The Sydney Cancer Centre - Research Network for Metals in Medicine
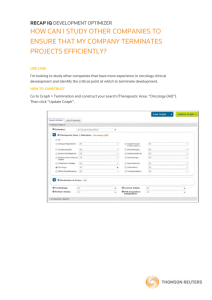
advertisement

Metals in Medicine Consortium Sydney Cancer Centre Sydney Cancer Centre Clinical Oncology Departments of: • Royal Prince Alfred Hospital Medical Oncology Radiation Oncology Surgical Units (urology, melanoma, breast, GI, H&N, cardiothoracic, etc) Palliative Care Haematology • Concord Hospital • Dubbo Hospital SCC Clinical Research Links • Pharmaceutical Industry • University of Sydney (Med Psychology, Chemistry, Pharmacology) • Australian cooperative groups (disease specific) • US National Cancer Institute: US cooperative groups (ph III) Cornell University phase II consortium (ph II) CTEP organ dysfunction working group (ph I) • Other international cooperative groups Essential Clinical Resources for Developmental Therapeutics Research • Clinicians • Patients • Clinical research staff • Regulatory infrastructure • Laboratory interface SCC Clinical Capability (Medical Oncology) A/Prof Michael Boyer Dr Philip Beale Dr Jane Beith A/Prof Stephen Clarke Dr Anne Hamilton Dr Lisa Horvath Prof John Simes Dr Martin Stockler Dr Anne Sullivan Prof Martin Tattersall • 2000 new patients per year • 200 patients on clinical trials per year • 40 active protocols at any point in time • 12 research staff (nurses / admin) including RT / Concord / Dubbo Key SCC Personnel - Metals in Medicine • Dr Philip Beale Director, Med Oncology, CGRH/Dubbo GI, gynae, breast, clin pharm • A/Prof Michael Boyer Director, Med Oncology, CSAHS/RPAH lung, GU, H&N • A/Prof Stephen Clarke Head, Clinical Pharmacology GI, lung, clin pharm • Dr Anne Hamilton Head, Clinical Trials breast, melanoma, gynae, clin pharm End-points of Phase I studies • Recommended phase II dose and schedule • Human toxicology profile • Pharmacokinetics • Pharmacodynamics • Preliminary efficacy data Role of Clinicians in Developmental Therapeutics Research 1. Protocol Planning (Registration Strategy) 2. Patient Selection and Treatment 3. Translational Laboratory Research Capability (“Bench to Bedside”) 4. Imaging Capability Protocol Planning (Registration strategy) • selection of schedule / route of administration • selection of starting dose / dose escalation plan • selection of monitoring according to knowledge of toxicities in drugs of same class / preclinical data • development of strategies for managing side effects / problems as they occur • identification of clinical “niches” for drug development • knowledge of competing molecules Patient Selection and Treatment • identification of appropriate patients • informed consent • drug administration • monitoring and management of efficacy and toxicity • determination of relationship of clinical events to the study drug • supportive care • reporting (regulatory) Translational Research Capability “Bench to Bedside” Concord Laboratory Cell lines • In vitro drug activity in sensitive and resistant cell lines Animal (xenografts / immune competent animals) • pharmacokinetics (LCMS) • pharmacodynamics • toxicology • anti-tumour activity Translational Research Capability “Bench to Bedside” Human (pretreated cancer / tumour targeted population) • pharmacokinetics (LCMS) • pharmacodynamics • PET labelled compounds (tissue distribution / “real time” PK)