RCC
advertisement

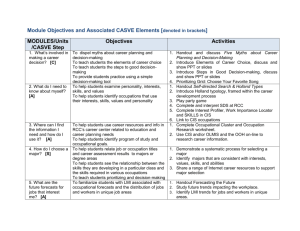
In the name of God Genitourinary Tumors ALI ARIAFAR, MD Fellowship of Uro-oncology Shiraz University of Medical Sciences Kidney tumors Primary or Secondary (metastatic) Malignant: RCC represents 80-85% of primary renal neoplasms Transitional cell carcinoma 8% Benign tumors: simple renal cyst Oncocytomas Angiomyolipoma Inflammatory Radiologic Evaluation of Renal Mass Sonography CT Scan MRI Oncocytoma Mostly benign Eosinophilic cytoplasm with fine granule. 3-5% of renal tumors CT :central scar Angiography :spoke wheel appearance. No definitive diagnostic test. Treatment: radical nephrectomy Angiomyolipoma Renal hamartoma F>M Incidence in tuberose sclerosis: 45-80% Diagnosis : CT( HF -20 to -60) Treatment: asymtomatic <4cm : annual F/U >4cm or symptomatic :angioembolization or partial nephrectomy Renal Cell Carcinoma (RCC) Rcc is the most lethal of the urologic cancers. 2-3% of all adult malignancies is RCC MR of RCC is 40% in contrast with the 20% MR of bladder and prostatic cancers Rcc is primarily a disease of the elderly pt. with presentation in the 6th and 7th decades M/F ratio is 3/2 Risk Factors The majority of cases of RCC are believed to be sporadic; only 2% to 3% are familial The only generally accepted environmental risk factor for RCC is tobacco exposure. (1.5 to 2.5 times) Tobacco use accounts for 20% to 30% of cases of RCC in men and 10% to 20% in women Obesity HTN Acquired cystic kidney disease due to dialysis Western diet (high in fat and protein and low in fruits and vegetables), increased intake of dairy products, and increased consumption of coffee or tea Familial RCC Von Hippel-Lindau (VHL) Major manifestation: retinal Angioma, CNS hemangioblastoma, pheoQ, epididymal cystandenoma, endolymphatic tumor of ear and RCC. Genetic element: loss of chromosome 3. The most common cause of MR in VHL is RCC. Tuberous sclerosis Epilepsy, Sebaceous adenoma, mental retardation Hereditary papillary RCC (HP RCC) Hereditary leiomyomatosis and RCC Autosomal dominant mode. Proto-oncogene on chromosome 7. Uterine leiomhyoma + RCC Birt- Hogg-Dube syndrome lung problem + RCC Genetic: chromosome 17. Pathology Clear cell carcinoma: VHL, 70-80% of all RCC Papillary RCC (10%-15%) : ARCD Chromophobe RCC(3%-5%) Collecting duct RCC. (<1%) Renal modularly RCC(rare) almost exclusively with sickle cell trait and young African-American Clear cell and papillary RCC arise from proximal tubules. Chromophobe and collecting duct RCC arise from distal part of nephron. Clinical Presentation More than 50% of RCC are now detected incidentally The classic triad of flank pain, gross hematuria, and palpable abdominal mass is now rarely found Paraneoplastic syndromes Anemia- anemia of chronic disease 30% Hepatic dysfunction in the absence of metastasis 3-20%(stauffer syndrome) Hypercalcemia 20% Cachexia and Fever 20% Erythrocytosis: 3-10% produce erythropoietin Elevated ESR Neuromyopathy Diagnosis Imaging IVP or Sonograghy CT Scan MRI Biopsy Staging and Prognosis Cohen HT, McGovern FJ. NEJM. 2005;353:2477. Prognosis Prognosis depends upon stage Other poor prognostic indications include poor performance status, anemia, hypercalcemia, and elevated LDH Five-year relative survival rates by tumor stage at diagnosis based on cases diagnosed during 1992–1999, followed through 2000. Drucker BJ. Cancer Treat Rev. 2005;31:536. Treatment Radical nephrectomy remains the main stay for treatment RCC. Partial nephrectomy is standard treatment for small (<4cm), unilateral, confined tumor, and for pts with bilateral or