Post Operative Arterial Hypoxemia
advertisement

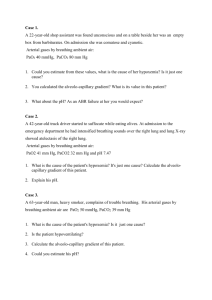
Post Operative Arterial Hypoxemia Oren Erlichman, M.D UCLA Department of Anesthesiology PACU Patient • 73 yo female with hx of depression and chronic cholesthiasis underwent GA for biliary duct leak repair. • Presented to PACU in respiratory distress. • Noted to be weak, altered, unable to talk, with poor inspiratory effort. • VS: 142/83, 114, 15 and shallow, 91-93% on FM. PACU Patient – Continued • Review of Anesthesia chart: – GA, sevo, nitrous, ETT, 3hrs. – 150mcg of fentanyl at beginning of case, 0.4 of dilaudid at the end of case after spontaneous breathing. – 50mg of rocuronium at beginning of case, then vecuronium titrated with nerve stimulator, then fully reversed to sustained tetanus. – Extubated once followed command to eye opening. PACU Patient Studies • ABG – 7.20/83/81/25/93.2 • Other labs normal except for increase in Crt from 0.9 to 1.5. • CXR, EKG – normal. • Rechecked twitches with nerve stimulator – 2mg of Neo/0.4 of Glyco given in PACU. Causes of Arterial Hypoxemia in the PACU • Hypoventilation – Residual narcotics – Residual benzos – Residual inhaled anesthetics – Residual muscle relaxants – Pain, splinting – Restrictive Conditions, abdominal wall binding, abdominal distension – Airway obstruction – Bronchospasm • V/Q mismatch and Shunt – Atelectasis – Inhibition of Hypoxic Pulmonary Vasoconstriction. – Pulmonary edema – Aspiration, Pneumonitis – Increased Venous Admixture How Does Hypoventilation Cause Hypoxemia? • The alveolar gas equation PaO2= FIO2 (Patm-PH2O) – PCO2/R If PaCO2=40 PaO2= 0.21(760-47) – 40/0.8 = 100 If PaCO2=80 PaO2= 0.21(760-47) – 80/0.8= 50 How Does Hypoventilation cause Hypoxemia? • Normally there is a linear increase in minute ventilation for increase in CO2. • This linear ventilatory response is blunted in the post operative period by the effects of drugs. How does V/Q mismatch and shunt cause arterial hypoxemia? • Alveoli that are either not getting perfused or not getting ventilated affect the transport of oxygen. • The diffusion capacity of oxygen is limited compared to that of carbon dioxide. Treatment Identify the Underlying Cause • Hypoventilation – Reversal of drugs – Decrease dead space ventilation – Supplemental O2 – Mechanical ventilation • V/Q Mismatch and Shunt – – – – – Sitting position Incentive Spirometry Encourage deep breathing. Positive airway pressure Supplemental O2, although not effective in true shunt. – Mechanical Ventilation PACU Patient - Course • Patient was assisted with AMBU bag intermittently for 2hrs, with some improvement in mental status and saturation. • Eventually patient was intubated, transferred to ICU and extubated the next day.