Post Resuscitation Care
Learning outcomes
To understand:
• The need for continued resuscitation after return
of spontaneous circulation
• How to treat the post cardiac arrest syndrome
• How to transfer the patient safely
• The role and limitations of assessing prognosis
after cardiac arrest
Chain of Survival
Post resuscitation care
The goal is to restore:
• Normal cerebral function
• Stable cardiac rhythm
• Adequate organ perfusion
• Quality of life
Post cardiac arrest syndrome
• Post cardiac arrest brain injury:
• Coma, seizures, myoclonus
• Post cardiac arrest myocardial dysfunction
• Systemic ischaemia-reperfusion response
• ‘Sepsis-like’ syndrome
• Persistence of precipitating pathology
Airway and breathing
• Ensure a clear airway, adequate oxygenation and
ventilation
• Consider tracheal intubation, sedation and
controlled ventilation
• Pulse oximetry:
• Aim for SpO2 94 – 98%
• Capnography:
• Aim for normocapnia
• Avoid hyperventilation
Airway and breathing
• Look, listen and feel
• Consider:
•
•
•
•
•
•
Simple/tension pneumothorax
Collapse/consolidation
Bronchial intubation
Pulmonary oedema
Aspiration
Fractured ribs/flail segment
Airway and breathing
• Insert gastric tube to decompress stomach and
improve lung compliance
• Secure airway for transfer
• Consider immediate extubation if patient
breathing and conscious level improves quickly
after ROSC
Circulation
• Pulse and blood pressure
• Peripheral perfusion e.g. capillary refill time
• Right ventricular failure
• Distended neck veins
• Left ventricular failure
• Pulmonary oedema
• ECG monitor and 12-lead ECG
Disability
Neurological assessment:
• Glasgow Coma Scale score
• Pupils
• Limb tone and movement
• Posture
Glasgow Coma Scale score
Glasgow Coma Scale score (GCS 3 – 15)
Eyes (4)
Verbal (5)
6
Motor (6)
Obeys commands
5
Orientated
Localises
4
Spontaneously
Confused
Normal flexion
3
To speech
Inappropriate words
Abnormal flexion
2
To pain
Incomprehensible sounds
Extension
1
Nil
Nil
Nil
Further assessment
History
• Health before the cardiac arrest
• Time delay before resuscitation
• Duration of resuscitation
• Cause of the cardiac arrest
• Family history
Further assessment
Monitoring
•
•
•
•
•
•
•
Vital signs
ECG
Pulse oximetry
Blood pressure e.g. arterial line
Capnography
Urine output
Temperature
Further assessment
Investigations
•
•
•
•
•
•
•
Arterial blood gases
Full blood count
Biochemistry including blood glucose
Troponin
Repeat 12-lead ECG
Chest X-ray
Echocardiography
Chest X-ray
Transfer of the patient
•
•
•
•
•
•
•
•
Discuss with admitting team
Cannulae, drains, tubes secured
Suction
Oxygen supply
Monitoring
Documentation
Reassess before leaving
Talk to family
Out-of-hospital VF arrest associated with
Enteral nutrition
AMI
Insulin
Cooling
Inotropes
Defibrillator
Ventilation
Pacing
IABP
Optimising organ function
Heart
• Post cardiac arrest syndrome
• Ischaemia-reperfusion injury:
• Reversible myocardial dysfunction for 2-3 days
• Arrhythmias
Optimising organ function
Heart
• Poor myocardial function despite optimal filling:
• Echocardiography
• Cardiac output monitoring
• Inotropes and/or balloon pump
• Mean blood pressure to achieve:
• Urine output of 1 ml kg-1 hr-1
• Normalising lactate concentration
Optimising organ function
Brain
• Impaired cerebral autoregulation – maintain
•
•
•
•
•
•
‘normal’ blood pressure
Sedation
Control seizures
Glucose (4-10 mmol l-1)
Normocapnia
Avoid/treat hyperthermia
Consider therapeutic hypothermia
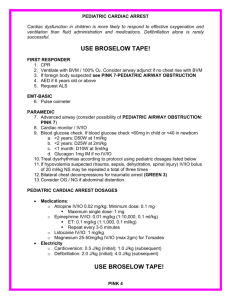
Therapeutic hypothermia
Who to cool?
• Unconscious adults with ROSC after VF arrest should
be cooled to 32-34oC
• May benefit patients after non-shockable/in-hospital
cardiac arrest
• Exclusions: severe sepsis, pre-existing medical
coagulopathy
• Start as soon as possible and continue for 24 h
• Rewarm slowly 0.25oC h-1
Therapeutic hypothermia
How to cool?
• Induction - 30 ml kg-1 4oC IV fluid and/or external
cooling
• Maintenance - external cooling:
• Ice packs, wet towels
• Cooling blankets or pads
• Water circulating gel-coated pads
• Maintenance - internal cooling
• Intravascular heat exchanger
• Cardiopulmonary bypass
Therapeutic hypothermia
Physiological effects and complications
• Shivering: sedate +/- neuromuscular blocking
•
•
•
•
•
•
drug
Bradycardia and cardiovascular instability
Infection
Hyperglycaemia
Electrolyte abnormalities
Increased amylase values
Reduced clearance of drugs
Assessment of prognosis
• No clinical neurological signs can predict outcome
< 24 h after ROSC
• Poor outcome predicted at 3 days by:
• Absent pupil light and corneal reflexes
• Absent or extensor motor response to pain
• But limited data on reliability of these criteria after
therapeutic hypothermia
Organ donation
• Non-surviving post cardiac arrest patient may be
a suitable donor:
• Heart-beating donor (brainstem death)
• Non-heart-beating donor
Any questions?
Summary
• Post cardiac arrest syndrome is complex
• Quality of post resuscitation care influences final
outcome
• Appropriate monitoring, safe transfer and continued
organ support
• Assessment of prognosis is difficult
Advanced Life Support Course
Slide set
All rights reserved
©Australian Resuscitation Council and Resuscitation Council (UK) 2010