw soy4 Growth depressant5 Stimulate pancreatic hyperplasia in test animals, including carcinoma5 1. 2. 3. 4. 5. American Academy of Peditrics Policy Statement, Pediatrics, 1998 Rackis et al, Qual Plant Foods Hum Nutr, 1985 Miyagi Y et al, J Nutr Sci Vitaminol, 1997 Liener IE , Arch Latinoam, Nutr, 1996 Liener IE, J Nutr,1995 2.1.3. Additional Factors Protein quality Soy protein contains only 1/3 of available nitrogen as essential or semiessential amino acids1 “Soy is not as good a protein source as cow's milk”2 Presence of hemagglutinin Growth depressant3 , might be resistant to dry heat4 Devoid of cholesterol Essential for brain cell development5 Early exposure to cholesterol associated with improved fat metabolism in later life6 Lactose replaced by sugar Lactose & galactose crucial for neural myelination Sugar is not favored because of its “potential effect on teeth and development of inappropriate eating habits”2 Low in chloride Reported cases of hypochloraemic alkalosis7 1. Graham GC et al, Am J Dis Child, 1970 2. U.S. Food and Drug Administration, http://www.fda.gov/fdac/features/596_baby.html 3. Liener IE, Crit Rev Food Sci Nutr, 1994 4. Liu K, Soybeans: Chemistry, Technology, and Utilization, 1997 5. Pond WG, Proc Soc Biol Med, 2000 6. Owen CG et al, Pediatrics, 2002 7. Linshaw MA et al, J Pediatr, 1980 2.2. Phytoestrogens 2.2.1. Definition 2.2.2. The Main Isoflavones in Soy-Based Infant Formula 2.2.3. Exposure Estimates 2.2.4. Bioavailability of Isoflavones 2.2.5. Adverse Effects of Phytoestrogens on Health 2.2.1. Definition of Phytoestrogen “Any plant substance or metabolite that induces biological responses in vertebrates and can mimic or modulate the actions of endogenous oestrogens usually by binding to oestrogen receptors”1 Three main classes of phytoestrogens: Isoflavones Soybeans and soy products Lignans Rye, wheat, sesame seeds, flax Coumestans Vegetables bean sprouts, red clover, sunflower seeds 1. Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment- Working Group on Phytpestrogens, UK 2.2.2. The Main Isoflavones in Soy Formulas1 Percentage Distribution of Total Isoflavone Equivants of the Three Main Isoflavonoids (i.e. Genistein, Diadzein, and Glycetein), their Glucosides, their Acetyl and Malonyl Derivatives % isoflavonoid aglycone equivalents 70 % Total genistein and derivatives % Total diadzein and derivatives % Total glycitein and derivatives 60 50 40 Brands of soy-based infant formula A- ProSobee Soy Formula (powder) B- Farley’s Soya Formula C- Isomil D- SMA Wysoy E- Cow &Gate Infasoy 30 20 10 0 A B C 1. Murphy PA, J Agric Food Chem, 1997 D E 2.2.3. Isoflavones Exposure Estimates1 Average isofalvone intake/day Isoflavone per kg body weight* China (1990 survey)2,3 3 mg 0.05 mg Japan (1996 survey)4 10 mg 0.17 mg Japan (1998 survey)5 25 mg 0.42 mg Japan (2000 survey)6 28 mg 0.47 mg Shown to induce goitrogenic effect in 3 months7 35 mg 0.58 mg Causing hormonal changes in 1 month8 45 mg 0.73 mg Increasing proliferation of breast tissue in 14 days9 45 mg 0.73 mg FDA recommended amount10,3 24 mg 0.40 mg Infants on soy-based formula11 34 mg 6.25 mg * Assumed 60 kg for adults, 6 kg for infants 1. http://westonaprice.org/soy/birthcontrolbabies.html 2. Chen J et al, Diet, Lifestyle and Mortality in China, 1990 3. USDA-Iowa State University Database on the Isoflavone Content of Foods, 1999 4. Fukutake M et al, Food Chem Toxicol, 1996 5. Nagata C et al, J Nutr, 1998 6. Nakamura Y et al, J AOAC Int, 2000 7. Ishizuki et al, Nippon Naibunpi Gakkai Zasshi, 1991 8. Cassidy A et al, Am J Clin Nutr,1994 9. McMichael-Phillips DF et al, Am J Clin Nutr 1998 10. Federal Register, October 1999 11. Setchell KD et al, Am J Clin Nutr, 1998 2.2.3. Isoflavones Exposure Estimates -con’t A Country of Study on Soy-based Infant Formula No. Brands analyzed Total isoflavone level (mg/L) Estimated isoflavone intake Age of infant USA1 5 32-47 4.5-8.0 N/A USA2 6 25-30 5-12 varies New Zealand3,4 5 N/A 3.8 3.3 2.9 1 month 2 months 4 months Austrlia4 4 17-22 NA United Kingdom 5 6 18-41 5.0 4.5 1-2 months 4-6months Switzerland6 