Risk factors for stillbirth
advertisement

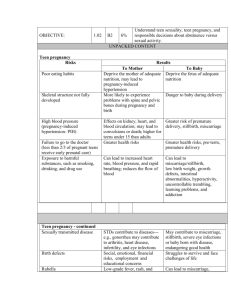
Stillbirth: risk factors and opportunities for prevention Vicki Flenady PhD, MMedSc (Clin Epi & Biostats) Mater Research Institute, University of Queensland Content • • • • Brief overview of global picture High income country picture – focussing on risk factor The Lancet’s stillbirth series key recommendations Stillbirth research initiatives in Australia and New Zealand Launch April 2011 Australia London New York Geneva New Delhi Florence, Italy Cape Town All papers can be accessed free at www.lancet.com/series/stillbirth “These papers, like no other Lancet Series before, have triggered a remarkable response not just from academia and organisations, but also from the public” The Lancet editors Global burden of stillbirth 2.65 million third trimester stillbirths each year 10 countries account for 66% of the world’s stillbirths – and also 66% of neonatal deaths and over 60% of maternal deaths 1. India 2. Pakistan 3. Nigeria 4. China 5. Bangladesh 6. Dem Rep Congo 7. Ethiopia 8. Indonesia 9. Tanzania 10. Afghanistan 98% of stillbirths occur in low-income and middle-income countries – Source: Lawn JE, Blencowe H, Pattinson R, et al, for The Lancet’s Stillbirths Series steering committee. Stillbirths: Where? When? Why? How to make the data count? Lancet 2011; published online April 14. thirds DOI:10.1016/S0140-6736(10)62187-3. more than two are in rural families. Stillbirths don’t count … 1. Global data NOT routinely reported to World Health Organization NOT included in the Global Burden of Disease metrics NOT measured appropriately in most national surveys 2. Global goals eg Millennium Development Goals (MDGs) Stillbirths NOT counted in the MDGs although intimately linked to: • Maternal health in MDG 5 • Neonatal deaths, accounting for 41% of child deaths in MDG4 • Poverty (MDG 1) and girls’ education (MDG2) Stillbirths often missed in national or international health policy and programmes … Yet they count for families Reality for families Giovanni Presutti CiaoLapo Over 7200 families a day experience a stillbirth late in pregnancy… In Australia over 2000 stillbirths each year: 7 every day (I in 130 women) Whether they are famous or not, in a rich country or poor, the grief is overwhelming, and usually hidden Sands UK Goal by 2020 Countries with a current stillbirth rate of less than 5 per 1000 births, the goal by 2020 is to eliminate all preventable stillbirths and close equity gaps. PMNCH Countries with a current stillbirth rate of more than 5 per 1000 births to reduce their stillbirth rates by at least 50% from the 2008 rates. www.thelancet.com/series/stillbirth Stillbirths during labour – 1.2 million a year The risk of stillbirth during labour (intrapartum) for an African woman is 50 times higher than for a woman in the UK/ANZ. Source: Lawn JE, Blencowe H, Pattinson R, et al, for The Lancet’s Stillbirths Series steering committee. Stillbirths: Where? When? Why? How to 55% of2011; allpublished stillbirths are14.for rural families in Africa, South Asia make the data count? Lancet online April DOI:10.1016/S0140-6736(10)62187-3. Stalled progress in high income countries Stillbirth rates halved 1950-1975 with improvements in infection treatment and obstetric –The rates have now stalled Source: Goldenberg RL, McClure EM, Bhutta ZA,care et al, for Lancet’s Stillbirths Series steering committee. Stillbirths: the vision for 2020. Lancet 2011; Stillbirths at 28 weeks or more in high-income settings Differences between countries and within countries show that more Source: Flenady V, Middleton P, Smith GC, et al, for The Lancet’s Stillbirths Series steering committee. Stillbirths: the way forward in highreduction rates is achievable income countries. Lancet 2011; published online Aprilin 14.stillbirth DOI:10.1016/S0140-6736(11)60064-0. Late gestation (>28weeks) stillbirth rates per 1000 births of 193 countries (Cousens et al., 2011) Australia 2.9 (ranked 15) New Zealand 3.5 (ranked 34) If Australia and New Zealand achieved the stillbirth rate of the best performing country, 368 stillbirths would be avoided each year Finland 2.0 (ranked 1) Germany USA UK France 2.4 (ranked 6) 