hypoxia
advertisement
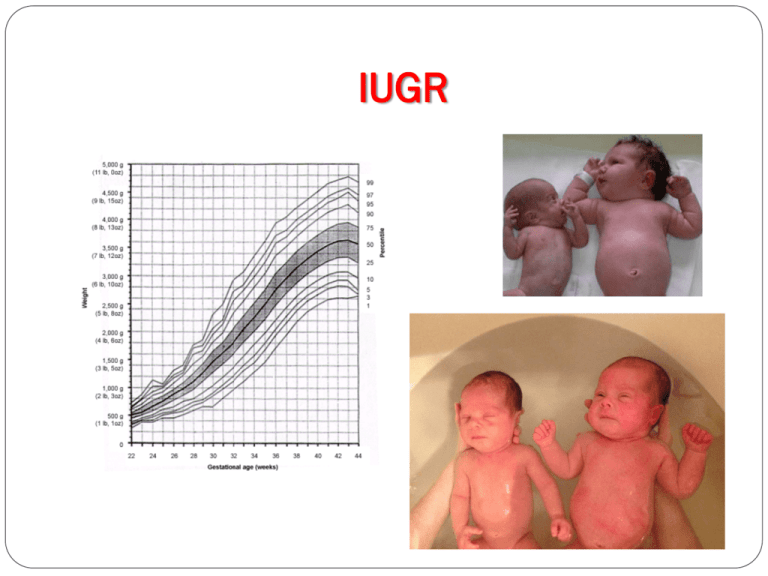
IUGR IUGR Asymmetric IUGR Chronic fetal distress (hypoxia) Preeclampsia Chronic hypertension Diabetes classes D to F Poor caloric intake Symmetric IUGR Genetic Torch Chromosomal Anomalad syndromes Insulin like growth type 1 deficiency Perinatal problems Fetal death Asphyxia Meconium aspiration pneumonia Fasting hypoglycemia Alimented hyperglycemia Polycythemia/ hyperviscosity Temperature instability Dysmorphology Pulmonary hemorrhage Immunodeficiency Decreased bone mineral density DIC Hypoglycemia 1. 2. 3. 4. 5. 6. Decreased hepatic glycogen stores Inactive gluconeogenesis Diminished use and oxidation of FFA Hyperinsulinism Deficient catecholamine release Failure of response to exogenic glucagon Thermal control neutral thermal environment“ This environment is a set of thermal conditions, including air and radiating surface temperatures, relative humidity, and airflow, at which heat production (measured experimentally as oxygen consumption) is minimal and the infant's core temperature is within the normal range. It is a function of the size and gestational age and chronological age of an infant; larger, older infants require lower environmental temperatures than smaller, younger infants do. Methods of heat loss 1- conduction 2- convection 3- evaporation 4- irradiation The concept of "Warm Chain" 1. Warm delivery room (> 25°C) 2. Warm resuscitation 3. Immediate drying 4. Skin-to-skin contact between baby and the mother 5. Breastfeeding 6. Bathing and weighing postponed 7. Appropriate clothing and bedding 8. Mother and baby together 9. Warm transportation 10. Training/awareness of healthcare providers KMC Incubator care Warmer care oxygen Administering oxygen to reduce the risk of injury from hypoxia and circulatory insufficiency must be balanced against the risk of hyperoxia to the eyes (retinopathy of prematurity) and oxygen injury to the lungs. oxygen Although cyanosis must be treated immediately, oxygen is a drug and its use must be carefully regulated to maximize benefit and minimize potential harm. The concentration of inspired oxygen must be adjusted in accordance with the oxygen tension of arterial blood (Pa02) or noninvasive methods such as continuous pulse oximetry or transcutaneous oxygen measurements. Oxyhood Nasal CPAP pulseoximetery In general oxygen saturation should be maintained in the range of 85% to 95%. Fluid therapy Water intake in term infants is usually begun at 70 ml/kg on day 1 and increased to 120 ml/kg by days 2-3. Smaller, more premature infants may need to start with 80 ml/kg on day 1 and advance gradually to 150 ml/kg/day. IV fluid in neonates day 1 2 3 4 5 6 term 70cc/kg 80cc/kg 90cc/kg 100cc /kg 110cc /kg 120cc /kg preterm 80cc/kg 90cc/kg 100cc /kg 110cc /kg 120cc /kg 130cc /kg 7 8 140cc /kg 150cc /kg Insensible water loss BW <1000 1000 - 1250 1251 - 1500 1501 - 1750 1751 - 2000 >2000 IWL(cc/kg/day) 65 55 40 25 20 20 IV fluid Daily weights urine out put - USG BUN Na should be monitored carefully to determine water balance and fluid needs. Clinical observation and physical examination are poor indicators of the state of hydration of premature infants. TPN The goal of parenteral alimentation is to deliver sufficient calories from glucose, protein, and lipids to promote optimal growth. If a peripheral vein is used, it is advisable to keep the glucose concentration below 12.5 g/ dL. If a