Patient
advertisement

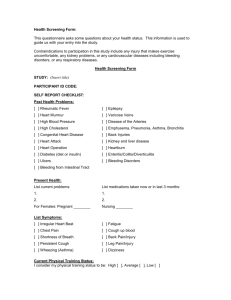
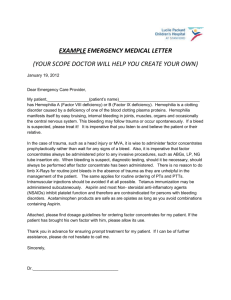
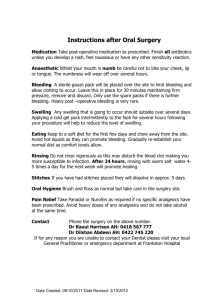
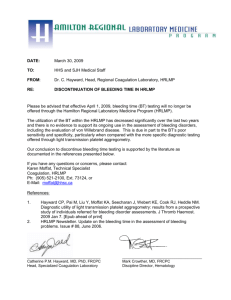
Diagnosis of the bleeding patient Diana Oelofse • Descriptions of “bleeders” date back a few centuries. • The first modern description of haemophilia, as an example of a bleeding disorder likely came from the American physician John Otto in 1803. • This description is the first in which the inheritance pattern is clearly stated. • And the first instance of what we now know as X-linked inheritance in any disorder. • “Otto clearly recognized both that the bleeding disorder was limited to males and the possibility of its transmission by healthy female relatives.” • We know now however that bleeding disorders can be hereditary or acquired. • And that females can also be affected by hereditary bleeding disorders, in some instances as often as males for e.g. VWD. • The evaluation of the patient with a suspected bleeding diathesis has the potential to provoke much diagnostic uncertainty. • A severe bleeding disorder is generally a relatively straightforward diagnostic process. • But in contrast the work-up for minor bleeding disorders can be complicated. • There is currently no test available that serves as a reliable screening test for global haemostasis. • (that includes the bleeding time - which does not predict bleeding) • In addition some patients have multiple acquired abnormalities in their haemostatic systems. • This may also be the case in hereditary bleeding disorders – where for e.g. VWD with Haemophilia A or B can co-occur, or concurrent Factor V deficiency and Haemophilia A. • Screening tests may point to the possible presence of defects in primary haemostasis or a factor deficiency. • Specific diagnosis : requires more detailed testing. • Laboratory studies have limitations including preanalytical errors, false negatives, long distances to reference laboratories for tests that cannot be done locally and costs involved. • In Port Elizabeth we are able to do basic screening tests and some of the more specialized tests. (with Livingstone NHLS being our regional reference laboratory for urgent tests) • Non-urgent specialized tests are often done in larger centralized labs. • Some specialized tests are however only available on site at certain universities in South Africa (for e.g. LPA) Pre-analytic errors • Problems with citrate vacutainers • Biological effects – Partially filled tubes – Vacuum leak and citrate evaporation – Hct ≥55 or ≤15 – Lipemia, hyperbilirubinemia, hemolysis • Problems with phlebotomy • Divers laboratory errors – – – – – Heparin contamination Wrong label Slow fill Under-fill Too vigorous shaking – Delay in testing – Prolonged incubation at 37°C – Freeze/thaw deterioration Aims when investigating a patient/family with suspected bleeding disorder / bleeding risk Determine likelihood that patient (family) has a haemorrhagic disorder, using the medical history and then confirmed by laboratory investigations. Is there implications for family members and potential offspring? • Attempt to estimate risk. • Establish a management plan for future problems and/or to at least reduce risk for invasive procedures. Stages in normal coagulation • Initiation phase : vasconstriction, platelet adhere to site (VWF), exposed collagen interaction with platelets and interaction between TF and FVII = TF/FVIIa : activation X and IX. • Amplification phase : thrombin activation of platelets and activation of procoagulant cofactors Va and VIIIa. (on a primed platelet surface) • Propagation : Burst of thrombin generation on platelets through the more stable platelet surface generated Xa (via IXa ), + Va : Thrombin = leading to fibrin formation. • Localization : TFPI, ATIII, Thrombomodulin, Prot C and C and fibrinolysis. Reproduced with permission from Sysmex http://www.healthcare.siemens.com/hemos tasis/hemostasis-onlinecampus/interactive-hemostasis-cascade The extent of laboratory investigations for an obvious, or possible bleeding diathesis is strongly informed by the “bleeding history” and also guided by clues from the physical investigation and context of the presentation. • Extensive work-up mandatory in major bleeds – these patients are relatively few. • (Possible) Minor bleeders problematic. • They may be normal or have mild to moderate bleeding disorders. (platelet secretion defects or mild VWD) • Tosetto et al. defines a bleeder as a patient with an increased bleeding rate. Number of bleeding episodes occurs within a defined time frame in the patients life. • Bleeding rate = Number haemorrhages/time Bleeding History • Bleeding symptoms are often reported by otherwise healthy subjects. • Trivial (non-relevant) is considered part of the human phenotype. • Trivial bleeding never interferes with daily activities or requires medical attention. • Minor bleeding severe enough to interfere with daily activities • Major bleeding may cause permanent damage or be life threatening. • Various established scoring systems / Bleeding assessment tools available. https://bh.rockefeller.edu/ISTH-BATR Other indicators that may