Garcia - Sage Products Inc.
advertisement

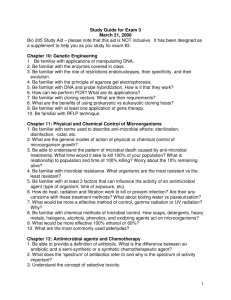
Infection Control & Sage: a Winning Combination A Presentation for the Annual Sage Products Sales Meeting Chicago, IL, October 2, 2002 Robert Garcia, BS, MMT(ASCP), CIC IC Responsibilities • Range: all depts. • Nosocomial infection surveillance • Communicable diseases • Employee health • Sterilization assurance • Medical devices • Sanitation • Antisepsis • Engineering & Construction • Patient Safety • Regulatory requirements • Bioterrorism planning The IC Profession at a Crossroads • 12,000 ICPs and dwindling • Responsibilities up 75% in acute care and 81% in LTC • Staffing has not changed for 60% of IC departments or decreased nearly 25% • 75% over 45 years of age • Most nurses, but where are the nurses? Jackson MM, Soule B, Tweetn SS. APIC Strategic Planning Member Survey, 1997. The Emerging Healthcare Delivery Systems Task Force. APIC. AJIC AM J Infec Control 1998;26:113-25. Lack of Nurses and Infection • >15 studies and reports equate decreased RN nursing staff with increasing nosocomial infections • Needleman J, Buerhaus P, Mattke S, et al. Nurse-staffing levels and quality of care in hospitals. N Eng J Med 2002;346:1715-22 • Jackson M, Chiarello L, Gaynes R, et al. Nurse staffing and health care – associated infections: Proceedings from a working group meeting. AJIC AM J Infec Control 2002;30:199-206. Nosocomial Infections • • • • • • 4th leading cause of death in U.S. >$4 billion dollar cost to hospitals LTC, Ambulatory, others $ = unknown Resistant organisms IOM Report Media reports ECONOMIC PRESSURE HEALTHCARE INFLATION COST OF TECHNOLOGY MEDICAID CUTS MANAGED CARE Prophetic Insight on Future Paths “…Because we do not provide direct care to patients, the value of our practice must be demonstrated in other ways. We must translate infection control activities into proposals and systems that gain priority by stressing quality and economy.” • Pantelick EL. Hospital infection control: Dinosaur or dynasty. Am J Infect Control 1989;17:56-61. APIC Research Foundation Priorities Project • A review of the world’s literature on IC and ID over the last 20 years • Identified 65 of most published authors • 43 responded to survey • #1 top priority: Cost-effectiveness/financial impact studies Report from the Research Foundation, APIC Educational Conference & International Meeting, June 2000, Minneapolis, MN. What is at Stake? • For infection control professionals: – A necessary increase in institutional value attained by sustained decease in infections and demonstration of cost reductions • For Sage: – The confirmation that a proven and high quality product does make a difference – Enhanced market position An Emerging Methodology Interventional Epidemiology “…IE examines all functions from a global health care viewpoint; that is, it takes into consideration the potent changes outside of a healthcare organization and in response integrates this knowledge into the internal process systems of the facility.” Garcia R, Barnard B, Kennedy V. The Fifth Evolutionary Era in Infection Control: Interventional Epidemiology. AJIC Am J Infect Control 2000;28:30-43 People Communication Between Providers Procedures Analysis of System Components Influencing the Occurrence of Ventilator-Associated Pneumonia Intubation/Extubation Physicians VAP surveillance rounds (observational periods between IC and nurses) Suctioning (closed/oral) Nurses Oral Care Respiratory Therapists Pharmacists Relay surveillance data to healthcare providers Cleaning & maintenance of ventilator and components Feedback from healthcare providers Handwashing Nutritional Specialists Placement & maintenance of nasogastric tube VAP Mechanical ventilator (Heated humidifier or HME) Vent circuits, filters Closed suction system, oral suction catheters, water, other suction devices, suction canisters/tubing