central vein is used, glucose concentrations as high as 25 g/ dL may be used (rarely). Intralipid may be initiated at 0.5 g/kg/24 hr and advanced to 3 g/kg/24hr, if triglyceride levels remain normal; 0.5 g/kg/24 hr is sufficient to prevent essential fatty acid deficiency. Aminoacids may be initiated at 0.5-1g/kg on first day of life, advanced to 1.5g/kg/day. Control Intralipid infusion with TG Triglyceride concentrations are most often used as an indication of lipid tolerance, and maintaining triglyceride concentrations below 150 to 200 mg/ dL seems prudent. Aminoacid infusion with ALT – AST Glucose infusion with BS Weight gain After a caloric intake of >100 kcal/kg/24 hr is established by total parenteral intravenous nutrition, LBW infants can be expected to gain about 15 g/kg/24 hr. Feeding Oral feeding (nipple) should not be initiated or should be discontinued in infants with: 1. 2. 3. 4. 5. 6. 7. 8. 9. respiratory distress, hypoxia, circulatory insufficiency, excessive secretions, gagging, Severe sepsis central nervous system depression, severe immaturity, or signs of serious illness. Oral feeding The process of oral alimentation requires, in addition to a strong sucking effort, coordination of swallowing, epiglottal and uvular closure of the larynx and nasal passages, and normal esophageal motility, a synchronized process that is usually absent before 34 wk of gestation. feeding most infants weighing <1,500 g require tube feeding because they are unable to coordinate breathing, sucking, and swallowing. Methods of feeding intermittent bolus feedings continuous feeding nasojejunal feeding Gastrostomy feeding Trophic feeding is the practice of feeding very small amounts of enteral nourishment to VLBW preterm infants to stimulate development of the immature gastrointestinal tract. The benefits of trophic feeding include enhanced gut motility, improved growth, decreased need for parenteral nutrition, fewer episodes of sepsis, and shortened hospital stays. Feeding advancement Feeding is started at 1cc/kg q3h, the rate of daily advancement should not be more than 20cc/kg/day. Drop back in feeding vomiting, abdominal distention, or gastric residuals from previous feedings should arouse suspicion of sepsis, necrotizing enterocolitis, or intestinal obstruction. Adding supplements When the amount of feeding approaches 120cc/kg/day corresponding to caloric intake of 80kcal/kg/day the milk should be fortified by adding supplements. Supplements 1-folic acid ¼ tab qd for 3months 2-vitamin E ¼ tab qod for 3months 3-zinc sulfate 1-2mg/kg daily for 6months 4-Ferrous sulfate 2-4mg/kg day* 5-calcium as gluconate salt 100mg/kg/day 6-phosphorus as phosphate Sandoze 50mg/kg/day 7-multivitamin 1ml daily(400U vitamin D) 8-Erythropoietin 250-400U/kg SC three days/week for 3weeks if birth weight is 1250-1500 and for 6weeks if birth weight is below 1250g. Ferrous sulfate *ferrous sulfate is started at 2mg/kg from the age 2 weeks if birth weight is 1500-2500g and at 4mg/kg from the age of 4 weeks if birth weight is less than 1500g. In those babies under erythropoietin treatment the dose of ferrous sulfate is 6mg/kg. Preterm formula Premature formulas contain a reduced amount of lactose (40% to 50%) because intestinal lactase activity may be low in premature infants. The remainder of the carbohydrate content is in the form of glucose polymers, which maintain low osmolality of the formula. The fat blends