Biological Safety in the Laboratory - Office of the Vice President for
advertisement

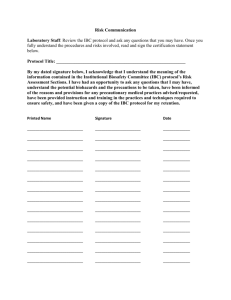
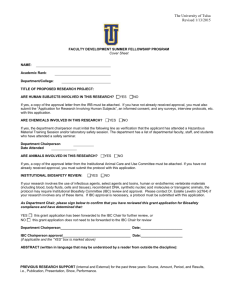
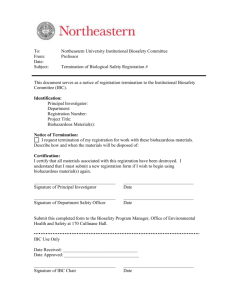
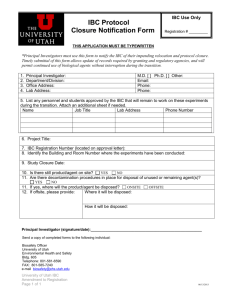
Biological Safety in the Laboratory Robert J. Hashimoto, CBSP The University of Minnesota Minneapolis, Minnesota November 15, 2007 Introduction The purpose of this training session is to familiarize you with the fundamentals of biosafety as it relates to the Office, Vice President of Research and the Department of Environmental Health and Safety. We will discuss: Institutional Biosafety Committee (IBC) Review The elements that are reviewed on the application form including but not limited to: Classification of Agents Risk Assessment/Management Work Practices/Engineering Controls/Personal Protective Equipment The Key Players Biosafety Program Points of Contact Office, Vice-President of Research Melissa Nellis: (612) 626-5892 Julie M. H. Quinn: (612) 626-2161 DEHS Darlene Charboneau: (612) 624-5479 XiaoHong Chen: (612) 624-5495 Claire Kari: (612) 626-2145 IBC Forms The reviews two key forms at a convened meeting: The Recombinant DNA Form, http://www.research.umn.edu/ibc/download/rDNA %20Form.doc The Infectious Agents Form, http://www.research.umn.edu/ibc/download/Infecti ous%20Agent%20Form.doc IBC Forms The submission of the application may require that you write a scope of work and complete templates. Other safety requirements: Section 6-10 on the Recombinant DNA Form Section 6-8.5 on the Infectious Agents Form The remainder of this presentation will discuss the considerations that IBC will review in your application and what you should include on the safety sections of the forms. Review the UMN Biosafety Manual for more information http://www.dehs.umn.edu/bio_pracprin.htm Recombinant DNA Definition Section I-B of the Guidelines In the context of the NIH Guidelines, recombinant DNA molecules are defined as either: molecules that are constructed outside living cells by joining natural or synthetic DNA segments to DNA molecules that can replicate in a living cell, or molecules that result from the replication of those described in (i) above. Infectious Agent Definition Infectious or pathogenic agents capable of causing disease in healthy humans, plants and animals including but not limited to: Bacteria Virus Fungi Parasites Rickettsia Classification of Agents The Centers for Disease Control and Prevention (CDC) in the guideline, Classification of Etiologic Agents on the Basis of Hazard, classify agents on a scale from Class 1 through Class 5. However, the NIH Guidelines cites the World Health Organization Risk Group Classification from Risk Group 1 to Risk Group 4, which will be discussed in the next training session. Risk Assessment Once the investigator has decided on the agent or recombinant molecule, then he or she must conduct an assessment of risk. This assessment shall be based on the following: Virulence/pathogenicity/infectious dose Environmental stability Route of spread, communicability Quantity/concentration/volume used Vaccine/Treatment availability Allergenicity Review Section IX of the UMN Biosafety Manual. Risk Assessment Routes of Exposure The assessment of risk will include common routes of exposure: Parenteral Inoculation (needle stick) Surface Contact (contaminated work area) Ingestion (food in lab) Inhalation (aerosol generating procedures) Mucous Membrane (aerosol droplets in face) The IBC will review the agent usage and determine the most likely routes of exposure (e.g. HIV, bloodborne pathogen-percutaneous) Public Health Agency of Canada MSDS http://www.phac-aspc.gc.ca/msds-ftss/msds84e.html Risk Assessment Experimental Procedures The IBC will also review the application for the procedures performed to assess risk. This includes but is not limited to the following: Handling of sharps Aerosol generating procedures Volume of culture used Transport of agents Use of chemicals and radionuclides Use of animals Any open bench top work Disposal of medical waste Containment The IBC will then evaluate containment of the agents. What is containment? The application of combinations of laboratory practice and procedure, laboratory facilities, and safety equipment when working with potentially infectious microorganisms. Biosafety Levels Containment=biosafety levels. The CDC guideline, Biosafety in Microbiological and Biomedical Laboratories describe four biosafety levels which consist of combinations of laboratory practices, safety equipment and laboratory facilities as well as the CDC hazard classification of the agent and the type of procedures used in the experiment. For recombinant DNA experiments, refer to Appendix G of the NIH Guidelines. Biosafety Level 1 Agent work conducted at Biosafety Level 1 (BL-1) involves little or no known potential hazard to laboratory personnel and the environment. Work is generally conducted on the open bench top and special containment equipment, such as a biosafety cabinet, is not required. E-coli K-12 is an example of a BL-1 organism. Biosafety Level 2 Agent work conducted at Biosafety Level 2 requires that biosafety cabinets are used whenever aerosol generating procedures are performed. Training and handwashing are also required. Access to the laboratory is limited while the experiment is in progress. The Hepatitis B Virus is