Morbid Obesity
advertisement

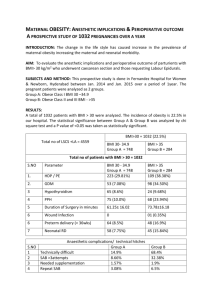
By Prof Dr WALEED IBRAHIM Obesity has been defined as excess body fat relative to lean body mass. The most widely accepted measure of obesity is the body mass index (BMI). BMI= Patient’s weight in kg / square of patient’s height in meters (kg/m²). A normal BMI ranges from 18.5 to 24.9 kg/m² BMI BMI BMI BMI BMI 25-29.9 = overweight. ≥30 = obesity. ≥35 = severe obesity. ≥40 = morbid obesity. ≥45 = super obese. GENETIC ( rare ) A. SYNDROMES INDUCING OBESITY: Prader- Willi : Hypotonia, Hyperphagia, M R, Facial features Laurence- Moon : Ret. Pig, M R , Sp. Pplegia, Hypogonad Bardet-Biedl : Polydactyly, Renal failure B. CHROMOSOMAL DEFECTS: NUTRITIONAL : Intra-uterine, Infancy, Dietary. PHYSICAL INACTIVITY : TV., Internet, Lifestyle, Technology. TRAUMA : NEUROLOGICAL : Post op., Head injuries. PSYCHOLOGICAL : Stresses, Abuse…. MEDICATIONS : Steroids, Psychotropic drugs. SOCIAL : Economic, Ethnic. HYPOTHALAMIC-PITUITARY GONADAL : Polycystic Ovary ADRENAL : Cushing THYROID PANCREATIC : Hyperinsulinaemia COMBINATION OF : OBESITY ( Esp. CENTRAL ) + 2 of : HT. DM. DYSLIPIDEMIA The American Heart Association and the National Heart, Lung, and Blood Institute recommend that the metabolic syndrome be identified as the presence of three or more of: Elevated waist circumference: Men —Equal to or greater than 40 inches (102 cm) Women — Equal to or greater than 35 inches (88 cm) Elevated triglycerides: Equal to or greater than 150 mg/dL Reduced HDL (“good”) cholesterol: Men — Less than 40 mg/dL Women — Less than 50 mg/dL Elevated blood pressure: Equal to or greater than 130/85 mm Hg FBS equal or greater than 100mg/dL Morbidly obese patients are classified according to area of main fat mass: Peripheral (Gynecoid) obesity: associated with degenerative joint disease and venous stasis in the lower extremities. Central (Android) obesity: associated with the highest risk of mortality related problems due to the “Metabolic Syndrome” as well as increased intra-abdominal pressure. 1. 2. 3. 4. Dietary therapy Physical activity therapy Drug therapy Behavioural therapy Candidates for surgery 1) 2) 3) 4) 5) BMI ≤ 40 Kg/m² or ≤ 35 Kg/m² with significant cormobidities. Failure of non surgical weight loss programs. Capability of tolerating surgery. Absence of endocrine disorders that can cause massive obesity. Psychological stability with supportive social environment. 6) 7) 8) 9) 10) Age less than 60 years Basic understanding of how obesity surgery causes weight loss. Realization that surgery itself does not guarantee weight loss Absence of active alcohol and drug abuse. Commitment to post-operative follow up. 1- Restrictive procedures: A)Vertical banded gastroplasty (VBG) B) Adjustable gastric banding (AGB) C) Sleeve Gastrectomy (SG) 2- Malabsorptive procedures : A) Roux en Y Gastric bypass(RYGBP) B) Minigastric bypass The aim of bariatric surgery is to induce weight loss that is sufficient to reduce obesity-related morbidities to acceptable levels. Loss of visceral fat is associated with improved insulin sensitivity and glucose metabolism , also reduces intra-abdominal pressure and this change may result in improvement in urinary incontinence, gastroesophageal reflux, systemic hypertension, venous stasis disease, and hypoventilation. 70-80% IMROVEMENT OF CO-MORBIDITIES : - TYPE 2 DM. - HYPERTESION. - DYSLIPIDAEMIA. - HYPERURICAEMIA. - SLEEP APNOEA. - CARDIAC RISK. - CANCER RISK. - GERD. - PCOS. QUALITY OF LIFE: - SOCIAL. - WORK. - SEXUAL. - PSYCHOLOGICAL IT WAS FOUND THAT THESE POSITIVE CHANGES START (& PERSIST) AS EARLY AS WHEN 10% EWL OCCURS. 1 st, 3 rd,6 th, 12 th MONTH POSTOPERATIVELY, THEN ANNUALLY. DO NOT FORGET: -ELECTROLYTES. -B. SUGAR. -RENAL FUNCTIONS. -LIVER FUNCTIONS. -TRANSFERRIN. - LIPID PROFILE.