solitary kidney. RCC is radio- and chem. Resistant. Advanced RCC Treatment Primary treatments are systemic therapy with molecularly targeted therapy or immunotherapy Surgery is palliative therapy - - Solitary metastatic site Solitary recurrence following nephrectomy Symptoms related to bulkiness of disease including pain, nausea, or GI obstruction Advanced RCC Immunotherapy IL-2 INF Targeted Therapy Sorafenib sunitinib temsirolimus Bladder Tumors In men, BT is the fourth most common cancer after prostate, lung, and colorectal cancer In women it is the ninth most common cancer whites> blacks; But blacks have a worse prognosis M/F=3:1 . But Women have a worse prognosis Median age at diagnosis is 68 y, incidence increases with age Risk Factor Cigarette Smoking Occupation Infection Inflammation Pelvic Irradiation Chemotherapy Nutritional Factors Fluid Intake Analgesic Abuse Coffee and Tea Risk Factor Hereditary First-degree relatives of patients with bladder cancer have a twofold increased risk of developing urothelial cancer Tumor suppressor gene P53 gene is the most common altered gene in human cancers. Oncogenes (p21 ras, c-myc, and c-jun) Pathology of Bladder Cancer Transitional Cell Carcinoma 90% (TCC) squamous cell carcinoma 5-7% more common in middle east schistosomiasis also seen in chronic catheterization Adenocarcinoma 2-3% Urachal tumor Symptoms The most common presenting symptom of BT is painless hematuria which occurs in 85% of pts. The 2nd most common presenting symptom is frequncy, urgency and dysuria. Blank pain, ureteral metastasis symptoms. obstruction, edema, Physical Exam Superficial bladder cancer is rarely found during a physical examination. Occasionally, an abdominal or pelvic mass may be palpable. Examine for lymphadenopathy Diagnosis U/A Cytology Cystoscopy and biopsy Urinary Cytology Voided or urine washing 40-60% sensitivity (as high as 90% in G3 Lesions) Dependent on grade of tumor Incidence of + urine cytology according to grade Grade # patients Negative (%) Positive (%) I 68 62(91) 6(9) II 60 41(68) 19(32) III 20 6(30) 14(70) Heney et al. J Urol, 130: 1083, 1983 Imaging Sonography CT Scan IVP Staging of Bladder Cancer Stage at diagnosis More than 70% of all newly diagnosed bladder cancers are superficial 50-70% are Ta 20-30% are T1 10% are CIS 5% of patients present with metastas 25% of affected patients have muscle-invasive disease at diagnosis. Surgical treatment TURB(gold standard in superfacial BC) Partial cystectomy Radical cystectomy(gold standard in muscle invasive) Medical treatment Non–muscle-invasive disease (Ta, T1, CIS) Intravesical immunotherapy ( BCG) Intravesical chemotherapy Muscle-invasive disease (T2 and greater) Adjuvant and neoadjuvant chemotherapy Cancer of prostate (Ca.P) Ca.P has been the most common visceral malignant neoplasma in USA. The estimated life time risk of disease is 17.6% for whites and 20.6% for blacks. The black men have the highest incidence of Ca.P and the lowest rate occur in Asia. Risk Factors Age Prostate cancer is rarely diagnosed in men younger than 50 years old, accounting for only 2% of all cases . The median age at diagnosis is 68 years, with 63% diagnosed after age 65 Risk Factors Androgens. Family Hx. Relative risk increase according to the number of affected family members, their degree of relatedness and the age at which they were affected. Accumulating evidence suggests that Ca.P may have an infectious etiology. (prostatitis or STD) Symptoms and signs Most patient are asymptomatic LUTS: frequency, urgency, hesitancy, ↓ed caliber of urine stream, obstructive