3.0 (ranked 17) 3.5 (ranked 33) 3.9 (ranked 41) Potentially Modifiable Risk Factors for Stillbirth in HIC? Maternal characteristics • Maternal/ paternal age • BMI • Smoking • Parity • Ethnicity • SES & education Adequacy of antenatal care Inter-pregnancy interval Substance use Alcohol intake Coffee consumption Consanguinity Stress Medical conditions • Diabetes • Hypertensive disease Pregnancy factors • Post-term pregnancy • Multiple pregnancy • ART conceptions Pregnancy complications • FGR & SGA • Birthweight Previous stillbirth Previous caesarean section Other previous pregnancy complications Methodology Study selection: Recent, population based studies (1998-Dec 2009) 19,126 studies reviewed HIC settings 75 included Stillbirth definition of ≥20 weeks or ≥ 400 grams Multivariate analysis controlling for important confounders (i.e. age, BMI, smoking, medical conditions etc) Quality appraisal: Newcastle-Ottawa Scale (NOS) for cohorts and case-controls (Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M & Tugwell P, 2003). Data analysis: Random effect meta-analysis (where appropriate) Population attributable risk (PAR%) PAR = Pe (RRe-1) / 1 + Pe (RRe-1) Maternal age > 35 years Prevalence 22% PAR 11% Prevalence 0.5% Previous stillbirth PAR 0.8% Potentially Modifiable Risk Factors for Stillbirth in HIC Maternal overweight & obesity: BMI 25-30 & >30 PAR 12%: OR 1.23, 1.63 (Prevalence 40%) (8000 stillbirths each year) 30% of all stillbirths Maternal age > 35 years: PAR 11%, OR 1.65 (Prevalence 22%) (4000 stillbirths) Smoking: PAR 6%; OR 1.36; (Prevalence 17%) (3000 stillbirths) Population attributable risk (PAR) Estimates for maternal demographics Factor aOR 95% CI Prev % PAR% Any (<28 wk stillbirth) (single study) 1.8 1.3-2.3 50 17 1 – 3 per week 1.1 1.0- 1.2 >5 per week 1.7 1.0-3.0 Binge 1.5 1.0-2.0 Low socio-economic status (SES) 1.2 1.01-1.4 49.6 9 Low education (<10 or <8yrs) 1.7 1.4-2.0 6.9 5 Illicit drug use 1.9 1.2-3.0 2.4 2 Assisted Reproductive Technology (ART) use 2.7 1.6-4.7 3.1 3 No antenatal care 3.3 3.1-3.6 0.3 1 Caffeine intake >8 cups (SB 20-27 weeks) 2.3 1.3-3.9 Paternal age > 50 years 3.9 1.1-13.8 Alcohol use Population attributable risk (PAR) Estimates for medical/pregnancy complications Factor aOR 95% CI Prev % PAR% Small for gestational age (SGA) <10% 3.8 2.3-6.3 10.0 23 Placental abruption 18.9 16.9-12.2 1 15 Pre-existing hypertension 2.6 2.1-3.1 4.6 7 Pre-existing diabetes 2.9 2.1-4.1 2.6 5 Pre-eclampsia 1.5 1.1-2.0 5.3 3 Multiple pregnancy (any) 2.9 2.5-3.4 2 3 Pregnancy induced hypertension (PIH) 1.3 1.2-1.6 6.3 2 Multiple pregnancy (twins) 1.6 1.4-1.9 2 1 Pregnancy prolongation (≥42 weeks) 1.3 1.1-1.7 0.9 0.3 Eclampsia 2.2 1.5-3.2 0.1 0.1 Population attributable risk (PAR) Estimates for previous pregnancy history Factor aOR 95% CI Prev % PAR% Primiparity 1.4 1.3-1.5 42 14 Caesarean section (contentious) 1.3 1.1-1.52 27 7 Stillbirth 2.7 1.6-4.6 0.5 1 SGA + PTB (any) 2.1 1.6-2.8 SGA + PTB 32-36 weeks 3.4 2.1-5.6 SGA+ PTB <32 weeks 5.0 2.5-9.8 SGA + preterm birth (PTB) Late gestation (>28weeks) stillbirth rates per 1000 births of 193 countries (Cousens et al., 2011) Australia 2.9 (ranked 15) Indigenous 3.5 (ranked 34) Australians Ranked 56th behind Colombia and Malaysia New Zealand Finland 2.0 (ranked 1) Germany USA UK France 2.4 (ranked 6) 3.0 (ranked 17) 3.5 (ranked 33) 3.9 (ranked 41) Indigenous status and stillbirth adjusted analysis Subgroup analysis: ethnic minorities PAR% Risk factor aOR AU Indig PAR % Smoking (any) 1.7 26% 29% 13% 5% (14-37) (16-40) (6-19) (3-9) 13% 12% (9-17) (9-16) - - Heavy smoking (10+) 1.9 CA Indig PAR% US Indig PAR% US Afr Am PAR % Overweight 1.3 15% 23% 21% 25% Obesity 1.9 (8-22) (13-32) (12-29) (15-35) Diabetes 2.9 - - - (3-8) Hazardous alcohol use 1.7 10% No antenatal care 3.3 - 8% 5% (7-8) (5-6) 5% (0-24) 8% (7-9) Contributory factors and potentially avoidable perinatal related deaths 2010 Action priorities in high-income countries − Reduce inequity, intentionally designing policies and programs to reach underserved women from poorer communities or ethnic minorities − Address lifestyle risk factors such as obesity, smoking, and advanced maternal age − Improve data quality, Implementation