N/A N/A 6-20 N/A (mg/kg bw/day) 100 mg isoflavones = 1 contraceptive pill7 1. Setchell KD et al, Am J Clin Nutr, 1998 2. Murphy PA et al, J Agr Food Chem, 1997 3. Irvine CHG et al, Proc Soc Exp Biol Med, 1998 4. Knight DC et al, Paediatr Child Health, 1998 5. MAFF-UK, Nov 1998 6. Tonz O et al, Paediatricia, 1997 7. Bulletin de L’Office Federal de la Santé Publique,1992 2.2.3. Isoflavones Exposure Estimates1- con’d B 0 1 2 3 4 5 6 7 8 9 10 11 12 13 Amount of Isoflavone kg-1 body weight-1 China (1990 survey) Japan (1996 survey) Japan (1998 survey) Japan (2000 survey) Shown to induce goitrogenic effect Causing hormonal changes and increasing breast tissue proliferation FDA recommended amount Infants on soy-based infant formula USA - Setchell et al USA - Murphy et al NZ - 1 month olds - Irvine et al NZ – 2 month olds- Irvine et al UK – 1 to 2 month olds - Reading Switzerland - EEK 2.2.4. Bioavailability of Phytoestrogens Plasma concentration1,2 Circulating concentrations of isoflavones in seven infants fed soybased formula were 13,000-22,000 times higher than plasma oestradiol concentrations in early life Greater than in infants fed breast milk and or cow-milk formulas An order of magnitude higher per bodyweight than typical plasma concentrations of adults consuming soy foods Urinary excretion3 Infants fed soy infant formulas absorb isoflavones, as evidenced from the high but variable urinary concentrations 1. Setchell KD, Lancet, 1997 2. Setchell KD, Am J Clin Nutr, 1998 3. Cruz et al, Pediatr Res, 1994 2.2.5. Adverse Effects of Phytoestrogens A. Thyroid Gland A.1. Infants A.2. Adults A.3. Possible Mechanisms of Action B. Sexual Development and Fertility C. Immune System D. Central Nervous System (CNS) 2.2.5. Adverse Effects of Phytoestrogens A. Thyroid Gland A.1. Effects on Thyroid Gland in Infants 1950s and 1960s: 12 cases documented goitrogenic effect of soy flour infant formula1,2,3 that resulted in substituting soy flour with SPI and supplementing it with iodine 4 Recent studies: Infants with congenital hypothyroidism fed soy-based infant formula have an increased requirement for thyroxine by as much as 18-25% 5 A significant increase in rate of thyroid disease in subjects fed soy-based infant formula as infants6 Incidence of positive thyroid antibodies was 2 1/2 times higher in formula-fed diabetic children than in breast-fed ones7 1. Hydovitz JD, N Engl J Med, 1960 2. Shepard TH et al, N Engl J Med, 1960 3. Van Wyk JJ et al, Pediatrics, 1959 4. Fomon SJ, Nutrition of normal infants, 1993 5. Jabbar et al, J Am Coll Nutr, 1997 6. Fort P et al, J Am Coll Nutr, 1990 7. Lanes et al, J Am Coll Nutr, 1986 2.2.5. Adverse Effects of Phytoestrogens A. Thyroid Gland A.2. Effects on Thyroid Gland in Adults 1. 2. 3. 4. 5. Study Participants Diet Reported Effects Premenopausal women1 Isoflavones (mg/day): 128 T3 Postmenopausal women2 Isoflavones (mg/day): 65, 132 Changes in Thyroid Binding Globulin (TBG) Postmenopausal women3 Isoflavones (mg/day): 56 , 90 Changes in T4 ,T3 & TSH Healthy Japanese men4 35 g soybeans for 3 months Goiter in half subjects 45 year old woman with hypothyroidism6 Soy protein supplement absorption of levothyroxine Duncan et al, J Clin Endocrinol Metab, 1999a Duncan et al, J Clin Endocrinol Metab, 1999b Persky et al, Am J Clin Nutr, 2002 Levy et al Proc Soc Exp Biol Med, 1995 Ishizuki Y et al, Nippon Naibunpi Gakkai Zasshi, 1991 Bell DS et al, EndocrPract, 2001 2.2.5. Adverse Effects of Phytoestrogens A. Thyroid Gland A.3. Possible Mechanisms of Action1 Isoflavones in soy-based infant formula may influence thyroid function in infants by: Acting as a mild goitrogen Reducing absorption of iodine from the gut Increasing loss of thyroxine via the enterohepatic circulation Inhibiting the activity of thyroid peroxidase A study found no free isoflavones in the plasma of four infants after 4 weeks of continuous feeding on soy-based infant formula Huggett AC, Pridmore S, Malnoe A, Haschke F, Offord EA. Phyto-oestrogens in soy-based infant formula. Lancet 1997 Sep 13;350(9080):815-6 1. Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment- Working Group on Phytpestrogens, UK 2.2.5. Advert Effects of Phytoestrogens B. Effects on Development and Fertility Participants Diet Results Adults between Formula as infants: ages of 20-341 cow-based or soybased Infants fed soy formula had in duration menstrual cycles discomfort with menstruation Premenopausal women2 60 g soy protein 45 mg isoflavones Menstrual cycle lengthened & two main ovulation hormones reduced Young women3 20 mg or 40 mg isoflavones daily 80% had prolonged or shortened menstruation Japanese men4 Semi quantitative food frequency questionnaire Serum estradiol concentration significantly inversely correlated with soy product intake Peurto Rican girls5 N/A Positive association between soy formula & premature thelarche Pregnant and lactating rats6 Genstein free, low, or high diets Altered masculinization of reproductive system of offspring 1. Strom BL et al, JAMA, 2001 2. Cassidy A et al, Am J Clin Nutr, 1994 3. Watanabe S et al, Biofactors, 2000 4. Nagata C et al, Nutr Cancer, 2000 5. Freni-Titulaer LW et al, Am J Dis Child, 1986 6. Wisniewski AB et al, J Urol, 2003 2.2.5. Adverse Effects of Phytoestrogens C. Effects on the Immune System Participants Diet Effect Women of ages Formula when infants: Soy-based formula 20-341 cow-based or soyassociated with more use of based allergy and asthma drugs 1. 2. 3. 4. Infants2 Soy-based infant formula Infants3 Soy-protein infant formula Women4 Synthetic isoflavone derivative Strom BL et al, JAMA, 2001 Zoppi G et al, Lancet, 1983 Zoppi G et al, J Pediatr Gastroenterol Nutr, 1982 Alexandersen P, JAMA, 2001 Reduced levels of antibodies in response to routine immunizations Increase in upper respiratory infections and bronchitis Immune proteins decreased Greater impairment in T cell function Depressed lymphocytes 2.2.5. Potential Effects of Phytoestrogens D. Effects on the CNS Study subjects Diet Results Rats1 N/A Genistein reduces DNA synthesis in the brain and inhibits the proliferation of brain cells 7,000 men from Honolulu Heart Program study2 Tofu consumption estimated from dietary assessment Significant dose-dependent risk (up to 2.4 fold) for development of vascular dementia and brain atrophy from consumption of tofu 27 student volunteers aged 22-30 years3 Diets containing 0.5 or 100 mg total isoflavones/day isoflavone intake related to: 1. Yakisich JS et al, Exp Neurol, 1999 2. White LR et al, J Am Coll Nutr, 2000 3. File SE et al, Psychopharmacol, 2001 Small improvements in tests of short and long term memory Mental flexibility More restraintment in a selfassessment of mood 2.3. Presence of Pontential Carcinogens Nitrites Formed during spray-drying1,2 Lysinoalanine Formed during alkaline processing1,2 Phytoestrogens Dietary bioflavonoids may contribute to infantile leukemia3 Genistein may be largely responsible for the development to Infantile Acute Leukemia (IAL)4 Genistein5,6 or soy phytoestrogens7,8 may stimulate proliferation of breast cancer cells “According to their concentration in vitro genistein and daidzein can slow up or stimulate the growth of tumorous cells” 9 1. 2. 3. 4. 5. Life Sciences Research Office, 1979 Rackis, Qual Plant Foods Hum Nutr, 1985 Strick R et al, PNAS, 2000 Abe T, Leukemia, 1999 Dees C et al, Environ Health Perspect, 1997 6. Hsieh CY et al, Cancer Res, 1998 7. McMichael-Phillips DF et al, Am J Clin Nutr, 1998 8. Martin PM et al, Endocrinology, 1978 9. Tonz O et al, Paediatricia, 1997 2.4. Aluminum 2.4.1. Exposure Estimates 2.4.2. Safety Issues 2.4. Aluminum 2.4.1. Exposure Estimates Feeding Aluminum Content (mug/L)1 Plasma Aluminum Concentration (mug/L)2 Human milk 4-65 8.6 Standard cow milk-based formulas, 20 or 24 calories/oz 15-400 9.2 Soy-based formula 500-2400 12.5 Premature infant formula 100-900 9.7 Mean plasma aluminum concentration in soy-based formula fed infants is 45% higher than breastfed children, and 36% higher than infants fed cow milk-based formulas 1. American Academy of Pediatrics, Pediatrics, 1996 2. Hawkins NM et al, J Pediatr Gastroenterol Nutr, 1994 2.4. Aluminum 