Kessler, Edward, B.A., et al. “A demographical study of hyperhidrosis”
advertisement

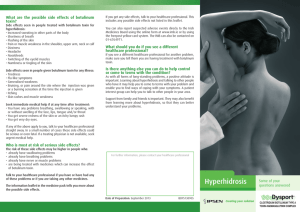
A Demographical Study of Hyperhidrosis Edward Kessler, B.A., Katherine Flanagan, M.D. and Dee Anna Glaser, M.D. Department of Dermatology, Saint Louis University, St. Louis, MO Current knowledge and research on this disease has emphasized treatment, while few studies have described the demographics of this population. 80 70 60 20 10 Sl ee p O Al th l li er st * ed No Fa Kn ct or ow s n Fa ct or s er cis e Ex Percentage 80 60 40 20 0 Palmar Plantar (Soles) Palms and Soles Face and scalp Groin Other significant predisposing factors were family history and the age of onset of HH. Patients who reported the onset of HH prior to the age of 20 years were more likely to have a positive family history of HH than those reporting the onset of HH after the age of 20 years old. Patients who complained of axillary HH (isolated or in addition to other areas) were more likely to have a post-pubertal onset of HH. The postpubertal onset of axillary HH coincided with an age of onset between the ages of 12 to 19 years. Patients presenting with palmoplantar HH were significantly more likely to have a pre-pubertal onset, with an age of onset prior to the age of 12 years. Negative Family History 50% The most common disease pattern was isolated primary axillary HH. An overwhelming majority of our patients were severely affected by hyperhidrosis, rating their condition as 4 out of 4 on the HDSS. 32% The majority (80%) of our patients were considered normal weight, with 16% considered overweight, and the remaining 4% were considered underweight. The preponderance of our patients were Caucasian (86.8%), followed by African-Americans (8.2%), Asians (2.5%), Hispanics (0.8%), and other (1.6%). Patients’ occupations ranged, in order of descending frequency categorically, from students, professionals (finance, law, medicine, sales, education), clerical workers, homemakers, tradespeople (electricians, plumbers, construction workers), retirees, unemployed, and disabled persons. 18% Cross-section of Site(s) of Hyperhidrosis by Age of Onset* Axillary Palmoplantar 0 to 11 years N (%) 51 (20.0) 12 to 19 years N (%) 148 (58) 20 to 53 years N (%) 50 (19.6) 94 (55.3) 59 (34.7) 15 (8.8) Palmar 104 (47.7) 89 (40.8) 23 (10.6) Plantar (Soles) 103 (52.3) 72 (36.5) 20 (10.2) Face 24 (31.6) 33 (43.4) 17 (22.4) Scalp 7 (31.8) 6 (27.3) 8 (36.4) Groin 16 (32.7) 27 (55.1) 6 (12.2) Additional Areas*** 21 (33.3) 27 (42.9) 13 (20.6) Gender Presentation *For each affected site, other sites may also be involved. For those patients with multiple affected sites, age of onset does not specify which site of hyperhidrosis occurred first and which occurred at a later date Male (32.8%) Female (67.2%) *Females were significantly more likely to present for evaluation of HH than males. N on e Unaware of Family History Results Of 515 patients, 67.2% were female and 32.8% were male. The average age of our patients at date of consultation was 27.94 ± 11.82 years with a median age of 25 years. The average age of HH onset was 14.1 ± 7.9 years with a median age of 13.0 years. Two-thirds of patients claimed a post-pubertal onset of HH. Anatomic Sites Axillary HH was the most common presentation in our patients. This may reflect greater media attention and marketing for botulinum toxin A treatment for primary focal axillary HH. A remarkable difference was noted between genders regarding the affected site(s) of presentation. Females were more likely to present with isolated axillary HH. Males were more likely to present with facial HH, which was aggravated significantly more frequently by stress, exercise, and heat than hyperhidrosis of other sites. Age of Onset Patients with onset of HH prior to the age of 12 years were more likely to present with palmoplantar HH. Patients with post-pubertal onset of HH were more likely to present with axillary HH. We anticipated this difference based on the hypothesis that axillary HH is due to dysfunction of the apocrine or apoeccrine