Osteoporosis
advertisement

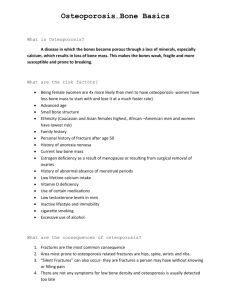
Osteoporosis Dr.Hazar Ibrahim Yacoub Pharmacy College .KSU FACTS AND FIGURES NATIONAL STATISTICS Osteoporosis affects more than 28 million Americans; 80% of them are women and 20% men 1 in 2 women and 1 in 8 men over the age of 50 will develop osteoporosis Thin bones are the cause of 1.5 million fractures a year FLORIDA STATISTICS Over 2.1 million individuals have osteoporosis or low bone mass 1998 - 22,630 residents had hip fractures 1998 - Hospital charges for hip fractures were $477.8 million with 80% discharged to nursing homes VERTEBRAL FRACTURES Can lead to chronic back pain, loss of height, protruding stomach, stooped posture - back pain is the most common complaint At age 50, a woman has a 50% chance of an osteoporosis-related fracture during her life Loss of ability to do daily living activities (cooking, cleaning, getting dressed, etc.) HIP FRACTURES A woman’s hip fracture risk equals her combined risk of breast, uterine and ovarian cancer 15-20% need long-term care facilities There is a 20% increased risk of death during the first year following a hip fracture MYTHS OR FACTS Men do not get osteoporosis Diet can provide all of the calcium a body needs If your grandmother had osteoporosis, you will get it too Dairy products are the only source of calcium Activity – Myths or Facts About Osteoporosis MYTHS OR FACTS If you have osteoporosis, you can do nothing about it Our bones stop growing when we reach full height (about age 20) Susceptibility to fractures can indicate osteoporosis MYTHS OR FACTS Low calcium intake during adolescence can cause osteoporosis later Exercise is dangerous for older people MEN & OSTEOPOROSIS Lifetime risk of getting osteoporosis is the same as a man’s lifetime risk for prostate cancer Nationally, one in eight men over 50 will get osteoporosis By age 75, one in three men will get osteoporosis ALL ABOUT BONES OSTEOPOROSIS: “The Silent Disease” “Osteo” is Latin for “bone” “Porosis” means “porous or full of holes” “Osteoporosis” means “bones that are full of holes” Osteoporosis can develop without symptoms You may not know you have the disease until a bone fractures TYPES OF BONE (1) Cortical – is hard, compact, dense bone (example: midsection of larger, long-bones of arms and legs) (2) Trabecular – is spongy, porous and flexible bone (example: end of the wrist, hip and the spine) Activity - Understanding Our Bones HEALTHY BONE Bone is living tissue, which is constantly being broken down and rebuilt, a process called remodeling Bone is renewed like skin, hair and nails OSTEOPOROTIC BONE The loss of living bone tissue makes bones fragile and more likely to fracture Note: arrow points to micro - fracture BONE “REMODELING” Resorptionremoves old bone Formationreplaces old bone with new bone OSTEOCLASTS-PHASE 1 Cells called osteoclasts (think “C” for chiseler) seek out old bone or damaged bone tissue and destroy it, leaving small spaces (resorption) OSTEOBLASTS – PHASE 2 Cells called osteoblasts (think “B” for builder) use minerals like calcium, phosphorus, and vitamin D to fill in the spaces with new bone (formation) BUILD YOUR BONE BANK You build bone until about age 30 Steps to building healthy bones include: Calcium & vitamin D Limit Caffeine & Alcohol Exercise Don’t Smoke BONE BANK DEPOSITS From birth through adolescence, new bone is built faster than old bone is removed In mid-life, depending on lifestyle and other factors, bone removal can achieve a balance with bone formation After menopause, bone removal may accelerate due to a decrease in estrogen BONE LOSS & AGING The first 5-15 years after menopause a woman can lose approximately 25 - 30 % of trabecular bone & approximately 10 – 15 % of cortical bone Bone loss often occurs without symptoms or warning signs CHANGES IN BONE MASS After menopause, bone removal accelerates due to a decrease in estrogen EARLY WARNING SIGNS History of broken bones as an adult Unexplained back pain – subsides after a couple of weeks Loss of more than an inch in height Posture has become stooped OSTEOPOROSIS Normal Posture Dowager’s Hump CLARIFICATIONS There is no relationship between osteoporosis and arthritis Osteoporosis is a generalized bone disease that causes porous bones, usually not causing symptoms until a fracture occurs CLARIFICATIONS Arthritis refers to a group of diseases and conditions that affect the joints and are usually painful Osteoarthritis is a degenerative type of arthritis affecting the hip, knees and tips of the fingers—no relationship to osteoporosis CLARIFICATIONS Steroids are sometimes used to treat arthritis, and using steroids may put a person at risk for osteoporosis There is no clear relationship between dental cavities and osteoporosis