Tracheostomy devices Nasogastric tubes Nebulizers Multidose vials Laryngoscopes Resusitation bags Definition of VAP Intubation/Extubation Self-extubation Closed suctioning Semi-recumbent positioning Handwashing Oral & Dental Care Cleaning of Use of H2 ventilator/other devices antagonists/sucralfate Tracheostomy care Ventilator circuits Filters Cleaning of laryngoscopes Nebulizers Suction canisters Enteral feeding Resuscitation bags Weaning Placement and care of nasogastric tubes Barrier equipment Equipment & Devices Policies The Practice Arena of Interventional Epidemiologists Clinical Financial Customer Satisfaction How can SAGE Help Bolster IC Value? • Provide a fresh perspective on infection transmission • Provide economic and clinical rationale • Provide viable interventional methodologies • Provide effective education • Provide support for the span of the partnership Hospital Water: Is it a Source for Nosocomial Infections? Causative Agent Reservoir Susceptible host Portal of exit Portal of entry Mode of Transmission The Chain of Infection. Components of the Infectious Disease Process. Water as a Reservoir of Nosocomial Pathogens • It is known that organisms such as Pseudomonas aeruginosa, Serratia marcescens, and Acinetobacter calcoaceticus can replicate in relatively pure water • May be present in drinking water that has acceptable limits of safety (<1 coliform bacterium/100 mL). P. aeruginosa Infections due to Hospital Water Sources • >12 reports indicating transmission and development of infection from contaminated hospital water – Trautmann M, Michalsky T, et al. Tap water colonization with Pseudomonas aeruginosa in a surgical intensive care unit and relation to Pseudomonas infections of ICU patients. Infect Control Hosp Epidemiol 2001;22:49-62. Burn Infections • Tap water has been cited as the source for serious wound and sepsis – Kolmos HJ, Thuesen B, et al. Outbreak of infection in a burn unit due to Pseudomonas aeruginosa originating from contaminated tubing used for irrigation of patients. Infections from Hospital Sinks • Many reports have identified the presence of gram-negative bacteria in hospital sinks • Organisms may survive for >250 days on sink surfaces – Simor AE, Ramage L, et al. Molecular and epidemiologic study of multiresistant Serratia marcescens infections in a spinal cord injury rehabilitation unit. Infect Control Hosp Epidemiol 1988;9:20-27. Tip of the Iceberg • More than 40 citations of water as a source of nosocomial infections • Anaissie et al estimate that >1,400 deaths occur each year due to waterborne nosocomial pneumonia due to P.aeruginosa alone – Anaissie EJ, Penzak SR, Dignani C. The hospital water supply as a source of nosocomial infections. A plan for action. Arch Intern Med 2002;162:1483-92. “…In such settings, hospital water may have contaminated environmental surfaces (eg, sinks, drains, and whirlpool baths), medical equipment (eg, by rinsing tube feed bags, endoscopes, respiratory equipment, etc., with tap water), or health care providers, leading ultimately to patient exposure.” - Anaissie EJ, et al. The hospital water supply as a source of nosocomial infections. A plan for action. Arch Intern Med 2002;162:1483-92. How are Patients Exposed to Hospital Water? • • • • • • • Handwashing (cross-contamination) Bedpans Enteral feedings Respiratory equipment Drinking Showering Bed bathing Basin Bath Drawbacks • • • • • High consumption of resources Negative impact on nursing and patients Damaging effects on the skin Contamination risks with basins & water Real economics of basins Why Should Hospitals Care? • Most of your patients skin is at risk • Cost of skin breakdown in U.S.: $13 Billion • Nosocomial contamination may lead to nosocomial infection • Cost of nosocomial infection: $5.9 Billion • JCAHO Patient Safety Quality Indicators • Patient ‘barometer’ for their quality