glands, which are highly dense in the axillary region and are nonfunctional until puberty (5, 11). Thus, this data suggests that a similar pathophysiology is involved in the development of HH. Family History of Hyperhidrosis Positive Family History The patient population in our study differed with the population described in the US prevalence study by Strutton, et al. by having an earlier age of onset, higher severity rating on the HDSS, higher percentage of axillary disease, and many more past therapies attempted by the time of consultation. This difference between studies may be due to our patients’ greater disease severity which compelled them to seek treatment for their condition. The population described in the US prevalence study by Strutton et al. were assessed through a national survey and likely reflects a less severely affected population. Gender Our study also detected a gender difference in the presentation of HH. Female patients presented for evaluation in much higher frequencies despite past reports of similar prevalence of HH between the sexes. In both this study and the Strutton et al. study, HDSS scores were similar between genders, which suggests that a difference in interpretation of HH severity between males and females was unlikely. This discrepancy may reflect a disparity between females and males in their willingness to consult with a physician. *Each category does not exclude other sites that may also be involved The results were compiled using the Statistical Package for the Social Sciences (SPSS) version 14 and analyzed for descriptive statistics. The data was grouped into nominal categories for all variables, except HDSS and age, which were analyzed as ordinal variables. Chi-square statistics were used to test differences between males and females, age of onset, puberty onset and sites of hyperhidrosis against all other variables. A pvalue of <0.05 was used to determine significance throughout this paper. Percentage Discussion Anatomic Sites of Hyperhidrosis* Axillary The medical records of 515 patients presenting to a midwestern American academic outpatient dermatology clinic between October 1998 and November 2006 for evaluation and treatment of primary focal HH were reviewed. Information collected included the following: gender, sites of hyperhidrosis, age, date of birth, age of onset, aggravating factors, pre- or post-puberty onset, severity of disease on Hyperhidrosis Disease Severity Scale (HDSS), family history, handedness, tobacco or alcohol use, general habitus, occupation, ethnicity, and past treatment. He at ty An xie Objective A lC l B TX -A O th O er ra lA * nt ic Io ho nt l op ho re si s Su rg er y 30 Patients presenting with HH of palms, or soles (plantar), or a combination of palms and soles (palmoplantar) were significantly more likely to list stress and anxiety as aggravating factors compared to patients with other sites of HH. Patients presenting with facial HH were significantly more likely to list stress, exercise, and heat as aggravating factors, and patients with scalp HH listed anxiety as a significantly aggravating factor. Methods 100 80 60 40 20 0 O TC 40 0 To perform a descriptive study of this patient population by identifying common trends and associations of patients presenting with primary focal HH. Past Treatment(s) Tried at Presentation 50 ss Primary HH is a relatively common disorder, affecting nearly 3% of the U.S. population, with the highest prevalence rates among those aged 18 to 64 years. The prevalence rate is the same for males and females (2). The most common sites of primary HH are palms, soles, axillae, face, and scalp (4, 5). Various treatments for primary focal HH exist, ranging from topical treatments, iontophoresis, oral anticholinergics, botulinum toxin injections, and surgery (5, 6, 7, 8). A genetic component may contribute to primary HH as family history has been positive in 30%-65% of patients (5, 9). Aggravating Factors St re Hyperhidrosis (HH) is a disorder characterized by perspiration in excess of the body's physiologic needs. It can significantly