Substance-Related Disorders
advertisement

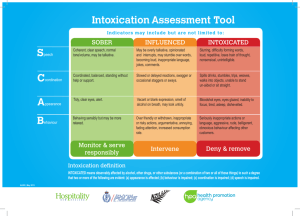
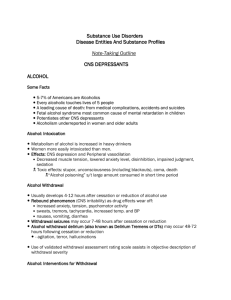
Substance-Related Disorders Core Concept Occurrence of adverse social, behavioral, psychological, & physiological effects caused by 1 or more of the following abused substances: 1) Alcohol 2) Inhalants 3) Amphetamines 4) Nicotine 5) Caffeine 6) Opioids 7) Cannabis 8) Phencyclidine 9) Cocaine 10) Sedatives, Hypnotics, or Anxiolytics 11) Hallucinogens 12) Other or Unknown Substances Categories for Substance-Related Disorders: Substance Use Disorders (generic criteria sets): Substance Dependence Substance Abuse Substance-Induced Disorders (specific criteria sets): Substance Intoxication Substance Withdrawal Substance-Induced Psychiatric Syndromes Substance Dependence & Abuse Criteria for Substance Dependence and Abuse: exactly the same for all 12 classes of substances Names for specific Dx: e.g. Alcohol Dependence, Alcohol Abuse Polysubstance Dependence: a pattern of maladaptive use of at least 3 classes of substances; meet the full criteria for Substance Dependence for substances considered as a group, but not for any single substance Substance Dependence A maladaptive pattern of substance use, leading to clinically significant impairment or distress, as manifested by 3+ of the following, at any time in a 12-month period: Tolerance A need for markedly increased amounts of substance to achieve intoxication or desired effect Markedly diminished effect with continued use of the same amount of substance Withdrawal Characteristic withdrawal syndrome for substance The same or a closely related substance taken to relieve or avoid withdrawal symptoms Substance taken in larger amounts or over longer period than intended. Substance Dependence Symptoms (continued): Persistent desire or unsuccessful efforts to cut down or control substance use. A great deal of time is spent in activities necessary to obtain or use the substance or recover from its effects. Important social, occupational, or recreational activities are given up or reduced because of substance use. Substance use is continued despite having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by the substance. Specifiers: With Physiological Dependence – evidence of tolerance or withdrawal. Without Physiological Dependence – no evidence of tolerance or withdrawal Substance Dependence Course Modifiers: Early Full Remission: no criteria for dependence or abuse have been met at any time for the last 1-12 months Early Partial Remission: 1 or more, but not full, criteria for dependence or abuse have been met for last 1-12 months Sustained Full Remission: no criteria for dependence or abuse have been met at any time for the last 12+ months Sustained Partial Remission: 1 or more, but not full, criteria for dependence or abuse have been met for the last 12+ months In a Controlled Environment: no criteria for abuse or dependence have been met for at least the past month On Agonist Therapy: no criteria for abuse or dependence have been met for at least the past month Substance Abuse A. Maladaptive pattern of substance use, leading to clinically significant impairment or distress, as manifested by 1 or more of the following, occurring in a 12-month period: Recurrent substance use resulting in a failure to fulfill major role obligations at work, school, or home Recurrent substance use in situations in which it is physically hazardous (e.g. driving while impaired) Recurrent substance-related legal problems (e.g. disorderly conduct) Recurrent substance use despite having persistent or recurrent social or interpersonal problems caused or exacerbated by the effects of the substance (e.g. arguments with significant other about substance use, physical fights) B. Symptoms have never met the criteria for Substance Dependence for this class of substance. Differential Diagnosis of Substance Dependence & Abuse Continuum of Substance Use: Recreational Use Problematic Use Substance Abuse Substance Dependence Substance Dependence: adverse consequences & tolerance, withdrawal, compulsive use. Substance Abuse: adverse consequences, but absence of tolerance, withdrawal, or compulsive use. Consider factors such as age, sex, culture, and health. Once person has met criteria for Substance Dependence for a substance, they can never be given dx of Substance Abuse for that substance. Substance Intoxication The development of a reversible substancespecific syndrome, due to recent ingestion of, or exposure to, a substance. B. Clinically significant maladaptive behavioral or psychological changes develop during or shortly after use of the substance due to the effect of the substance on the central nervous system. C. The symptoms are not due to a general medical condition and are not better accounted for by another disorder. A. Substance Withdrawal Development of a substance-specific syndrome due to the cessation of, or reduction in, substance use that has been heavy & prolonged. B. The substance-specific syndrome causes clinically significant distress or impairment in social, occupational, or other important areas of functioning. C. Symptoms aren’t due to a general medical condition and aren’t better accounted for by another mental disorder. A. Necessary Clinical Information Current substance use History of substance use History of substance use emergencies & treatment Cognitive impairment, e.g. confusion, disorientation, impaired attention, rambling thoughts, drowsiness Physiological signs, e.g. tachycardia, hypertension, hypotension, dilation or constriction of pupils Neurological signs, e.g. slurred speech, lack of coordination, ataxia, dystonia, tremor, seizure, etc. Psychomotor agitation or retardation Changes in personality, mood, anxiety Urine drug screening, blood alcohol level Changes in social or family life Current and past legal problems Making a Diagnosis Identification of abused substance(s): Patient