GI – Hesi Review Question - MedSurgFinal
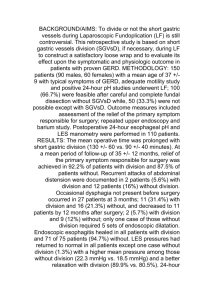
advertisement

Gastrointestinal Disorders N635 Medical Surgical - Disease Management II 02-23-10 Presenters: Maria M. Stone Alicia Talavera Amy Davidson Amanda Durazo Timothy Wong 1 Gastrointestinal Disorders Review at a Glance • Barrett’s epithelium: esophageal epithelial tissue that has undergone change as a result of repeated exposure to gastric juice and is more resistant to erosion, but is premalignant. • Body mass index (BMI): estimates total body fat stores in relation to height and weight. • Bulk-forming agents: high-fiber supplements that increase fecal bulk. • Cholecystitis and Choleithiasis: • • Cholecystitis: an acute inflammation of the gallbladder. Cholelithiasis: The formation or presence of stones in the gallbladder. • Cirrhosis: Degeneration of liver tissue causing enlargement, fibrosis, and scarring. • Crohn’s Disease (Regional Enteritis): Subacute, chronic inflammation extending throughout the entire intestinal mucosa (most frequently found in terminal ileum). • Chyme: stomach contents – partially digested food mixed with gastric juice. 2 Gastrointestinal Disorders Review at a Glance • Colostomy: surgical diversion of large intestine fecal contents to an external collection device. • Diarrhea: increase in frequency, amount or liquidity of stool that is a change from the individual’s normal pattern. • Diverticular Disease: manifested in two clinical forms – 1) Diverticulosis and 2) diverticulitis. 1. 2. Diverticulosis: bulging pouches in the GI wall (diverticula) push the mucosa lining through the surrounding muscle. Diverticulitis: inflamed diverticula, (may cause obstruction, infection, and/or hemorrhage.) • Dumping syndrome: complication of gastric resections where there is a rapid emptying of stomach contents into the jejunum causing physiologic manifestations. • Esophagogastroduodenoscopy (EGD): direct visualization of esophagus, stomach, and duodenum through a fiberoptic endoscope and used to diagnose disorders of aforementioned structures. 3 Gastrointestinal Disorders Review at a Glance - continued • Esophagogastric tube: also known as the Sengstaken-Blakemore and Minnesota tube, consisting of a tube with several lumens used to inflate a gastric balloon, esophageal balloon and drain stomach contents. • Fistula: abnormal pathway been structures or from an internal organ to an outside surface. • Gastroesophageal reflux: the backward flow of gastric contents into the lower portion of the esophagus. • Gavage: referring to intermittent feeding through a tube in the stomach or jejunum. • Hepatitis: Widespread inflammation of liver cells usually caused by a virus. Hernia: referring to a protrusion of an organ through a weakness in muscle. • • Hiatal Hernia: herniation of the stomach and other abdominal viscera through an enlarged esophageal opening in the diaphragm. Etiology unknown. 4 Gastrointestinal Disorders Review at a Glance - continued • Esophagogastroduodenoscopy (EGD): direct visualization of esophagus, stomach, and duodenum. • Ileostomy: surgical diversion of fecal contents at the level of the ileum to an external collection device. • Inflammatory Bowel Diseases: consists of Crohn’s disease and ulcerative colitis. • Intestinal Obstruction: Partial or complete blockage of the intestinal flow (fluids, feces, gas). • Intestinal tube: long tube, 6 to 10 feet in length, used to decompress the intestines. • Lavage: irrigation of the stomach using a tube inserted into the stomach. 5 Gastrointestinal Disorders Review at a Glance - continued • Lower esophageal sphincter (LES): the sphincter located at the esophageal gastric junction. • Nasogastric (NG) tube: a tube inserted through the nose and into the stomach and used to drain contents or for feeding. • Non-steroidal anti-inflammatory drugs (NSAIDs): medications usually used for analgesia and to reduce inflammation. • Pancreatitis: Nonbacterial inflammation of the pancreas. • Peptic Ulcer Disease (PUD): ulceration which penetrates the mucosal wall of the GI tract. • Ulcerative Colitis: disease which affects the superficial mucosa of the colon, causing the bowel to eventually narrow, shorten, and thicken due to muscular hypertrophy. Occurs in the large bowel and rectum. • Zollinger-Ellison syndrome: disorder in which a pancreatic tumor secretes gastrin, which then stimulates secretion of acid and pepsin. 6 Gastrointestinal Disorders Case Study MW, a 47-year-old female, is admitted to the hospital to rule out chronic gastro esophageal reflux disease (GERD) versus peptic ulcer disease (PUD). You are the nurse assigned to care for this client. 