PowerPoint - Minnesota Brain Injury Alliance
advertisement

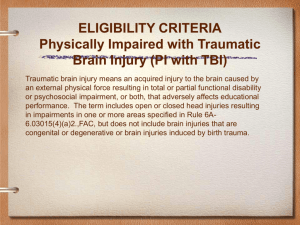
CRANIUM; IT’S NOT JUST A GAME: MILD & MODERATE TRAUMATIC BRAIN INJURIES IN CHILDREN Andrew W. Kiragu, MD, FAAP Interim Chief of Pediatrics Medical Director, PICU Hennepin County Medical Center Assistant Professor of Pediatrics University of Minnesota FACES OF TBI Disclosures • I have no relevant financial relationships with the manufacturers of any commercial products and/or commercial services discussed in this CME activity • I do not intend to discuss any unapproved commercial product/device in this presentation GOALS OF THE PRESENTATION • Discuss a representative case of pediatric TBI • Review epidemiology, evaluation and initial management of traumatic brain injury • Briefly review pathophysiology of TBI • Review other aspects of TBI management including follow-up, family-centered care and injury prevention GOALS OF THE PRESENTATION • Discuss a representative case of pediatric TBI • Review epidemiology, evaluation and initial management of traumatic brain injury • Briefly review pathophysiology of TBI • Review other aspects of TBI management including follow-up, family-centered care and injury prevention CASE REPORT • Patient FP is an 11 year-old boy who presented to the ED after being struck by a vehicle while riding his bicycle. • He was out riding with his friends and they had been going fairly fast downhill when he swerved to avoid an object on the road. • Swerved into the path of a slow moving truck, was struck and flung off his bike. • Landed on the pavement and struck his unhelmeted head. He was observed to lose consciousness for about 2-3 minutes. CASE REPORT • The driver called 911 and paramedics arrived to find him still lying on the sidewalk somnolent but rousable • He opened his eyes to voice, was able to talk but was confused and could only localize pain CASE REPORT • Initial GCS 12 (E3, V4, M5) • He was transported to the ED for additional evaluation and treatment CASE REPORT • Initial Vital signs: T36.7 C, HR124, RR20, BP110/56, SpO2 98% on RA • Gen: more awake and somewhat combative. Bruise and swelling noted over forehead and large abrasion noted of right forearm • HEENT: NC, swelling and bruising of forehead, PERRL, no nasal dc, • Chest: CTA B • CV: nl S1S2, RR increased heart rate CASE REPORT • Abdomen: soft, NT, NABS, no HSM • Ext: abrasion of R forearm, MAE, WWP • Neuro: awake but somewhat combative, intermittently following commands, GCS 14(E4, V4, M6) • Taken for head CT which significant for two small punctate hemorrhage in frontal lobe. Soft tissue swelling of forehead seen. No fracture • Labs in ED including electrolytes and CBC normal • Sent to PICU for overnight observation EPIDEMIOLOGY • There are approximately 1.7 million traumatic brain injuries sustained in the US annually • 50,000 die; • 235,000 are hospitalized; and • 1.1 million are treated and released from an emergency department. EPIDEMIOLOGY • Over 85% of the 1.7 million TBI’s occurring annually in the US are considered mild. • The average incidence of mild TBI was 503.1 per 100,000 population, with a peak among American Indians/Alaska Natives (1026/100,000 population) and in children younger than 5 years old (1115.2/100,000 population). • The mechanisms by which children sustain head injury vary by activity, age, helmet use, and geographic location. EPIDEMIOLOGY • Among children aged 0 to 14, TBI results in over 400,000 ED visits, 2685 deaths and 37,000 hospitalizations each year. Injury rates are highest among children 0 to 4. • Approximately 50% of patients hospitalized with TBI are younger than 20 INTRODUCTION • The term concussion has been used interchangeably with mild traumatic brain injury (TBI) • Defined as a trauma-induced alteration in mental status that may or may not involve the loss of consciousness (LOC). • Cerebral concussion is considered a diffuse brain injury and is associated with widespread disruption of brain function. INTRODUCTION Wing, R & James, C; Emerg Med Clin N Am 31 (2013) 653–675 INTRODUCTION • Not usually