Important point biochem mid2 Lec1: Carbohydrates digestion: Mouth
advertisement

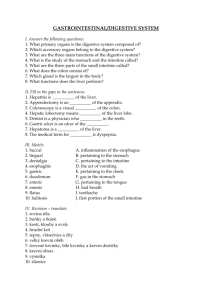
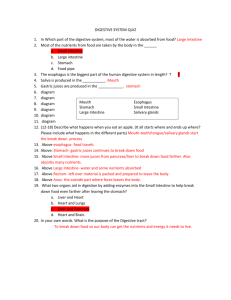
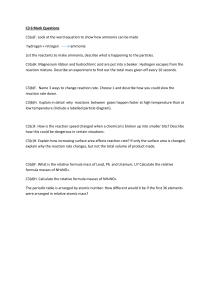
Important point biochem mid2 Lec1: Carbohydrates digestion: Mouth: salivary a-amylase Stomach: no digest salivary a-amylase can’t catch to work there. Intestine: Pancreatic bicarbonate > neutralization Pancreatic a-amylase > oligosaccharide and disaccharide ^ Those enzymes from pancreas lactese, Sucrase, maltes > free glucose ^ From intestine Glucose and galactose transport by sodium dependent glucose cotransporter-1 < need energy Fructose transport by sodium-independent transporter (GLUG-5) < no need energy Example Q: Infant drink milk with watery diarrhea has abdominal discomfort and gases? Answer: lactose intolerance < lactase deficiency Or defect in intestine Treated by milk free lactose Maybe the cause a drug damages the intestine wall. Protein digestion: Mouth: no digest. Stomach: secret pepsin “zymogen” activated by HCL < breakdown the protein Intestine: Pancreatic enzymes: trypsin, chymotrypsin, elastase, carboxypeptidase Most digest in pancreas. All the enzyme zymogen “inactive” activated by trypsin after it activated by entrokinase. Elastase> endopeptide Carboxypeptidase> exopeptide Intestine enzyme: aminopeptidase Example Q: Enzyme digest protein from pancreas? Carboxypeptidase. Lec2: Enzymes digest lipid: Lingual lipase, gastric lipase, pancreatic lipase 1-Gastric lipase> breakdown short and medium chain “milk” baby depend on it. 2-Bile salt > emulsification “ increase surface area for pancreatic enzyme to work faster” Form from liver and stored in gall bladder, derived from cholesterol. 3-Pancreatic lipase: the important one in lipid digestion. Work in Triacylglycerol in carbon 1,2 to give 2 monoacylglycerol and 2 F.A Colipase >anchore for pancreatic lipase * Orlistat inhibit pancreatic lipase > will not digest so not absorbed and loss in stool. Phospholipid: break down by phospholipase 2 < remove F.A from carbon 2. The remnant lysophospholipid break down by lysophospholipase Cholesterol ester> by cholesterol ester hydrase > to give free cholesterol After all break down “digested” Short and medium chain direct from intestine to portal by albumin The long chain: Bile salt > micelles “to absorbed” The micelles contain: 2 monoacylglycerol, free F.A, free cholesterol < will go inside intestine cell Then will resynthesis to TAG, PL, CE. Transport: by chylomicrons Apo B48 > carrier in the circulation, HDL> give apoC, apoE To enter the adipose tissue need apo C to active liopproteinlipase Lipopropteinlpase> F.A and glycerol Remnant of chylomicron: apoC go back to HDL The apoE active uptake the remnant to the liver. Example Q: 1- In deficiency of lipoproteinlipase what will elevate in blood? Answer: chylomicron or trygylecrol. 2- Deficiency in aopE what will elevate in blood? Answer: remnant of chylomicron or cholesterol. 3-patient with malabsorption and statorriha and has live cirrhosis, the defect will be in? Answer: no bile salt 3- Patient with pancreas disease treatment will be? Answer: diet with short chin and medium chin, milk product. Lec3: b-oxidation of F.A occurs in mitochondria. Long chain more than 12 carbons need for transport CAT1 and CAT2 Carnitine inhibited by F.A synthesis *malonyl* and increase in acetyl coA CAT1 bind carnitine with F.A in outer mitochondria transport F.A inside inner mitochondria *Inner mitochondria is impermeable* CAT2 break down CAT1 into carnitine and F.A **Defect in canitine no transport for F.A so no energy caused by 2ry causes: liver diseases and malnutrition and increase in demand> pregnancy 1ry causes: 1-Defect in CPT1 < affect liver Patient has Hypoglycemia < if no carbohydrate in diet 2-Defect in CPT2< affect muscle and heart No energy muscle weakness, cardiomyopathy ^^ Treated by diet with carbohydrate and milk product < if they say milk free is WRONG!! MCAD> defect in first enzyme “dehydrogenases” ^F.A not breakdown < in medium chain Happened in children cause they rely on milk. Treatment carbohydrate diet. F.A oxidation > 129 ATP Refsum diseases: The branched F.A need a-oxidation to break it down ^ If there’s defect on it will lead to toxicity < deafness and blindness Ketones bodies: Synthesis in liver and breakdown in all tissue except liver And synthesis in prolonged fasting and in DM< no insulin, increase in lipolysis. Lec4: Protein degradation by: 1-ubiquitin > need energy, intracellular 2- lysosomes> no need energy, extracellular a.a > remove a-amino group > give ammonia And the remaining carbon skeleton > give energy Transporter for ammonia: What the carrier for ammonia in brain? Glutamine What the carrier for ammonia in muscle? Alanine Transamination reaction not gives free ammonia or free amino group Oxidative deamination done by glutamate dehydrogenase work on glutamate give > free ammonia and a-ketoglutarate Example Q: Oxidative deamination done by? Answer: glutamate dehydrogenase Or amino acid dehydrogenase **Make sure is glutamate not GLUTAMINE. Urea form in liver for disposal ammonia and excretion mainly in urine via kidney And stool and reabsorbed to blood via intestine Hyperammonemia: Acquired: 1-liver diseases 2-GIT bleeding < increase amount of reabsorbed ammonia in blood Heredity: defect in enzymes in urea cycle **Renal failure: Can’t excrete urea in urine so it’ll transfer to intestine that will increase the amount of ammonia absorbed to the blood lead to hyperammonemia For treatment give oral neomycin antibiotic to reduce intestinal Bactria that responsible for production of ammonia