of care Source: Stone P. et al, Outcomes of ICU Working Conditions, Nov 2001 Nursing Shortage vs. Patient Outcomes JCAHO Expert Panel Report “Insufficient staffing not only adversely impacts health care quality and patient safety, it also compromises the safety of nurses themselves” Source: Joint Commission on Accreditation of Healthcare Organizations, August 2002 Damage to the Skin • Soaps can strip the acid mantle, raise the pH and compromise the epidermis • Washcloths introduce friction because they are harsh and rough • Soap and washcloths are fragile skin’s worst enemy Sources: Friers, S.A. Ostomy, Wound Management June 2001 Bryant R. A. Ostomy, Wounnd Management June 2001 Wysocki A. Acute and Chronic Wounds 2nd Edition 2000 Who’s Skin Are We Talking About? • Your Patient – – – – – – – – Majority are elderly Most have pruritic skin condition Epidermis and dermis are thinner Skin has reduced barrier function Reduced skin elasticity Poor epidermal turnover Lowered sebum production Loss of subcutaneous fat and muscle Source: Thomas MD, D., Clinical Journal of Medicine, Cleveland Pressure Ulcers • 1.6 million cases per year in acute care alone • varied settings: – – – – – medical wards surgery and operating rooms intensive care units rehabilitation centers long term and home care Prevalence of Pressure Ulcers • Reported rates to be between 3% and 11% • Two large studies: – 9.2% (148 hospitals) 1 – 7% (116 hospitals) 2 1. Meehan M. Multisite pressure ulcer prevalence survey. Decubitus 1990;3:4-14. 2. Whittington K, Patrick M, Roberts JL. A national study of pressure ulcer prevalence and incidence in acute care hospitals. J Wound Ostomy Continence Nurs 2000;27:209-15. Cost Impact: Hospitals • Unadjusted mean costs: – With Pressure ulcers - $37,288 – Without pressure ulcers - $13,924 • Adjusted for admission predictors and nosocomial infections: – With pressure ulcers - $29,048 – Without pressure ulcers - $13,819 Allman RM, Goode PS, Burst N, et al. Pressure ulcers, hospital complications, and disease severity: Impact on hospital costs and length of stay. Adv Wd Care 1999;12:23-30. Basinborne Contamination Study • Hospital personnel do not perceive basin bath water as significantly contaminated • 100% of the samples in the study were positive for bacterial growth, 60.8% were gram negative • The bacterial count in basin water was so high it was similar to the bacterial count in the urine from patients with UTI’s • Employee’s, wearing contaminated gloves used during the procedure, were observed to touch many environmental surfaces. • Basin water may serve as a reservoir of antibiotic resistant organisms Source: Shannon R et al., Patient Bath Water as a Source of Nosocomial Microbiological Contamination: An intervention Study using Chlorhexidine. J Healthcare Safety Infect Control, 1999;3:180-84. Basinless Bathing • Removes the risk of basin contamination • Removes the risk of waterborne contamination • 8 washcloths to reduce transfer of organisms • Mild cleanser helps maintain skins natural barrier • Single-use helps reduce environmental/cross contamination • No water spills reduce slips & fall potential Better Science and Patient Safety What’s the Real Cost to Bathe with a Basin? Nursing $5.11 $6.84 per bath Energy, Water & Sewer $.10 Laundry Processing $.98 Materials $.65 Source: Total Delivered Cost Analysis Database from U.S. hospitals 1997 - 2002, Sage marketing data on file. Solid Economics $6.84 total $3.68 total $5.11 Nursing Time $1.83 Nursing Time $1.73 $.98 Laundry &Linens Basinless Bath $.10 Water,Sewer,Energy $1.10 to $1.90 $.65 Materials Basin Bath Cost Basinless Cost Source: Total Delivered Cost data analysis of U.S.hospitals 1997-2002 $1.90 $1.10 Linen Savings Summary $100,000 Baylor University Medical Center Linen Dollars Saved $90,000 $339,139 Cumulative Savings $94,425 $94,909 $80,000 $70,000 $70,677 $60,000 $50,000 $40,000 $36,010 $30,000 $24,851 $20,000 $18,266 $10,000 $0 Bath Blankets Bath Towels Straight Sheets Wash Cloths Fitted Sheets Pillowcases Jan. 1999 – Apr. 2002 Nursing Time Reallocated 90,000 89,870 Gallons Saved 80,000 70,000 72,783 60,000 2,499,200 Gallons Saved 69,007 50,000 40,000 30,000 36,520 20,000 10,000 0 Time Spent per Bath Water Consumption Savings 35 30 104,133 Cumulative Nursing Hours Created 35 minutes 25 20 15 10 10 minutes 5 0 1999 2000 2001 2002 BASINS BASINLESS Monthly Water Savings with Comfort Bath™ Jan. 1999 – Apr. 2002 Jan. 1999 – Apr. 2002 Time is on Your Side Original Price H o s p i t a l p r i c e $5.50 $5.00 New Concept High Distribution Margins $4.00 One or two Product Choices $3.75 Manufacturing Efficiencies $3.00 GPO Contracts $2.25 $2.00 $2.05 Multiple Product Choices $1.90 $1.00 '96 '97 '98 '99 '00 $1.10 '01 '02 Ventilator-Associated Pneumonia Is Dental & Oral Care a Valid Part of a Global Prevention Program? VAP Facts • Mechanical ventilation increases risk of pneumonia 6-21 times (1% per day) • Attributable mortality is 27% and increases to 43% when etiologic agent is P.aeruginosa or Acinetobacter sp. • LOS with VAP is 34 days and 21 days without VAP What strategies have been advocated in preventing VAP? • • • • • • • • • Ventilator circuit replacement Semirecumbent positioning of patients Closed suction catheter replacement Heat and moisture exchanger replacement Selective digestive decontamination Oral and dental care Stress ulcer prophylaxis Enteral feeding methodologies Weaning People Communication Between Providers Procedures Analysis of System Components Influencing the Occurrence of Ventilator-Associated Pneumonia Intubation/Extubation Physicians VAP surveillance rounds (observational periods between IC and nurses) Suctioning (closed/oral) Nurses Oral Care Respiratory Therapists Pharmacists Relay surveillance data to healthcare providers Cleaning & maintenance of ventilator and components Feedback from healthcare providers Handwashing Nutritional Specialists Placement & maintenance of nasogastric tube VAP Mechanical ventilator (Heated humidifier or HME) Vent circuits, filters Closed suction system, oral suction catheters, water, other suction devices, suction canisters/tubing Tracheostomy devices Nasogastric tubes Nebulizers Multidose vials Laryngoscopes Resusitation bags Definition of VAP Intubation/Extubation Self-extubation Closed suctioning Semi-recumbent positioning Handwashing Oral & Dental Care Cleaning of Use of H2 ventilator/other devices antagonists/sucralfate Tracheostomy care Ventilator circuits Filters Cleaning of laryngoscopes Nebulizers Suction canisters Enteral feeding Resuscitation bags Weaning Placement and care of nasogastric tubes Barrier equipment Equipment & Devices Policies Ventilator Circuits • Humidifier vs. HME technology • CDC Draft: Do not change routinely, on the basis of duration of use, the ventilator circuit (i.e., ventilator tubing and exhalation valve, and the attached humidifier) that is in use on an individual patient. Rather change the circuit when it is visibly soiled or mechanically malfunctioning. Cat IA [same as for HME - Cat II ]. – Kollef MH, Shapiro SD, Fraser VJ, Silver P, Murphy D, Trovillion E, et al. Mechanical ventilation with and without 7-day circuit changes: a randomized controlled trial. Ann Intern Med 1995; 123;168-74. Semirecumbent Positioning • CDC Draft: If there is no medical contraindication, elevate at an angle of 30-45° the head of the bed of a patient at high risk for aspiration pneumonia, e.g., a person receiving mechanical ventilation.