an example of a BL-2 organism. Biosafety Level 3 Agent work conducted at Biosafety Level 3 is required for agents that may cause serious or lethal disease by the inhalation route. All BL-3 procedures are conducted within a biosafety cabinet; the lab has special engineering features to prevent a release of the BL-3 agent to the environment. Lab workers may need to wear a respirator. Mycobacterium tuberculosis is an example of a BL-3 agent. Biosafety Level 4 Agent work conducted at Biosafety Level 4 is necessary for all work with dangerous and exotic agents which pose a high individual risk of aerosol transmitted laboratory infections and life threatening disease. Lassa Fever Virus is a BL-4 agent. There is currently no Biosafety Level 4 research conducted at the University of Minnesota. Minimization of Risk Once exposure determination has been completed, then ways to minimize risk are evaluated. This includes but is not limited to the following: Work Practices/Engineering Controls Personal Protective Equipment Disinfection/Medical Waste Disposal Medical Surveillance Training (at the laboratory level) Both the investigator and the IBC must review and determine appropriate measures-it is the reason why the application must be completed in detail. Minimize Sharps Usage Needles must not be recapped, bent, sheared or removed from a disposable syringe. All used sharps must be placed in a rigid, hard-plastic, puncture-resistant container for disposal. Substitute plastic for glass whenever possible. Review Section XI of the UMN Biosafety Manual Handwashing Hands should be washed: immediately and thoroughly with a disinfectant hand soap, if contaminated with biological agents. after gloves are compromised or removed with water after a puncture wound If a sink is not available (e.g. equipment room), consider the use of disinfectant towelettes in these areas. Minimize Aerosol Generation To avoid inhalation exposure to agents, workers must minimize the potential generation of aerosols. These procedures include but are not limited to: sonicating centrifuging grinding blending, mixing vortexing Work on the open bench top should be limited whenever conducting these procedures. Review Section XIV-B of the UMN Biosafety Manual Use Biosafety Cabinets Biological safety cabinets are: used for product/personnel protection used for aerosol generating procedures disinfected after use certified annually not recommended for chemical or radioisotope usage. Review Section III of the UMN Biosafety Manual for more information. Use Mechanical Pipettes Mechanical pipetting devices should be used for manipulating all liquids in the laboratory. Never mouth pipet. Decontaminate Work Surfaces Laboratory work surfaces should be decontaminated with an appropriate chemical disinfectant after a spill of biohazardous materials and when work activities are completed. Disinfectant Selection Disinfectants must be selected on a case by case basis to ensure efficiency. Quaternary Ammonia Compounds Chloride Compounds (Bleach) Iodophores (Wescodyne) Phenolics (Amphyl)) Alcohols (70% Ethanol) Formaldehyde/Glutaraldehyde Review Section XVII of the UMN Biosafety Manual for more information. Infectious Waste Disposal Review the Infectious Waste Management Plan in the UMN Biosafety Manual, Chapter XVII-D Ensure that: infectious waste is placed in a red bag lined bin. sharps waste is placed in a sharps container mixed chemical-biological waste is handled as chemical waste mixed radioactive-biological waste is handled as radioactive waste No Eating, Drinking, or Smoking Hand to mouth transmission of disease is a common route of exposure while handling biological agents. Avoid eating, drinking, or smoking in laboratory work areas. Wash hands with disinfectant soap prior to leaving the work area. Do not store or heat/chill food or beverages in the lab. Personal Protective Equipment Use personal protective equipment to prevent skin/mucous membrane exposure during agent use, such as: Gloves Safety glasses/face shield Lab coat Closed toe shoes/foot covers Respiratory protection (BL-3 agents) Review the UMN Biosafety Manual, Chapter XIIIE for more information Hazard Communication Biohazard labels shall be placed on: Biohazard signs shall be placed on: the surface of all equipment (freezers, incubators, refrigerators) which may be contaminated with biohazardous materials. sample transport outer containers. medical waste bins the outer door of BL 2 labs. medical waste storage areas Review Section XIII-B of the UMN Biosafety Manual for more information. Medical Surveillance Requirements-Vaccinations Vaccinations are available for some organisms and should be offered when feasible. However, some members of the population may be at risk for medical complications from the vaccination (e.g., excema-vaccinia vaccinations); therefore it is extremely important that a physician be consulted prior to the administration of any vaccine. Medical Surveillance Some Available Vaccinations Organism Disease Bordetella pertussis Clostridium tetani Corynebacteria diptheriae HBV Influenza Mycobacterium tuberculosis (Bacille Calmette Guerin or BCG) Neisseria meningitidis Polio Virus Rubivirus Salmonella typhi Varicella Zoster Variola major Whooping Cough tetanus diptheria hepatitis Flu -TB meningococcal disease Poliomyelitis Rubella Typhoid Fever Chicken Pox Smallpox Biological Spills If a spill