1. What diagnostic tests should you anticipate being ordered to differentiate her diagnoses? 7 Gastrointestinal Disorders Case Study – Answer and Rationale • An upper-GI series will probably be ordered and can show lower esophageal sphincter (LES) function as well as ulceration. An esophagogastroduodenoscopy can be more diagnostic because it is a direct visualization of the tissue of the esophagus and can show inflammation. The gastric and duodenal mucosa are also visualized directly and ulcerations are evident. The advantage of endoscopy over an upper-GI series is that tissue samples can be obtained for determining the presence of cancer, Barrett’s epithelium, or H. pylori. Gastric analysis may also be used to determine the pH and acid output of the stomach. 8 Gastrointestinal Disorders Case Study MW, a 47-year-old female, is admitted to the hospital to rule out chronic gastro esophageal reflux disease (GERT) versus peptic ulcer disease (PUD). You are the nurse assigned to care for this client. 1. What are the priorities of care after these tests? 9 Gastrointestinal Disorders Case Study – Answer and Rationale • An upper-GI series usually involves the ingestion of barium, which is constipating. The client should be encouraged to drink fluids and ambulate. Aspiration of barium during the procedure is a possibility, so the nurse should assess lung sounds and monitor for signs of aspiration such as fever, cough, and dyspnea. For the client after esophagogastroduodenoscopy, it is extremely important to assess for return of swallowing and the gag reflex since the throat is anesthetized for the procedure, therefore, general safety measures should be instituted (side rails up, bed in low position). 10 Gastrointestinal Disorders Case Study MW, a 47-year-old female, is admitted to the hospital to rule out chronic gastro esophageal reflux disease (GERT) versus peptic ulcer disease (PUD). You are the nurse assigned to care for this client. 1. What instructions about lifestyle changes should you give MW if she has gastro esophageal reflux disease (GERD)? 11 Gastrointestinal Disorders Case Study – Answer and Rationale • Lifestyle and diet modifications are key to controlling GERD. The client should be instructed to avoid eating within 2 hours of bedtime and should remain in an upright position after eating. Tight clothing (belts, tight waistbands), straining (weight lifting, bending over, lifting heavy objects), and vigorous physical activity increase intraabdominal pressure aggravate GERD and should be avoided. A reduction in dietary fat and an increase in complex carbohydrates encourage more rapid gastric emptying and reduction in symptoms of GERD. The client should be instructed to avoid substances that decrease LES tone such as caffeinated beverages, chocolate, peppermint, spearmint, smoking, and fried foods. The client should be encouraged to elevate the head of the bed about 12 inches to prevent reflux at night 12 Gastrointestinal Disorders Case Study MW, a 47-year-old female, is admitted to the hospital to rule out chronic gastro esophageal reflux disease (GERT) versus peptic ulcer disease (PUD). You are the nurse assigned to care for this client. 1. What instructions about signs and symptoms of complications of GERD and PUD should you provide to MW? 13 Gastrointestinal Disorders Case Study – Answer and Rationale • The complications of GERD are limited to the development of Barrett’s epithelium, cancer, and esophageal stricture. Symptoms include dysphagia, pain, and more systemic symptoms such as fatigue, dyspnea, and activity intolerance. Complications of PUD are perforation, hemorrhage, gastric cancer (gastric ulcer), and pyloric obstruction. The client should be instructed to report any of the following symptoms: vomiting, hematemesis, black tarry stools, pain, rapid heart rate, abdominal rigidity, and fever as they may indicate a complication. 14 Gastrointestinal Disorders Case Study MW, a 47-year-old female, is admitted to the hospital to rule out chronic gastro esophageal reflux disease (GERT) versus peptic ulcer disease (PUD). You are the nurse assigned to care for this client. 1. If MW asks you about the possibility of developing cancer, how would you respond? 15 Gastrointestinal Disorders Case Study – Answer and Rationale • Clients with GERD may develop Barrett’s epithelium and be at a greater risk for cancer if GERD remains untreated, so it is important that the client follow the treatment regimen. If the client has a duodenal ulcer, the risk for developing cancer as a result are minimal; however, there is an increased incidence of gastric cancer in people with gastric ulcers. Continued follow-up is therefore important in this population. 