associated with visible lesions that can be detected by current imaging techniques. • The primary injury mechanism for a concussion is thought to be from a rotational acceleration force . • No head injury should be considered minor. EPIDEMIOLOGY • Falls • Motor vehicle crashes • Sports and recreational injuries • Violence including child abuse and child on child violence EPIDEMIOLOGY • Severity • Mild 80-85% • Moderate to Severe 12-15% • Fatal 4-5% EPIDEMIOLOGY • Average cost of hospitalization for a child with mild TBI $10,000 up to $3+ million for severe TBI leading to PVS. • The annual cost of hospitalization for TBI estimated in the US at $100 billion. • Immeasurable price to individual and family and to society as a whole. • Head injury the single greatest cause of lost potential productivity in children. EVALUATION • History • Physical Examination • Laboratory evaluation • Imaging • Cognitive evaluation/Neuropsychology • PT/OT/SLP EVALUATION • Primary Survey • Neurologic Assessment • Airway • Pupillary response • Breathing • Responsiveness • Circulation • Glasgow Coma Scale • Disability • Modified Glasgow Coma Scale • Exposure EVALUATION Wing, R & James, C; Emerg Med Clin N Am 31 (2013) 653–675 EVALUATION • Head CT imaging an important tool in the management of TBI. • Provides valuable information regarding the type, location, and severity of intracranial injuries, skull fractures, and cervical spine injuries. • Newer improved technology allows faster and more detailed imaging to be obtained. • Unfortunately, increased CT use leads to increased radiation exposure as well as increased costs EVALUATION Advances in Imaging: MRI DTI Tractography RISK FACTORS FOR DELAYED COMPLICATIONS • Age of less than 2 years a moderate risk factor for ICI after head trauma. • Lower threshold for imaging studies of younger children because historical and clinical factors may not be available or present for assessment PECARN Guidelines Kupperman, n et al. Lancet 2009; 374: 1160–70 PATHOPHYSIOLOGY PATHOPHYSIOLOGY • Impact -head striking a surface or being struck by object • Inertial (translational, rotational or both) • Penetrating • Anoxic PATHOPHYSIOLOGY • Are potentially preventable and are caused by: • Hypoxia/ischemia • Energy failure • Brain swelling/edema • Excitotoxicity • Necrosis/Apoptosis • Inflammation SPORTS CONCUSSIONS SPORTS CONCUSSIONS • High concussion risk organized sports such as wrestling and boxing described as early as 776 BC • Sports related concussions recognized historically but remain a frequent and controversial topic • Increased concern, awareness and prevention efforts including at the legislative level SPORTS CONCUSSIONS • Differences between sports concussions and concussions from other etiologies • Sports concussions a particular problem in pediatrics • Children at increased risk SPORTS CONCUSSIONS • More than 300 000 sport-related concussions occur annually in the United States • More than 60 000 cases of concussions occur at the high school level, with football accounting for the majority of these. • Approximately 4% of high school and collegiate football players sustain concussions during each season. • 1 250 000 student-athletes participating at the high school level SPORTS CONCUSSIONS • Recent concerns over the health of athletes who sustain concussions. • Practice guidelines and parameters for evaluating and managing the head-injured athlete have been developed. • The various guidelines released have raised controversy since not enough data on concussion grades and return-to-play criteria SPORTS CONCUSSIONS • Baseline and post concussion neuropsychological testing • ImPACT testing (Immediate Post-Concussion Assessment and Cognitive Testing) • Return to play guidelines • Return to school guidelines SPORTS CONCUSSIONS • Heads Up Campaign-CDC • Information for coaches, parents and student athletes regarding concussions • Guidelines for recognition and treatment SPORTS CONCUSSIONS SPORTS CONCUSSIONS Thiessen, ML & Woolridge, DP; Pediatr Clin N Am 53 (2006) 1 – 26 SPORTS CONCUSSIONS Thiessen, ML & Woolridge, DP; Pediatr