high quality investigation and perinatal audit linked to practice change − Improve detection of pregnancies at increased risk eg placental dysfunction and fetal growth restriction Decreased fetal movements ranked in the top 10 research priorities Stillbirths by PSANZ PDC, QLD 2000-2008 Unexplored not explained Unexplained stillbirth: possible 13% Unknown 7% Congenital abnormality 20% Hypertension 3% Unexplained stillbirth: 7% Maternal conditions 6% Spontaneous preterm unknown chorio 4% Specific perinatal conditions 5% Spontaneous preterm no chorio 3% Spontaneous preterm chorio 8% Perinatal infection 2% Placenta: Insufficiency 7% Hypoxic peripartum death 2% Placenta: Other 6% Placenta: APH 7% ANZ Autopsy rates Autopsy Rates in Australia and New Zealand 80.00% Autopsy Rate 70.00% 60.00% 50.00% 40.00% 30.00% 20.00% 10.00% 0.00% WA SA Perinatal Mortality autopsy rate Stillbirth autopsy rate Neonatal death autopsy rate ACT NZ TAS Region VIC NSW QLD NT Perinatal Society of Australia and New Zealand Guidelines Promoting a systematic approach to clinical care, including audit, around the time of a perinatal death. • • • • • • Institutional Perinatal Mortality Audit Investigation of stillbirth Investigation of neonatal death Autopsy Perinatal Mortality Classification Psychological and social aspects of bereavement care IMPROVE (IMproving Perinatal Mortality Review & Outcomes Via Education) Program Station 1: Communicating with parents about perinatal autopsy Station 6: Psychological and social aspects of perinatal bereavement Study Guide Station 2: Autopsy and placental examination Teaching Stations Formative Assessment Station 5: Audit and classification of perinatal death SCORPIO Methodology: D.A. Hill, Medical Teacher. 1992; 14: 37-41 Station 4: Examination of babies who die in the perinatal period Station 3: Investigation of perinatal deaths National Perinatal Death Clinical Audit Tool On-line: A platform for audit and research 1. Effective online data collection tool for maternity hospitals 2. Includes stillbirth and neonatal deaths 3. Reports automatically generated for Hospital and Health Department reporting of perinatal deaths National prospective perinatal death data collection: Audit and research 30 maternity hospitals IMPROVE workshops First study: Stillbirth investigation and causes; 1,000 stillbirths – causes, contributing factors, yield of tests, costs Decreased fetal movements − Possible adaptive response to placental dysfunction − DFM is associated with a doubling of the risk of FGR (Flenady 2011) − Women who reported DFM (and came to hospital with a live baby) had 4 times the risk of stillbirth compared with women who did not report DFM (Flenady 2011) − Women perceiving a reduction in strength of fetal movements had twice the risk of stillbirth (Stacey 2010) DFM Reporting and Practice in Australia and New Zealand Women: − 50% wait 24 hours or more to report DFM − 60% say it is normal for movements to decrease towards term − 70% indicate awareness of FM would NOT help identify a baby at risk Obstetricians and Midwives: − asking women about FM is important − define DFM most commonly by maternal perception of DFM − lack of clinical practice guidelines − For women with DFM : − Suggest drink some cold/iced water − Low level of ultrasound scan (< 10%) Evidence for raising awareness (+/- kick counting) Cochrane systematic review of Kick Counting: INSUFFICIENT EVIDENCE Grant trial- large Cluster RCT, methodological flaws Lowered stillbirth rate after 28 weeks by 30% DFM Guidelines in Australia and New Zealand − All pregnant women should be routinely provided verbal and written information about normal FM − All women should be advised to contact their health care provider if they have any concern about decreased or absent FM and be advised not to wait until the next day − Maternal concern of DFM overrides any other definition − Women should be assessed within 12 hours of reporting DFM; CTG, clinical assessment of fetal growth, risk factor − USS if risk factors present or clinical concerns (managed a high-risk pregnancy) DFM Information for women Translations: Korean, Arabic, Spanish, Hindi, Vietnamese, Chinese Simplified & Traditional My Baby’s