16 Gastrointestinal Disorders HESI Hints • A Fowler’s or semi-Fowler’s position is beneficial in reducing the amount of regurgitation as well as preventing the encroachment of the stomach tissue upward through the opening in the diaphragm. • Stress can cause or exacerbate ulcers. Teach stress reduction methods and encourage those with a family history of ulcers to obtain medical surveillance for ulcer formation. • Clinical manifestations of GI Bleeding: Pallor: conjunctival, mucous membranes, nail beds. Dark tarry stools Bright red or coffee-ground emesis. Abdominal mass or bruit. Decreased BP, rapid pulse, cool extremities • The GI tract usually accounts for only 100 to 200ml fluid loss per day, although it filters up to 8 liters per day. Large fluid losses can occur if vomiting and/or diarrhea exists. • Opiate drugs tend to depress gastric motility. However, they should be given with care, and those receiving them should be closely monitored because distended intestinal wall accompanied by decreased muscle 17 tone may lead to intestinal perforation. ALICIA 18 GI – Hesi Review Question • Which of the following assessments is essential for the nurse to make when caring for a client who has just had an esophagogastroduodenoscopy (EGD)? 1. 2. 3. 4. Auscultate bowel sounds Check gag reflex Monitor gastric pH Measure abdominal girth 19 Answer Answer is 2. • The posterior pharynx is anesthetized for easy passage of the endoscope into the esophagus. The return of the gag reflex indicates that normal function is returning and the client is able to swallow (option 2). Bowel sounds (option 1) and abdominal girth (option 4) are associated with caring for a client with a nasogastric tube in place. Gastric pH (option 3) is related to the client with peptic ulcer disease. 20 GI – Hesi Review Question • The client is admitted to the hospital with ulcerative colitis. The nurse should assess the client for which sign that indicates a complication of the disease? 1. 2. 3. 4. Low hemoglobin and hematocrit Low platelet count Epigastric or right-sided pain following a high-fat meal Presence of fat in the stools 21 Answer Answer is 1. • Hemorrhage and bleeding are a common feature of ulcerative colitis, and over time this can lead to significant loss of RBCs, the client should be assessed for possible anemia (option 1). Steatorrhea is seen in malabsorption syndrome (option 4). Thrombocytopenia may occur if the client is treated with immunosuppressants (option 2) to control the disease. Signs of cholelithiasis are unrelated to ulcerative colitis (option 3). 22 GI – Hesi Review Question • A client is admitted to the hospital with a bowel obstruction. Which of these findings by the nurse would indicate that the obstruction is in the early stages? 1. 2. 3. 4. High-pitched tinkling bowel sounds Low rumbling bowel sounds No bowel sounds auscultated Normal bowel sounds heard in all four quadrants 23 Answer Answer is 1. • Early in a bowel obstruction, the bowel attempts to move the contents past the obstruction, and this is heard as high-pitched tinkling bowel sounds (option 1). As the obstruction progresses, bowel sounds will diminish and may finally become absent (option 3). Bowel sounds in all four quadrants (option 4) and rumbling bowel sounds (option 2) are normal. 24 GI – Hesi Review Question • A client with gastroesophageal reflux disease (GERD) is prescribed famotidine (Pepcid). In order to provide effective teaching, the nurse must include which information about the action of the drug? 1. 2. 3. 4. It improves motility It coats the distal potion of the esophagus It increases the gastric pH It decreases the secretion of gastric acid 25 Answer Answer is 4. • Famotidine is a histamine-2 receptor antagonist and reduces the secretion of gastric acid (option 4). This class of drugs does not have a direct effect on reflux or GI motility. Metoclopramide improves GI motility (option 1). Sucralfate coasts the ulcer (option 2). Antacids neutralize the hydrochloric acid in the stomach (option 3). 26 AMY 27 GI – Hesi Review Question • A 65-year old man presents to the Emergency Department complaining of recurring burning chest pain after eating. His history consists of obesity, type-II diabetes, sedentary behavior, and commonly takes TUMS on a regular basis. As his ED nurse, which nursing diagnosis would be suitable for this patient? 1. 2. 3. 4. At risk for severe pain related to an angina attack. At risk for hyperglycemic hyperosmolar nonketotic syndrome related to poorly controlled diabetes. Deficient knowledge related to GERD. Possible nutritional deficiency related to overuse of antacids. 