Clin N Am 53 (2006) 1 – 26 OUTCOMES OF MTBI • Related to: • Severity of injury • Severity of intracranial hypertension • Secondary brain injuries • 20% of mild brain injury have some deficit • 90-100% of moderate to severe will have deficit OUTCOMES OF MTBI • Neurologic sequelae • motor deficits • sensory deficits • hearing and vision should be formally tested • Communication difficulties • Cognitive deficits • Behavioral problems OUTCOMES OF MTBI • The short- and long-term complications of mild TBI in children are poorly understood. • Postconcussive syndrome refers to the constellation of acute symptoms after a mild TBI. • These symptoms can be somatic (headache, dizziness, blurriness), emotional (irritability, anxiety), and cognitive (concentration and memory) POST-CONCUSSION SYNDROME POST-CONCUSSION SYNDROME • Studies have assessed physical, behavioral, and cognitive outcomes across the severity continuum of head injuries. • Speech and feeding difficulties associated with an increasing severity of head injury, but not walking. • Headaches are among the most common postconcussive symptoms reported • Also, temper outbursts, dizziness, mood swings, anxiety, and aggressive behavior have been reported. POST-CONCUSSION SYNDROME • Children with mild TBI do well in their recovery, but studies have found that not all mildly injured children recover completely. • In one study 50% of the study group made a good recovery, but only 18.4% made a full recovery without discernible sequelae. • Unclear what the threshold of injury severity below which the risk of late morbidity could be discounted. CTE • Concerns about effects of repetitive head trauma • Recent professional athlete cases • NFL money for research etc. Rehabilitation • Treatment directed at maximizing functional independence by reducing impairment, disability and handicap. • Early intervention. • Interdisciplinary team effort/organization. • Short-term rehabilitation- consider intra-facility resources • Long-term rehabilitation-specialized facility(note agerestrictions) RETURN TO SCHOOL • When children with head injury return to school, they may be expected to assimilate immediately with the class. • The child’s teacher may not understand the head injury or even know the child suffered a MHI, which could affect how the child is treated, observed, or graded. • In one study, teachers knew of the child’s head injury in only 39.8% of the children, and there was a significant linear trend across injury severity groups. RETURN TO SCHOOL • Special educational needs were provided for only 65% of the children identified with such needs. • At follow-up, 18.7% of the children were currently having difficulties with schoolwork • Interestingly, 18% of the children had been disciplined by the school for problem behavior after sustaining their head injury Return to Play Wing, R & James, C; Emerg Med Clin N Am 31 (2013) 653–675 FOLLOW-UP • Pediatric Traumatic Brain Injury Clinic • Mild/Moderate TBI Clinic • Primary care Physicians • Return to school • Return to sports • PT/OT/Neuropsychology/SLP • Brain Injury Association of Minnesota PREVENTION • All head trauma is potentially preventable. • Ensure a safe environment for kids. • Educate regarding motor safety. • Emphasize helmet use, age-appropriate MV restraints to prevent or attenuate injury. • Educate about guns (limit access). • Educate about prevention of inflicted head injuries. PREVENTION • Heads Up Campaign by CDC • National and regional injury prevention programs • Role of pediatricians • State and federal legislation RESEARCH • Need for ongoing research into brain injury treatment • Need for increased federal and foundation funding for traumatic brain injury. Conclusions • Traumatic brain injuries are a common cause of morbidity and mortality in children • Damage to the brain cannot be reversed • Sports related concussions are a continued problem for the pediatric population • Advances in management of MTBI offer hope for improved outcomes • Research into the pathophysiology of MTBI crucial • PREVENTION IS KEY QUESTIONS?