2.4.2. Safety Issues Concerns associated with increased aluminum intake from soy-based infant formula: Interferes with a variety of cellular and metabolic processes in the nervous system and in other tissues 1 Increased aluminum deposition in CNS 2 Osteopenia2 Infants at increased risk of aluminum toxicity2 Preterm infants Children with renal failure Infants with intrauterine growth retardation 1. American Academy of Pediatrics, Pediatrics, 1996 2. Koo WWK et al, J Am Coll Nutr, 1988 2.5. Manganese 2.5.1. Exposure Estimates 2.5.2. Safety Issues 2.5. Manganese 2.5.1. Exposure Estimates Milk Manganese Content (µg/L)1 Breast milk 10 Cow’s milk-based formula 150 Soy milk-based formula 250 Mangnaese content of soy-based infant formula is 2400% than that of breastmilk 1. Position of the United Soybean Board: Manganese and Soy-Based Infant Formula 2.5. Manganese 2.5.2. Safety Issues Human Studies May be present at higher levels in hair of hyperactive children and children with learning disabilities compared with levels in normal children1 Chronic manganese exposure associated with poor verbal and visual memory2 Animal Studies Accumulates in the brains of animals exposed at young ages3 Exposure to young animals can cause neurodegenerative changes4 Neonatal manganese exposure is related to neurocognitive and developmental deficits in rodent5 1. 2. 3. 4. 5. Collip PJ et al, Ann Nutr Metab, 1983 Woolf A et al, Enviro Health Perspect, 2002 Dorman DC et al, J Appl Toxicol, 2000 Pappas BA et al, Neurotoxicol and Teratol, 1997 Tran TT et al, NeuroToxicol, 2002 2.6. Allergicinity of Soy Soy is a potent allergen1 Soy is at least as antigenic as cow's milk protein2,3 Up to 40% of infants intolerant of cow's milk also develop soy protein intolerance4 Soy protein can cause intolerance reactions with gastrointestinal symptoms & acute anaphylaxis4 Feeding soy formula from birth in infants at increased risk of developing allergy does not have a beneficial effect2,3,5 1. Tonz O et al, Paediatricia, 1997 2. Eastham EJ et al, J Pediatr, 1978 3. Miskelly FG et al, Arch Dis Child, 1988 4. Hill DJ et al, Clin Rev Allergy, 1984 5. Gruskay FL et al, Clin Paediatr, 1982 2.7. Genetically-Modified (GM) Soy GM soy might contain: Lower levels of phytoestrogens by 12-14%1 Higher trypsin inhibitor levels2,3 1. 2. 3. 4. 5. By 27% in raw RR soy By 18% in toasted RR soy Lower choline levels in lecithin by 29%3 Lower levels of phenylalanine3 Double the amount of lectins (hemaglutinin)3 An additional segment of DNA4 Higher concentration of the herbicide glyphosate5 Lappé MA et al, J Med Food, 1999 Padgette SR, J Nutr, 1999 Keeler B, Los Angeles Times, 2001 Palevitz, The Scientist, 2000 Masaharu, Nagoya University, Japan, 2001 3. Position of Various Regulators 1. American Academy of Pediatrics 2. Australian College of Paediatrics 3. Food Safety Authority of Ireland 4. Joint Working Group of Canadian Paediatric Society Nutrition Committee, Dietitians of Canada, and Health Canada 5. New Zealand Ministry of Health 6. Swiss Federal Commission on Food 7. United Kingdom Health Authorities 3.1. American Academy of Pediatrics Soy-based formulas are safe and effective alternatives: Term infants whose nutritional needs are not met from breast milk or cow-based formula Galactosemia and hereditary lactase deficiency Parents seeking a vegetarian diet for term infant Most infants with Ige-mediated allergy to cow milk protein American Academy of Paediatrics, Paediatrics, 1998 3.1. American Academy of Pediatrics- con’d Soy-based formulas have no proven value in: Management of acute gastroenteritis for most previously-well infants Prevention or management of infantile colic Prevention of atopic disease in healthy or high-risk infants Cow milk protein-induced enteropathy or enterocolitis Soy-based formulas not designed or recommended for: Infants with documented cow milk protein-induced enteropathy or enterocolitis Preterm infants who weigh <1800 g 3.2. Australian College of Paediatrics Soy formula is not to be indiscriminately used: In infants with vague symptoms and signs not