Someone with osteoporosis may have weakened jawbones and be prone to losing teeth RISK FACTORS RISK FACTORS - CAN’T CONTROL Gender: Females are usually diagnosed with osteoporosis at four times the rate of males. Bone mass in males is approximately 15-20% higher than females Small Boned & Thin: may result in smaller bones with a lower bone density Activity - Risk Factor Worksheet RISK FACTORS - CAN’T CONTROL Race/Ethnicity: Women, especially Caucasian and Asian women with thin frames are at greater risk African American women have a higher peak bone mass (10%) than Caucasian women, but other factors such as nutrition, exercise, certain diseases, and medications may increase their risk of osteoporosis RISK FACTORS - CAN’T CONTROL Heredity: your family history may put you genetically at risk or may be a result of family members sharing the same environment, exercise, and nutritional habits Menopause or several months without periods: bone loss begins to exceed bone formation, due to a decrease of estrogen RISK FACTORS - CAN’T CONTROL Age: In your 40’s you start to lose bone faster than you build new bone. The accumulated loss of bone puts an older person at higher risk RISK FACTORS – CAN CONTROL Calcium Rich Diet: milk, cheese, yogurt Weight Bearing Exercise: walk, bike, run Vitamin D: sunshine, multivitamin, fortified food RISK FACTORS – CAN CONTROL Caffeine: RecommendationNo more than 2-3 cups of caffeine beverages per day Cola, coffee and chocolate all contain caffeine RISK FACTORS – CAN CONTROL Alcohol: consuming more than one alcoholic drink per day is associated with risk of low bone mass Eating Disorders: anorexia nervosa or bulimia can lead to malnutrition and bone loss RISK FACTORS – CAN CONTROL Smoking: causes lower bone density Immobility: extreme lack of exercise can lead to bone loss OTHER RISK FACTORS Steroids - cause increased bone breakdown and decreased bone replacement Prolonged hyperthyroidism – can cause increased risk of bone loss Thyroid hormone - (in excess) – acts on bone cells to increase resorption OTHER RISK FACTORS Diuretics – some types of diuretics may increase excretion of calcium in the urine Kidney failure – affects the metabolism of calcium, phosphorous and vitamin D Chronic hepatitis – chronic liver disease may cause bone loss in several different ways Intestinal disease – some can affect the absorption of vitamin D & calcium DRUGS-MAY CAUSE BONE LOSS Cortisone Isoniazid Seizure drugs Lithium Cyclosporine Heparin Methotrexate Some Hormones Lupron® Zoledex® Ask your healthcare provider PREVENTION CALCIUM’S FUNCTION Blood clotting (control bleeding) Regulates heart beat Muscle function Nerve transmission Bone formation DAILY CALCIUM REQUIREMENTS Age 1-3 years 4-8 years 9-18 years 19-50 years over 50 years Milligrams (mg) 500 800 1,300 1,000 1,200- 1,500 National Academy of Science CALCIUM NEEDS Adolescents-may lack calcium due to high fat snacks with empty calories, soda and dieting Eating Disorders-anorexic or bulimic teens lack calcium and may develop osteoporosis at an early age Older Adults-may have increased calcium need due to poor absorption SERVING SIZE 1 ½ cup (12 oz) of liquid is the size of sodapop can 1 cup (8 oz) of food is the size of large handful ½ cup (4 oz) of food is about half a large handful 3 (oz) of cooked meat, fish, poultry is about the size of a deck of cards A serving size is the amount of the food after it is cooked SERVINGS-INCLUDE CALCIUM Food Fat: Serving Sparingly Dairy: 2-3 Protein 2-3 Vegetable: 3-5 Fruit: 2-4 Grains: 6-11 Activity - Calcium Worksheet or Calcium Card Game CALCIUM IN FOODS 1 oz cream cheese: 20 mg 1 hard boiled egg: 30 mg ½ cup cooked broccoli: 40 mg ½ cup cottage cheese: 80 mg 1 oz cheddar cheese: 205 mg 6 oz calcium-fortified OJ: 250 mg 1 cup milk: 300 mg 1 cup fruit yogurt: 345 mg 3 oz sardines with bones: 370 mg 8 oz vegetable lasagna: 450 mg Activity - Results to Calcium Card Game FOOD LABELS Serving size & number of servings Calories, Total & Saturated fat in grams, Cholesterol & Sodium, Fiber, Sugars, & Protein in grams % Daily Value (DV) Daily Amount READING FOOD LABELS Calcium content may vary greatly between different brands of food The percentage of calcium in a food is based on 1000 milligrams. A food containing 20% calcium = 200 mg A food containing 10-19% of calcium is a good source; 20% of calcium or higher is a very good source Activity – Nutrition Facts % DAILY VALUE OF CALCIUM FOOD %DV Fruit yogurt 35% Oatmeal 10% Turnip Greens 20% Total % DV = 65% Add % DV by reading food labels to ensure you get the recommended daily calcium Activity - Foods and Calcium LACTOSE-INTOLERANCE Individuals who have difficulty digesting the sugar found in milk, called lactose Start with small portions of food such