…Cat IB – Drakulovic MB, Torres A, Bauer TT, Nicholas JM, Nogue S, Ferrer M. A Supine body position as a risk factor for nosocomial pneumonia in mechanically ventilated patients: a randomized trial. Lancet 1999;354:1851-58. Closed Suction Catheters • Manufacturers: replace at 24 hours • CDC Draft: If the closed-system suction is used, change the in-line suction catheter when it malfunctions or becomes visibly soiled. Cat IB – Kollef MH, Prentice D, Shapiro SD, Fraser VJ, Silver P, Trovillion E, et al. Mechanical ventilation with or without daily changes of in-line suction catheters. Am J Resp Crit Care Med, 1997;156:466-72 Heat & Moisture Exchangers (HME) • Hydroscopic vs. hydrophobic • CDC Draft: …use a heat-moisture exchanger (HME) to prevent pneumonia in a patient receiving mechanical ventilation. Cat II. Change an HME…when it malfunctions mechanically or becomes visibly soiled. Cat IB • Davis K, Evans SL, Campbell RS, Johannigman JA, Luchette FA, Porembka DT. Prolonged use of heat and moisture exchangers does not affect device efficiency or frequency rate of nosocomial pneumonia. Crit Care Med 2000;28:1412-18. – Studied 220 consectutive SICU patients – HME changed at 24h or 120h, measuring resistance and colonization – No differences after 5 days in resistance or colonization Stress Ulcer Prophylaxis • Theory has it that modifying stomach acid effects the bacterial colonization level • “after all of this time and study, it is likely that neither drug has any advantage in significantly maintaining gastric flora and reducing VAP.” – Livingston DH. Prevention of ventilator-associated pneumonia. Am J Surg 2000;179(suppl 2A):12S-17S. Selective Digestive Decontamination • Preventive decolonization on the theory that the gut is a major source of VAP • 30+ studies to date • “…this selective pressure on the epidemiology of resistance definitely precludes the systematic use of SDD for critically ill patients” – Eggimann P, Pittet D. Infection control in the ICU. Chest 2001;120:2059-2093. Evidence of the Need to Control Oral and Dental Colonization in Order to Prevent VAP 1. Oral Cavity vs. Gastric Colonization • “…decolonization approaches in the prevention of nosocomial pneumonia strongly suggests that oropharyngeal decontamination, indeed, represents the effective part of SDD, and that the majority of antibiotic use in SDD is unlikely to add beneficial effects” – Bergmans DCJJ, Bonten MJM, Gaillard CA, Paling JC, van der Geest S, van Tiel F, Besens AJ, et al. Prevention of ventilatorassociated pneumonia by oral decontamination. A prospective, randomized, double-blind, placebo-controlled study. Am J Resp Crit Care Med 2001;164:382-88. 2. Further Evidence... • ...that oropharyngeal colonization rather than gastric colonization leads to VAP – Garrouste-Orgeas M, Chevret S, Arlet G, Marie O, Rouveau M, Popoff N, Sclemmer B. Oropharyngeal or gastric colonization and nosocomial pneumonia in adult intensive care unit patients. A prospective study based on genomic DNA analysis. Am J Respir Crit Care Med 1997;156:164 – Bonten MJM, Gaillard GA, Van Tiel H, Smeets GGW, Van Der Geest S, Stobberingh EE. The stomach is not a source for colonization of the upper respiratory tract and pneumonia in ICU patients. Chest 1994;105:878-84. 3. Oral Pathogens & Respiratory Infect. • 20 trial subjects on mechanical ventilation • at 24h, all patients identified with potential pathogens in oral secretions • 67% of sputum cultures with pathogens • 94% of oral suction devices colonized after 24h of use Sole ML, Poalillo FE, Byers JF, et al. Bacterial growth in secretions and on suctioning equipment of orally intubated patients: A Pilot study. Am J Crit care 2002;11:141-49. 