admits to using substance(s) Substance is detected in urine or blood Patient has characteristic physiological, behavioral, or psychological signs & Sx of intoxication or withdrawal from substance Current pattern of use: dependence or abuse Abnormal physiological symptoms or signs: current intoxication or withdrawal History of substance abuse Experiencing recent related legal problems: intoxication, abuse, or dependence Maladaptive behavioral or psychological changes: intoxication, withdrawal, abuse, or dependence Treatment Planning Detoxification (for severe withdrawal) Inpatient treatment programs (substance dependence) Outpatient treatment programs Groups: psychoeducation, 12-step recovery, support groups, relapse prevention Evaluate social system (family situation, significant relationships, friendships, support network) & coping skills Prevention strategies: stressing the need for abstinence for those with a strong family Hx of alcoholism or their own Hx of alcohol or substance dependence Alcohol, Sedative, Hypnotic, or Anxiolytic Intoxication Behavioral & Psychological Changes: Inappropriate sexual/aggressive behavior Mood lability Impaired judgment Impaired social/occupational functioning Clinical Signs & Symptoms: Slurred speech Lack of coordination Unsteady gait Nystagmus Impaired attention and memory Stupor or coma Alcohol, Sedative, Hypnotic, or Anxiolytic Withdrawal Autonomic hyperactivity, e.g. sweating, pulse greater than 100 Increased hand tremor Insomnia Nausea or vomiting Transient visual, tactile, or auditory hallucinations or illusions Psychomotor agitation Anxiety Grand mal seizures Amphetamine or Cocaine Intoxication Behavioral & Psychological Changes: Euphoria or affective blunting Changes in sociability Hypervigilance Interpersonal sensitivity Anxiety, tension, or anger Stereotyped behaviors Impaired judgment Impaired social/occupational functioning Amphetamine or Cocaine Intoxication Clinical Signs & Symptoms: Tachycardia or bradycardia Pupil dilation Elevated or lowered blood pressure Perspiration or chills Nausea or vomiting Weight loss Psychomotor agitation or retardation Muscular weakness, respiratory depression, chest pain, cardiac arrhythmias Confusion, seizures, dyskinesias, dystonias, or coma Amphetamine or Cocaine Withdrawal Dysphoric mood Fatigue Vivid, unpleasant dreams Insomnia or hypersomnia Increased appetite Psychomotor retardation or agitation Caffeine Intoxication Clinical Signs & Symptoms: Restlessness Nervousness Excitement Insomnia Flushed face Diuresis Gastrointestinal disturbance Muscle twitching Rambling flow of thought and speech Tachycardia or cardiac arrhythmia Periods or inexhaustibility Psychomotor agitation Nicotine Withdrawal Dysphoric or depressed mood Insomnia Irritability, frustration, anger Anxiety Difficulty concentrating Restlessness Decreased heart rate Increased appetite or weight gain Cannabis Intoxication Behavioral & Psychological Changes: Impaired motor coordination Euphoria Anxiety Sensation of slowed time Impaired judgment Social withdrawal Clinical Signs & Symptoms: Conjuctival injection Increased appetite Tachycardia Dry mouth Hallucinogen Intoxication Behavioral & Psychological Changes: Marked anxiety or depression Ideas of reference Fear of losing one’s mind Paranoid ideation Impaired judgment Impaired social/occupational functioning Clinical Signs & Symptoms: Pupillary dilation Tachycardia Sweating Palpitations Blurring of vision Tremors Lack of coordination Hallucinogen Persisting Perception Disorder Individuals who have previously used a hallucinogen reexperience one or more of the perceptual symptoms that they experienced while intoxicated with the hallucinogen: Geometric hallucinations False perceptions of movement in peripheral visual fields Flashes of color Intensified colors Trials of images of moving objects Positive afterimages Halos around objects Macropsia Micropsia Inhalant Intoxication Clinical Signs & Symptoms: Dizziness Blurred vision or diplopia Nystagmus Stupor or coma Incoordination Euphoria Slurred speech Tremor Unsteady gait Lethargy Depressed reflexes Generalized muscle weakness Psychomotor retardation Behavioral & Psychological Changes: Belligerence Impaired judgment Assaultiveness Impaired social/occupational functioning Apathy Opioid Intoxication Behavioral & Psychological Changes: Initial euphoria followed by apathy Dysphoria Psychomotor agitation or retardation Impaired judgment Impaired social/occupational functioning Clinical Signs & Symptoms: Pupillary constriction Drowsiness or coma Slurred speech Impaired attention or memory Opioid Withdrawal Dysphoric mood Nausea or vomiting Muscle aches Lacrimation or rhinorrhea Pupillary dilation, piloerection, or sweating Diarrhea Yawning Fever Insomnia Phencyclidine Intoxication Behavioral & Clinical Signs & Sx: Psychological Changes: Vertical or horizontal Belligerence nystagmus assaultiveness Hypertension or tachycardia Impulsiveness Numbness or diminished responsiveness to pain Unpredictability Ataxia Psychomotor agitation Dysarthria Impaired judgment Muscle rigidity Impaired social/ occupational functioning Seizure or coma Hyperacusis Substance-Induced Psychiatric Syndromes There is evidence that psychiatric symptoms developed during or within a month of significant substance intoxication or withdrawal. Every class of abused substances, except nicotine, has the capacity to produce psychiatric symptoms during intoxication or withdrawal. Specific diagnosis should specify the name of the abused substance, the psychiatric syndrome, & whether the onset occurred during withdrawal or intoxication, e.g. Alcohol-Induced Anxiety Disorder with onset during withdrawal. Substance-Induced Psychiatric Syndromes Delirium Persisting Dementia Persisting Amnestic Disorder Psychotic Disorder with Delusions Psychotic Disorder with Hallucinations Mood Disorder Anxiety Disorder Sexual Dysfunction Sleep Disorder