28 Answer Answer is 3. • Chest pain only after eating is a common complaint of Gastroesophaegeal reflux disease (GERD). Chest pain before eating is related to Peptic Ulcer Disease. Commonly taking TUMS is another indication of acid reflux. 29 GI – Hesi Review Question • Name the three causes of intestinal obstruction. 1. 2. 3. 4. Constipation, neurogenic, and vascular. Mechanical, neurogenic, and vascular. Mechanical, diverticulitis, and vascular. Mechanical, constipation, and diverticulitis. 30 Answer Answer is 2 • The three main causes of intestinal obstruction are due to Mechanical (adhesions, hernias, volvulus [twisting of the gut], intussusceptions, tumors), neurogenic (paralytic illeus, lesions on the spinal cord), and vascular causes (artery occlusions). 31 GI – Hesi Review Question • A patient is being admitted to post-op recovery for a hip replacement. It is 12-hours post-op and she is complaining that she has not eaten in 24 hours and wants some ice cream to soothe her irritated throat. What is the next nursing intervention for this patient? 1. 2. 3. 4. Give her the ice cream right away to soothe her irritated throat and document the amount on her I&O’s. Tell her she cannot have any liquids or food until she ambulates for the first time. Contact doctor to increase IV fluids because her output is decreasing. Ascultate for bowel sounds, if bowel sounds are heard, allow her to eat some ice cream. 32 Answer Answer is 4 • After surgery, it is important to determine if the intestines have begun to move or are still paralytic. The nurse must determine, via auscultation of the abdomen, if bowel sounds have returned. If food and liquid is given too early, an intestinal obstruction may occur. 33 GI – Hesi Review Question • A 45-year old woman presents in your outpatient facility concerned with her family history of colorectal cancer. What interventions would be suitable to suggest for this woman? 1. 2. 3. 4. Eat more cruciferous vegetables. Tell her that there is nothing she can do; this type of cancer cannot be prevented. Decrease fiber intake, and increase more foods from animal sources. Begin colonoscopy examinations every year after 50. 34 Answer Answer is 1 • The only valid answer is to eat more cruciferous vegetables (broccoli, cauliflower, etc…). Preventative screening is important. Rectal examinations should be given every year after age 40, and colonoscopies/sigmoidoscopies should only be given every 3 -5 years after age 50. Fiber intake should increase, and foods from animal sources should decrease for preventive measures. 35 TIMOTHY GI – Hesi Review Question • A client is to receive gavage feeding through a nasogastric (NG) tube. Which of the following nursing actions should be performed to prevent complications? 1. 2. 3. 4. Flush with 20 mL of air Place client in high Fowler’s position Advance tube 1 cm Plug the air vent during feeding Answer Answer is 2. Keeping the client in a high Fowler’s position minimizes the risk of aspiration (option 2). Flushing with air (option 1) will increase abdominal distention and increase discomfort and risk of aspiration. Advancing the tube (option 3) is only relevant if it is a nasoduodenal tube that has not advanced beyond the pylorus. Plugging the air vent (option 4) is unnecessary. Strategy: The NG tube bypasses the oropharynx and the gag reflux, which concludes that the airway is compromised. Select the answer that protects the airway. GI – Hesi Review Question • The nurse should question the client with gastroesophageal reflux disease (GERD) about the use of which type of medications that decrease lower esophageal sphincter (LES) tone? 1. 2. 3. 4. Antidepressants Calcium channel blockers Antiestrogen agents Alpha-adrenergic blocking agents Answer Answer is 2. Many common substances contribute to decreased LES tone including fatty foods, caffeinated beverages, nicotine, betaadrenergic blocking agents, calcium channel blockers (option 2), nitrates, theophylline, alcohol, and anticholinergic drugs. Antidepressants, antiestrogen agents, and alpha adrenergic blockers have no effect on LES tone. Strategy: Identify how the lower esophageal sphincter contributes to the symptoms of GERD and select the drug that increases that effect. GI – Hesi Review Question • The client with irritable bowel syndrome (IBS) asks the nurse what causes the disease. Which of the following response by the nurse would be most appropriate? 1. 2. 3. 