4. Oral Pathogens & Respiratory Infect. • A review article • 6 articles cited as support for a relationship between poor oral health and resp. infect. • Bacteria from colonized dental plaque may be aspirated into the lower airway Scannapieco FA.Role of oral bacteria in respiratory infection. J Peridont 1999;70:793-802. * Available on Sage Intranet 5. Dental Plaque as a Contributor to VAP • Fourrier E, Duvivier B, Boutigny H, Roussel-Delvallez M, Chopin C. Colonization of dental plaque: a source of nosocomial infections in intensive care patients. Crit Care Med 1998;26:301-8. – Study on dental plaque colonization and ICU nosocomial infs. – Dental plaque occurred in 40% of pts. – Colonization of dental plaque was highly predictive of nosocomial infection – Salivary, dental, and tracheal aspirates cultures were closely linked 6. Oral Decolonization: Use of Chlorhexidene • DeRiso AJ II, Ladowski JS, Dillon TA, Justice JW, Peterson AC. Chlorhexidene gluconate 0.12% oral rinse reduces the incidence of total nosocomial respiratory infection and nonprophylactic systemic antibiotic use in patients undergoing heart surgery. Chest 1996;109:1556-61. – 353 pts undergoing coronary bypass surgery – Used chlorhexidine gluconate (0.12%) as oral rinse to prevent nosocomial infections – Randomozed to receive CHG or placebo – Overall reduction in nosocomial infections of 65% when using CHG – Respirtaory infections were reduced 69% in CHG group Subglottic Secretion Suctioning • CDC Draft: Use an endotracheal tube with a dorsal lumen above the endotracheal cuff to allow drainage (by continuous suctioning) of tracheal secretions that accumulate in the patient’s subglottic area. CAT 1B – Valles J, Artigas A, Rello J, et al. Continuous aspiration of subglottic secretions in preventing ventilator associated pneumonia. Ann Intern Med 1995;122:179-86. – Kollef MH, Skubas NJ, Sundt TM. A randomized clinical trial of continuous subglottic suctioning in cardiac surgery patients. Chest 1999; 116:1339-46. Biofilms • Complex layers forming on the surfaces of medical devices • Contain “mother” bacteria which bread pathogenic “free-floating” organisms • Nearly impervious to antibiotics – Donlan RM. Biofilms and device-associated infections. Emerging Infect Dis 2002;2:277-81. Biofilms & VAP • Clear association between development of biofilm and VAP • “Conclusion: ET biofilms are clinically relevant, locate closer to the patient than ventilator, and mature over time. Staging of ET biofilms is possible and correlates with increased pneumonia, LOS, and cost.” – Bergstein JM, Thomas JG, Kincaid SD, et al. Endotracheal tube biofilm stage correlates with outcome in surgical critical care patients. [abstract] 1st Annual Joint Meeting, Surgical Infection Society 22nd Annual Meeting Surgical Infection Society-Europe 15th Annual Meeting, May 2-4, 2002, Madrid, Spain. Surg Infect 2002;3:90. Is there a comprehensive, effective, and readily available system to address many of the factors that influence the occurrence of VAP? VAP Reduction by Oral Care: A Successful Project • Implemented the use of assessment tools • Introduced Oral Care System • From 5.6/1000 VD to 2.2/1000 VD – Schleder B, Stott K. The effect of a comprehensive oral care protocol on patients at risk for ventilator-associated pneumonia. J Adv Health 2002;4:27-30 CDC 2002 Draft Guidelines on Pneumonia Prevention: Does not address dental or oral care as a factor in the occurrence of ventilatorassociated pneumonia !!!!!! ????? Summary: What Works in Reducing VAP • • • • • Semi-recumbent positioning Circuits-filters-closed suction = 1 system Subglottic suctioning Dental & oral care Weaning Summary on Dental & Oral Care • Oral, rather than gastric colonization, plays major role in VAP events • Dental plaque acts as a source of pathogens • Good supportive science • Poor oral care contributes to swift biofilm formation • Good oral care reduces infection Benefits of Complete Oral Care System • Closed system • Provides major components of global prevention program (dental/oral care & subglottic suctioning) • Provides anti-microbial solution • Nurse friendly • Provides assessment tools My appreciation for your wonderful support, Robert Garcia, BS, MMT(ASCP) Brookdale University Medical Center One Brookdale Plaza Brooklyn NY 11212 516-810-3093 rgarcia@brookdale.edu