of preterm formulas are 20% to 50% MCTs to compensate for low intestinal lipase and bile salts. The protein content of preterm formulas is higher than that of term formulas (2.7 to 3 g/100 kcal), which promotes a rate of weight gain and body composition similar to that of the reference fetus. Premature formulas are whey predominant, which reduces the risk of lactobezoar formation and may provide a more optimal amino acid intake. Calcium and phosphorus content is also higher in preterm formulas, which results in improved mineral retention and bone mineral content. Preterm formula If the baby is taking preterm formula at 150cc/kg/day there will be no need for adding the supplements. Growth SGA neonates who have symmetric IUGR related to congenital viral, chromosomal, or constitutional syndromes remain small throughout life. Those infants whose intrauterine growth was inhibited late in gestation because of uterine constraints, placental insufficiency, or nutritional deficits will have catch-up growth after birth and approach their inherited growth potentials when provided with an optimal environment. Developmental outcome Intellectual and neurologic functions in IUGR depends on the presence or absence of adverse perinatal events , in addition to the specific cause of IUGR. Cerebral morbidity will be worsened by hypoxic ischemic encephalopathy subsequent to birth asphyxia, and by the postnatal problems of hypoxia and hypoglycemia. When these perinatal problems are minimal or are avoided, the neonate who is SGA may still demonstrate cerebral developmental problems, especially in the presence of relative head growth retardation. Another major determining influence on neonatal neurodevelopmental outcome in infants who are SGA is the family socioeconomic status. vaccination Palivizumab (Synagis) should be given according to the respiratory syncytial virus (RSV) policy. Breast feeding by a mother who is positive for hepatitis B surface antigen (HBsAg) poses no additional risk for acquisition of hepatitis B virus (HBV) infection by the infant. Vaccination schedule age birth vaccine comments BCG- OPV hepatitis B 0.05ml dose in infants for BCG 2 months DPT- OPV hepatitis B 4 months 6 months DPT- OPV 12 months 18 months 4-6 years MMR DPT- OPV hepatitis B DPT- OPV DPT- OPV MMR Retinopathy of prematurity IVH= intraventricular hemorrhage Bleeding from subepandymal germinal matrix. Grade1= bleeding is confined to germinal matrix Grade 2=intraventricular hemorrhage without ventricular dilation Grade3=intraventricular hemorrhage with acute ventricular dilation (clot fills >50% of the ventricle) Grade4= intraparenchymal lesion intraventricular hemorrhage Intraventricular hemorrhage AOP= apnea of prematurity = idiopathic apnea Apnea: Cessation of respiration for more than 20 seconds, or any duration if associated with bradycardia and cyanosis. The etiology of AOP is immature respiratory center. NEC=necrotizing enterocolitis A common gastrointestinal emergency of premature neonates that presents with abdominal distention and can culminate in intestinal perforation if left untreated. Etiology: ischemia + infection + concentrated formula Stage 1 Suspected NEC Abdominal distention – bloody stools – emesis – gastric residuals Stage 2 Proven NEC Pneumatosis intestinalis and/or portal venous gas ± metabolic acidosis – thrombocytopenia Stage 3 Advanced NEC Pneumoperitoneum – hypotension – DIC – neutropenia