of biological material occurs: Always tend to injured person-Call 911 Notify supervisor and DEHS (626-6002) Initiate clean up procedures Notify the Office of Vice President of Research as a report may need to be sent to NIH OBA. Refer to the UMN Biosafety Manual, Chapter I-C Emergency Procedures needlestick, surface exposure wash your skin with soap and water. Review Section I-D of the UMN Biosafety Manual splash in the eyes wash at an eyewash for 15 minutes. Other injury Call 911 The IBC Application Process The Correct Form Required Templates Frequently Asked Questions The IBC Application Process To initiate the review process, University of Minnesota researchers must submit an IBC application form to the IBC Office. Obtain the appropriate form based on your work: Recombinant DNA and gene transfer form Infectious Agents Form Biological Toxin Form IBC approval is required PRIOR to the initiation of experimental procedures. The IBC Application Process In addition to the appropriate application form, the following items must accompany the completed form: Decontamination and Spill Cleanup Template Biological Waste Disposal Other Required Attachments Requested in the Application or information requested by the IBC upon review of the application form. The IBC Application Process All submissions must be sent electronically to ibc@umn.edu from the Principal Investigator's email account. Projects are reviewed by the Institutional Biosafety Committee. The IBC meets once a month to review projects. The Committee may request modification of procedures and may direct the Biosafety Officer to inspect labs or other facilities. An electronic approval letter will be sent to the Principal Investigator when all requirements have been met. The IBC Application Process Things to Remember Q: How long will the IBC approval process take? A: If an application is received on or before a submission deadline, it will be reviewed at the next IBC meeting, which falls approximately two weeks after the deadline. The Principal Investigator will receive notice of the meeting results approximately 7-10 business days after the meeting. Projects that are assigned stipulations will take an additional amount of time, depending on how quickly the stipulations are met and when they can be reviewed, either by the Biosafety Officer or by the full committee. The IBC Application Process Things to Remember Q: How should you respond to stipulations from the IBC? A: Responses to IBC stipulations should be submitted electronically to ibc@umn.edu. Please submit your response in the form of a letter, addressing each point in the order in which they are presented in the stipulations letter from the IBC. Responses to stipulations should be attached as a Microsoft Word document or PDF and sent directly from the Principal Investigator’s University of Minnesota e-mail account. The IBC Application Process Things to Remember Q: Does research that is exempt from the NIH Guidelines for Research Involving Recombinant DNA Molecules require IBC review? A: Yes, the University of Minnesota Board of Regents Policy requires that University faculty, staff and students using any potentially hazardous biological agents (recombinant DNA, infectious agents and/or biologically-derived toxins) in research or teaching activities apply to the IBC. Even if recombinant DNA activities are exempt according to Section III-F of the NIH Guidelines, the activities must be reviewed by the IBC. The IBC Application Process Things to Remember Q: In what order should I submit my IACUC and IBC applications? A: There is no prescribed requirement for the order in which IACUC and IBC application are submitted; however, IACUC final approval will not be granted until IBC approval has been received. It is advisable to submit your IBC proposal either before or at the same time as when you submit your IACUC proposal to avoid delays. You need a separate form submitted to each committee as each committee reviews different issues. Accident Reporting Accident reporting is critical for several reasons: Risk management Reporting to local regulatory agencies (e.g. Department of Public Health) IBC NIH obligations whenever recombinant DNA molecules are involved Serious adverse events-human subjects The Principal Investigator must report accidents involving biological agents and recombinant DNA to the IBC and DEHS within 24 hours. The Office of Vice President for Research and DEHS will determine who may need to be notified. Conclusion The University of Minnesota Department of Environmental Health and Safety and the Office of the Vice President of Research jointly participate in the review of biological research. If you must perform experiments with recombinant DNA or infectious agents, please remember the following: Conclusion Go on-line to download the appropriate forms and safety templates; Allow sufficient time for the appropriate institutional committees to review your work; Ensure that the form has adequate information for the IBC to assess your workinclude the safety considerations and assessment of risk pertinent to the agent or recombinant molecule that you are using. Conclusion If you have any questions on the administrative process of IBC approval, please contact Melissa Nellis (626-5892) If you have any questions on biosafety containment or DEHS related safety issues, please contact Darlene Charboneau (6245479).