proven to be due to cow’s milk protein intolerance As prophylaxis in infants thought to be at risk of developing allergy Soy formula may be appropriately prescribed for: Galactosemia Lactose intolerance The use of soy-based infant formula may not be without side effects: Its use may impair immunity The long-term effects of soy (e.g. aluminum and phytoestrogens) are unknown The Australian College of Paediatrics, J Paediatr Child Health, 1998 3.3. Food Safety Authority of Ireland Soy-based infant formula can be used under medical supervision for the treatment of: Transient lactose intolerance Galactosemia IgE mediated cow’s milk allergy Soy-based infant formula can be used under medical supervision in infants whose parents wished to feed their child a vegetarian diet Soy-based formula is not recommended for: Routine use in infants Preterm infants Cows’ milk protein induced enterocolitis or enteropathy Treatment colic Atopic disease Food Safety Authority of Ireland, Recommendations for a national feeding policy, 1999 3.4. Joint Working Group of Canadian Paediatric Society Nutrition Committee, Dietitians of Canada, and Health Canada Restrict use of soy-based formulas only for infants who: “Cannot be fed dairy-based products for health, cultural or religious reasons, including galactosemia or a vegan lifestyle” Soy-based infant formula not recommended: In the management of infants with an allergy to cows’ milk protein For the prevention of atopic diseases Health Canada, Nutrition for Healthy Term Infants, 1998 3.5. New Zealand Ministry of Health Soy formula may be appropriately prescribed only for: Proven cow’s milk protein intolerance or allergy Lactose intolerance Galactosemia Potential interaction between soy infant formula and thyroid function to be considered: Thyroxine replacement should be monitored closely Assessment of thyroid function should be considered if satisfactory growth and development is not achieved or maintained New Zealand Ministry of Health, Soy based infant formula, 1998 3.6. Swiss Federal Commission on Food Use of soya-bean products as baby foods should be made “very restrictive” and is allowed only in a few medical conditions: Lactose intolerance Galactosemia (Possibly) Cow’s milk allergy Soya-bean products should not be used: Routinely in preparation of food for healthy babies For ecological, ideological or ethical reasons “Hydrolyzed or lactose-free products are probably better than those based on the soya bean” 1. Tonz O et al, Paediatricia, 1997 3.7. United Kingdom Health Authorities United Kingdom Department of Health - 1996 Breastfeeding is the best feeding choice and cow’s milk formulae are preferable for most bottle-fed babies. Babies being fed soya-based formula on a healthcare professional’s advice should continue to do so Babies being fed soya-based formula by choice of parents should continue to so so, but parents should seek the advice of a healthcare professional. Food Advisory Committee - 1996 Infant formulae manufacturers should investigate ways to reduce the levels of phytoestrogens in soy-based infant formula 1. Department of Health, London, UK, 1996 2. MAFF, London, UK 1996 3.7. United Kingdom Health Authorities- con’d Scientific Advisory Committee on Nutrition, 20031 Considers that “there is cause for concern about the use of soybased infant formula. Additionally, there is neither substantive medical need for, nor health benefit arising from, the use soybased infant formulae.” Working Group of the Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment (COT)1 – 2003 Recommends to amend the advise of the Department of Health to read as follows: “…soy-based infant formulae be fed to infants only when indicated clinically.” 1. Working Group of the Committee on Toxicity of Chemicals in Food, Consumer Products and the Environment, 2003 http://www.food.gov.uk/multimedia/pdfs/2003-03.pdf “The use of soy formulas as a large, uncontrolled, and basically un-monitored human infant experiment continues unabated”. Dr. Daniel Sheehan National Center for Toxicological Research of the USFDA