be derived from the history: • • • • Bleeding localized / diffuse. Spontaneous vs provoked. Mucocutaneous vs. joint bleeds. Delayed onset bleeding. Factor XIII deficiency A2 antiplasmin deficiency Plasminogen activator inhibitor-1 deficiency • Bleeding in male and female members of a family. • Consanguinity. Physical examination • Skin : petechiae, ecchymoses, perifollicular haemorrhages, telangiectasia around mounth (HTS),distribution, oculocutaneous albinism, hepatosplenomegaly and lymphadenopathy,stigmata of liver disease • Joint hypermobility and skin hyper-elasticity in Ehlers-Danlos Syndrome • Aortic Stenosis in acquired VWD. • Large tongue, carpal tunnel syndrome peri-orbital purpura in amyloidosis – several acquired factor deficiencies. Laboratory Investigations • FBC, U/E and Creatinin, LFTs • Clotting Screen Prothrombin time : Extrinsic ( F 2 5 10 + 7 ) liver pathology, warfarin therapy PTT Intrinsic ( F12 11 9 8 + 2 5 10) Trombin Time and Fibrinogen (Common path) DIC , Heparin therapy and dysfirbinogenaemia Bleeding time : Result depends on integrity of blood vessels, platelet function, VWD. Not standardised. Ivy template method 3 – 8min PFA - 100 D-Dimers :DIC • Corrections studies and Factor assays • Von Willebrand Disease screen (often needs to be repeat and can be complex) • LTA (light transmission aggregometry) • Electron microscopy platelets • Evaluation of fibrinolysis Two stage approach First Stage • FBC • PT • PTT • Fibrinogen • TT • BT / PFA-100 • VWF assays • FVIII • ABO blood group Second Stage (Depending on results of first stage) • Specific coagulation factors • Mixing tests • VW:Collagen binding assay • VWFM • LTA • FXIII • Antiplasmin • Fibrinolysis exploration Coagulation tests in context of simplified clotting cascade Intrinsic Pathway (F12,11,9, Extrinsic Pathway F8 ) (TF and F7) F10 PTT PT/INR F5 Correction studies Correction studies Common Pathway Thrombin time Thrombin (F 2) F13 Clauss Fibrinogen Clot lysis time, α2 antiplasmin Fibrinogen → Fibrin D-Dimers FDPs A quick and accurate method for measuring fibrinogen in plasma J. Lab. Clin. Med. 1961 Sep; 58; 477-88 Ellis BC, Stransky A. Coagulation factor disorders • Inherited bleeding disorders – Hemophilia A and B – vonWillebrands disease – Other factor deficiencies • Acquired bleeding disorders – Liver disease – Vitamin K deficiency/warfarin overdose – DIC – Acquired inhibitors to factors Platelet problems can be congenital or acquired platelet abnormalities, and quantitative and qualitative Blood Vessels in Hemostasis: • • • • • Initial phase of hemostasis. Simple easy bruising – women Senile purpura – atrophy, Scurvy – vit C deficiency, collagen def. Steroid induced purpura • Henoch-Schonlein purpura – children. ( *Acquired F 13 deficiency) Patient - 1 Abnormal PT Abnormal PTT Repeat with 50:50 mix 50:50 mix is abnormal Test for inhibitor activity: Specific : Factors V, X, Prothrombin, fibrinogen (rare) Non-specific: anti-phospholipid (common) 50:50 mix is normal Test for factor deficiency: Isolated deficiency in common pathway: Factors V, X, Prothrombin, Fibrinogen Multiple factor deficiencies (common) (Liver disease, vitamin K deficiency, warfarin, DIC) Patient - 2 Normal PT Abnormal PTT Repeat with 50:50 mix 50:50 mix is abnormal Test for inhibitor activity: Specific factors: VIII,IX, XI Non-specific (anti-phospholipid Ab) 50:50 mix is normal Test for factor deficiency: Isolated deficiency in intrinsic pathway (factors VIII, IX, XI) Multiple factor deficiencies (rare) Patient - 3 Abnormal PT Normal PTT Repeat with 50:50 mix 50:50 mix is abnormal Test for inhibitor activity: Specific: Factor VII (rare) Non-specific: Anti-phospholipid (rare) 50:50 mix is normal Test for factor deficiency: Isolated deficiency of factor VII (rare) Multiple factor deficiencies (common) (Liver disease, vitamin K deficiency, warfarin, DIC) Evaluation of a Bleeding Patient 4 normal PT normal PTT Abnormal Urea solubility Factor XIII deficiency Normal Consider evaluating for: Mild factor deficiency Monoclonal gammopathy Abnormal fibrinolysis (a2 anti-plasmin def) Elevated FDPs Platelet disorder Vascular disorder To conclude with Dr Otto: And now 210 years later….. Thank you ! References 1. Key,Makris et al. Practical Haemostasis and Thrombosis, Second edition. Pg1 2. Hayward, Moffat 2013. Laboratory testing for bleeding disorders, uses of high and low-yield tests IJLH 3. Tosetto, Castaman et al. 2013. Bleeders, bleeding rates and bleeding score. JTH 4. Schulman, Angeras et al.2010.Definition of major bleeding in clinical investigations of antihemostatic medicinal products in surgical patients. JTH 5. Redeghiero, Michel et al. 2013. Standardization of bleeding assessment in ITP from the IWG. Blood. 6. The Medical Research Council`s General Pratice Research Framework. Thrombosis prevention trial. 1998 Lanset 7. Ridker,Cook et al . A Randomised trial of low dose aspirin in the primary prevention of CVD in women. 2005. NEMJ 8. http://www.genmedhist.info/articles-and-papers/ 9. https://bh.rockefeller.edu/ISTH-BATR 10. De Moerloose et al. Diagnosis of mild bleeding disorders. 11. Diagnosis and management of mild bleeding disorders.Hayward. ASH