uropathy Metastatic symptoms: Bone pain, Dyspnea, Cough, etc. D.x DRE PSA: cut off= 4ng/ml Free PSA: free PSA: free/total<18%, PSA density> 15%, PSA velocity>75% TRUS-bx Digital Rectal Exam • Start annual exams when 50 years old Based on: Mayo Clinic Health Letter, April PSA Levels by Age Based on: Time, April 1, 1996 PSA Test Detects an enzyme (prostate specific antigen) made by the prostate PSA increases with age in healthy men PSA increases dramatically with prostate cancer but can also increase with inflammation or an enlarged prostate Needle Biopsy for Prostate Cancer Biopsy gun inserted through anus Needles shot into prostate from rectum 6 to 18 samples taken Attempting to detect cancer in stage A Analysis of cancer spread and cell type Based on: Mayo Clinic Health Letter, April, Treatment Watchful Waiting Active Surveillance Radical prostatectomy Radiotherapy Hormone therapy Chemotherapy TESTICULAR TUMOUR 1% to 2% of cancers among men in the United States The most common malignancy among men aged 20 to 40 years 99% of all Testicular Tumors are malignant. The incidence of bilateral GCT is approximately 2% 95% of which are germ cell tumors (GCTs). GCTs are broadly classified as seminoma (52% to 56%) Classic Typical Seminoma Spermatocytic Seminoma Seminoma is the most common type of GCT. On average, seminomas occur at an older average age than NSGCTs, with most cases diagnosed in the fourth or fifth decade of life NSGCT (44% to 48%) Embryonal Carcinoma. Choriocarcinoma Yolk Sac Tumor. Teratoma Risk Factors Cryptorchidism Males with cryptorchidism are four to six times more likely to be diagnosed with testicular cancer, but the relative risk (RR) falls to 2.0 to 3.0 if orchidopexy is performed before puberty Testis Atrophy ( infection,trauma) Risk Factors family history of testicular cancer An individual’s RR for testicular cancer is 8.0 to 12.0 with an affected brother compared with 2.0 to 4.0 in those with an affected father personal history of testicular cancer Men with a history of testicular cancer are at a 12-fold increased risk of developing GCT in the contralateral testis Signs and Symptoms The most common presentation of testicular cancer is a painless testicular mass Dull Ache or Heaviness in Lower Abdomen 10% - Acute Scrotal Pain 10% - Present with Metatstasis - Neck Mass / Cough / Anorexia / Vomiting / Back Ache/ Lower limb swelling 5% - Gynecomastia Rarely - Infertility Diagnostic Testing and Initial Management ScrotalUltrasonography Serum Tumor Markers (LDH, AFP, and hCG) Chest X Ray CT Scan All patients with a solid, Firm Intratesticular Mass that cannot be Transilluminated should be regarded as Malignant unless otherwise proved AFP EC and yolk sac tumors secrete AFP. Choriocarcinomas and seminomas do not produce AFP. Patients with pure seminoma in the primary tumor with an elevated serum AFP value are considered to have NSGCT. The half-life of AFP is 5 to 7 days. HCG Approximately 15% of seminomas secrete hCG. hCG is also secreted by choriocarcinoma and EC The half-life of hCG is 24 to 36 hours TREATMENT Radical Inguinal Orchiectomy A transscrotal orchiectomy or biopsy is contraindicated TREATMENT Seminomas: Radio-Sensitive. Treat with surveillance ,Radiotherapy or chemotherapy Non-Seminomas are Radio-Resistant and best treated by surveillance ,Surgery(RPLND) or chemotherapy Advanced Disease or Metastasis - Responds well to Chemotherapy Limits of Lymph Nodes Dissection For Right & Left Sided Testicular Tumours PROGNOSIS Seminoma Stage I99% Nonseminoma 95% to 99% Stage II 70% to 92% 90% Stage III 80% to 85% 70% to 80%