as milk--gradually Increase portions Eat dairy foods in combination with other foods Many hard cheeses have less lactose than milk Commercial lactase preparations aid digestion CALCIUM SUPPLEMENTS Read Labels--several different types of calcium supplements available Avoid -“natural” calcium such as bone meal or dolomite-some contain toxic lead or mercury “Elemental calcium” - is the type of calcium the body absorbs ELEMENTAL CALCIUM Kinds of Calcium % Elemental Calcium Calcium carbonate 40% Calcium phosphate (tribasic) 39% Calcium phosphate (dibasic) 30% Calcium citrate 21% Calcium lactate 13% Calcium gluconate 9% Example, a 500 mg calcium tablet may only contain 45-200 mg of elemental calcium CALCIUM TIPS Do not take more than 500 mg of calcium at a time or 2000 mg total per day Your body can absorb only about 500 to 600 mg at a time Example: take one tablet at breakfast and another at dinner CARBONATE CITRATE Needs acid to dissolve and for absorption Doesn’t require stomach acid for absorption Less stomach acid as we age May be taken between meals Take “at” or May cost more “after” meals when more stomach acid TEST YOUR CALCIUM TABLET Put a calcium tablet in a cup of half water and half vinegar. Stir every 5 minutes. If it doesn’t dissolve in 30 minutes, it probably won’t dissolve in your stomach VITAMIN D •Vitamin D is necessary for calcium to be absorbed •Multivitamin or calcium tablets may contain 400 IU daily (don’t exceed 800) •Vitamin D is in milk (100 IU in 1 cup) EXERCISE! Walking Dancing Gardening Tennis Jump Rope Volleyball Skating Activity – Exercise Guide ENVIRONMENTAL SAFETY PREVENT PAINFUL FALLS Activity – Environmental Safety Cartoon BONE DENSITY TESTING WHO NEEDS TESTING? If you have major risk factors for osteoporosis If you have a family history of osteoporosis If you have a personal history of fractures after age 45 If you are on prolonged use of steroids If you are postmenopausal, and not on estrogen replacement therapy Consult your healthcare provider SCREENING TESTS Portable scanners: SXA - (Single Energy X-ray Absorptiometry), measures wrist or heel pDXA - (Peripheral Dual Energy X-ray), measures wrist or heel SCREENING TESTS RA - (Radiographic Absorptiometry), x-ray of hand that is compared to a small metal wedge QCT - (Quantitative Computed Tomography), measures the spine Ultrasound - sound waves to measure the heel, shin, and kneecap DXA-BONE DENSITY TESTING WHAT IS A DXA? DXA (Dual Energy X-ray Absorptiometry) is the “gold standard” Measures bone density in the hip, spine, and forearm Painless, non-invasive, requires no injections Takes 10 - 20 minutes WHAT IS A T-SCORE? World Health Organization T-score is comparing the average bone density to that of healthy young Caucasian women T-Score Diagnosis 0 to –1 “Normal” -1 to –2.5 “Osteopenic”low bone mass -2.5 or lower “Osteoporotic” MEDICATION MEDICATIONS Estrogen - “ERT” Fosamax® - Alendronate Actonel® - Risedronate Evista® - Raloxifene Miacalcin® - Calcitonin ESTROGEN Most cost-effective prevention for osteoporosis Slows bone loss and may slightly increase bone mass Estimated to reduce hip fracture by 30-50% EVISTA (Raloxifene) SERMS-Selective Estrogen Receptor Modulators-designer drugs SERMS act like estrogen but doesn’t stimulate breast or uterine tissue Evista is the first and only SERM approved for the prevention and treatment of osteoporosis BISPHOSPHONATES Fosamax and Actonel Specifically designed to affect the skeleton, increase bone density & reduce number of fractures Must be taken correctly - on an empty stomach, first thing in the morning with glass of plain water, fasting, & remain upright for 30 minutes FOSAMAX ® (Alendronate) Approved for prevention and treatment Approved for treatment of steroidinduced osteoporosis in men and women Prevention – 5 mg daily Treatment – 10 mg daily or 70 mg once weekly (for men and postmenopausal women) ACTONEL ® (Risedronate) Weekly 35 mg is approved for prevention and treatment of osteoporosis in postmenopausal women, and for women who have osteopenia, but are not yet postmenopausal Daily 5 mg dose is approved for prevention and treatment of glucocorticoid-induced osteoporosis in women Actonel may be given to males at the discretion of the Health Care Provider MIACALCIN (Calcitonin) Is a naturally occurring hormone involved in calcium regulation and bone metabolism Available by injection or nasal spray PUTTING IT ALL TOGETHER SUMMARY Calcium Rich Diet Vitamin D Prevent Falls Weight-Bearing Exercise SUMMARY Don’t Smoke Minimize Caffeine & Alcohol Testing & Medication if Needed HEALTHCARE PROVIDERS Healthcare providers are the best source of information about osteoporosis and medical options Activity – Affirming a Positive Change Please complete evaluation form-thank you!