Movements Trial Smartphone Tool − User-controlled − Information about fetal movements and what to expect as pregnancy progresses − Incudes daily fetal movement prompt (time chosen by woman) − Includes movement monitoring option if concerned about fetal movements − Designed to be supportive and non-directive, and minimise unnecessary anxiety and to respect women’s right to autonomy My Baby’s Movements Trial Primary outcome: Stillbirth 28 weeks or more Randomisation: Assigned to timing of intervention using computergenerated random number table Implementation schedule: 9 time periods of 4 months over 36months with groups of 3-4 hospitals in each group 27 hospitals of 3000 births/year over a 3 year period Biophysical and biochemical tests to predict stillbirth Low predictive accuracy : fetoplacental proteins, first- and second-trimester screening for Down syndrome, multivariable prediction models, uterine artery Doppler velocimetry, nuchal translucency, fetal growth, flow in ductus venosus, thyroid function-related tests, maternal hemoglobin levels, and cervicovaginal infection had a low predictive accuracy for stillbirth Moderate to high predictive for stillbirth placental conditions: A pulsatility index in the uterine arteries >90th percentile and low levels of pregnancy associated plasma protein A (PAPP-A) had a moderate to high predictive accuracy for stillbirth related to placental abruption, small for gestational age or preeclampsia Emerging evidence microRNAs derived from the placenta circulate in the maternal blood during pregnancy and may serve as non-invasive biomarkers for pregnancy complications. Summary • Maternal overweight and obesity, smoking and advanced age are important potentially avoidable risk factors • Primiparity is an important risk factor. With increasing incidence of combined risk factors – stillbirth rates could increase • Abruption, Diabetes and Hypertension remain important factors in stillbirth • Must improve data quality including clinical audit linked to practice change • Research to improve detection of women at risk in the antenatal period is a priority Acknowledgements The Lancet's Stillbirth Series Steering Committee J Frederik Frøen, Joy Lawn, Zulfiqar Bhutta, Robert Pattinson, Vicki Flenady, Robert Goldenberg, Monir Islam MBM Trial Investigators Glenn Gardener, David Ellwood, Philippa Middleton, Michael Coory, Caroline Crowther, Christine East, Emily Callander, Frances Boyle, Adrian Charles, Adrienne Gordon, Alison Kent, Belinda Jennings, Deborah Schofield, Glyn Teale, Jonathan Morris, Kassam Mahomed, Susan Vlack, Jane Norman, Fredrik Frøen, International Collaborators Ruth Fretts, Fredrik Frøen, Alex Haezell; Jane Norman ANZSA Researchers Aleena Wojcieszek, Annie McArdle, Cate Nagal, Ann Peacock, Paula Dillon, Debra Creedy, Jenny Gamble, Jocelyn Toohil, Tomasina Stacey, Kassam Mahomen, Julie MacPhail, Glenn Gardener, Yogesh Chadha, Ibi Ibiebele, Laura Koopmans, Dom Rossouw, Kristen Gibbons, Peter Gray Professor Michael Humphrey Queensland Maternal Perinatal Quality Council We also thank the women and clinicians who contributed data Acknowledgements Collaborators ANZSA Consortium hospitals and investigators QLD: Gold Coast Hospital, Anne Sneddon; Ipswich Hospital, Kassam Mahomed; Nambour Hospital, Ted Weaver; Caboolture Hospital, Kate Kerridge; Cairns Base Hospital, Paul Howat; Logan Hospital, Janet Draper; Townville Hospital, David Watson and Anne-Maree Lawrence; Mater Mother’s Hospital Public, Mater Mother’s Hospital Private, Glenn Gardener; Royal Women’s Hospital Yogesh Chadha. NSW: Nepean Hospital, Michael Peek; Royal Prince Alfred Hospital, Sydney; Royal Hospital for Women, Leo Leader; Royal North Shore Hospital, Jonathan Morris. VIC: Sunshine Hospital, Glyn Teale; Mercy Hospital, Robyn Aldridge; Kasey and Dandenong Hospitals, Monash Medical Centre, Chris East; Royal Women’s Hospital Melbourne, Fiona Cullinane; Mercy Hospital for Women, Sue Walker. WA: King Edward Memorial, Adrian Charles and Belinda Jennings. SA: Women’s and Children’s Hospital, Rodney Petersen. NZ: Auckland City Hospital, Peter Stone and Nick Waller; Middlemore Hospital, Dr Graham Parry. Thank you Vicki Flenady vflenady@mmri.mater.org.au