impact one's occupational, physical, emotional and social life. HH is categorized as either primary or secondary hyperhidrosis (1,2). Primary focal HH is a chronic, idiopathic disorder of excessive perspiration in a bilateral, symmetrical manner (3). Primary focal HH is associated with hyperactivity of the sympathetic nervous system and can affect one or several areas of the body (2, 3). Secondary HH is due to an underlying condition, such as infection, endocrine disorders, metabolic disorders, neoplastic diseases, neurological conditions, spinal cord injuries, cardiovascular disorders, respiratory disorders, anxiety, and stress (2, 4). The most common aggravating factors reported were stress, anxiety, heat, and exercise. Significant associations were detected between gender and affected site(s). Males were significantly more likely to present with facial HH. Females were significantly more likely to present with isolated axillary HH than males. Otherwise, both genders had similar presentations for sites affected by HH. Percentage Background **Note: Bolded items with single asterisk are statistically significant, with p < 0.05 ***Additional areas include patients presenting with other additional areas of hyperhidrosis (back, chest, abdomen, forearm, and lower extremities) CONCLUSIONS This large descriptive study of patients seeking care of primary focal HH has demonstrated novel findings: • Despite similar disease prevalence between genders, women were significantly more likely to seek medical care for hyperhidrosis than men. • Distinct gender differences exist in the clinical patterns of hyperhidrosis. • Patients seeking medical attention are severely affected by their disease. • Axillary HH is the most common presentation. • An early age of onset correlated with a positive family history. • Patients aged 12 years or under were more likely to present with palmoplantar HH. • Patients over the age of 12 years were more likely to present with axillary HH. Our data offers a unique characterization of the demographic and clinical features of patients seeking treatment for primary HH in a university-based practice, and will hopefully aid management of these patients and the development of future treatments. REFERENCES 1. Lowe N, Campanati A, Bodokh I, et al. The place of botulinum toxin type A in the treatment of focal hyperhidrosis. Br J Dermatology. 151(6):1115-22, 2004 Dec. 2. Strutton DR, Kowalski JW, Glaser DA, Stang PE. US prevalence of hyperhidrosis and impact on individuals with axillary hyperhidrosis: results from a national survey. J Am Acad Derm. 51(2):241-8, 2004 Aug. 3. Hornberger J, Grimes K, Naumann M, et al. Multi-Specialty Working Group on the Recognition, Diagnosis, and Treatment of Primary Focal Hyperhidrosis. Recognition, diagnosis, and treatment of primary focal hyperhidrosis. JAmAcad Derm. 51(2):274-86, 2004 Aug. 4. Eisenach JH, Atkinson JL, Fealey RD. Hyperhidrosis: evolving therapies for a wellestablished phenomenon. Mayo Clinic Proceedings. 80(5):657-66, 2005 May. 5. Haider A, Solish N. Focal hyperhidrosis: diagnosis and management. Canadian Medical Association Journal/Journal de L'Association Medicale Canadienne. 172(1):69-75, 2005 Jan 4. 6. Naumann M, Hamm H. Treatment of axillary hyperhidrosis. Br J Surgery. 89(3):259-61, 2002 Mar. 7. Baumann L, Slezinger A, Halem M, et al. Double-blind, randomized, placebo-controlled pilot study of the safety and efficacy of Myobloc (botulinum toxin type B) for the treatment of palmar hyperhidrosis. Derm Surg 2005; 31(3);263-270. 8. Glogau RG. Treatment of hyperhidrosis with botulinum toxin. Dermatol Clin 2004; 22(2):177-85, vii. 9. Ro KM, Cantor RM, Lange KL, Ahn SS. Palmar hyperhidrosis: evidence of genetic transmission. J Vasc Surg. 35(2):382-6, 2002 Feb. 10. Fronek KS, Schmelz M, Kruger S, et al. Effects of gender and level of surgical sympathetic block on vasoconstrictor function. Clin Auton Res 2003; 13(suppl 1):74-78. 11. Lonsdale-Eccles A, Lawrence C. Axillary hyperhidrosis: eccrine or apocrine? Clinical and Experimental Dermatology. 28(1):2-7, 2003 Jan.