4. This is an inflammation of the bowel caused by eating too much roughage. IBS is caused by a stressful lifestyle The cause of this condition if unknown There is thinning of the intestinal mucosa caused by ingestion of gluten Answer Answer is 3. There is no known cause of IBS, and diagnosis is made by excluding all other diseases that cause the symptoms (option 3). There is no inflammation of the bowel (option 1). Some factors exacerbate the symptoms (option 2), including anxiety, fear, stress, depression, some foods (options 1 and 4) and drugs, but these do not cause the disease. Strategy: Know the different forms of inflammatory bowel disease and causative factors vs exacerbating factors. GI – Hesi Review Question • A client with Crohn’s disease (regional enteritis) who is taking sulfasalazine (Azulfidine) asks the nurse why this medication is necessary. When information should the nurse include in her response. 1. 2. 3. 4. The drug decreases abdominal cramping by slowing peristalsis. The drug decreases prostaglandin production in the bowel so it decreases inflammation. The drug inhibits neurotransmission of pain impulses. The drug stimulates the release of endorphins so pain is relieved. Answer Answer is 2. Sulfasalazine is a GI anti-inflammatory medication that exerts its action by decreasing prostaglandin production in the bower (option 2). Peristalsis is decreased by anticholinergic agents (option 1). Analgesics affect pain impulses (options 3 and 4). Strategy: Review the goals of treatment for inflammatory bowel disease and select the answer that directly decreases the inflammatory response. Amanda Question #1 • Colace works by? 1. Stimulating muscles and nerves in the bowels to help move stool along Forming bulk that absorbs liquid to produce a soft bulky stool, stimulating bowel normally by the presence of the bulk Encouraging bowel movements by drawing water into the bowel from surrounding body tissues, providing soft stool mass and increased bowel action 2. 3. Answer is 2 • • Rationale: Colace is a bulk-forming laxative. Nursing Intervention: We should encourage our patients to increase their fluid intake during their use of Colace because water is being lost to the colon. Question #2 • When a client has peptic ulcer disease, the nurse would expect a priority intervention to be? 1. 2. 3. 4. Assisting in inserting a Miller-Abbott tube Assisting in inserting an arterial pressure line Inserting a nasogastric tube Inserting an IV Answer is 3 • • Insert a NG tube Rationale: NG tube needs to be inserted to determine the presence of active GI bleeding. A Miller-Abbott tube is a weighted, mercury-filled ballooned tube used to resolve bowel obstructions. There is no evidence of shock or fluid overload in the client; therefore an arterial line is not indicated and an IV is optional. Question #3 • A 55 year old patient with severe epigastric pain due to acute pancreatitis has been admitted to the hospital. The client’s activity at this time should be? 1. 2. 3. 4. Ambulation as desired Bedrest in supine position Up ad lib and right side-lying position in bed Bedrest in Fowler’s position Answer is 4 • • Bedrest in Fowler’s position Rationale: The pain of pancreatitis is made worse by walking and by laying in the supine position. The client is more comfortable sitting up and leaning forward. Question #4 • A client has had a cystectomy and ureteroileostomy (ileal conduit). The nurse observes this client for complications in the postoperative period. Which of the following symptoms indicates an unexpected outcome and requries priority care? 1. 2. 3. 4. Edema of the stoma Mucus in the drainage appliance Reddness of the stoma Feces in the drainage applance Answer is 4 • • Feces in the drainage appliance Rationale: The ileal conduit procedure incorporates implantation of the ureters into a portion of the ileum which has been resected from its anatomical position and now functions as a reservoir or conduit for urine. Feces should not be draining from the conduit. Edema a red color of the stoma are the expected outcomes in the immediate postop period, as is mucus from the stoma. Question #5 • Most cleft palates are repaired at what age? 1. 2. 3. 4. Immediately after birth 1 to 2 months 3 to 4 months 1 to 2 years Answer is 4 • • 1 to 2 years Rationale: Most surgeons will correct the cleft at 1 to 2 years old before faulty speech patterns develop to take advantage of palatal changes during infancy Question #6 • To clear Dr. B out of the classroom as quickly as possible, so we can all go home, we should have all eaten which food for lunch? 1. 2. 3. 4. Beans Donuts Wine and cheese Pizza Question #6 Answer Do you really need the answer and rationale? We are done people! Let’s go home! Thank you for your participation!! The GI Group