Phase III RECOURSE slides
advertisement

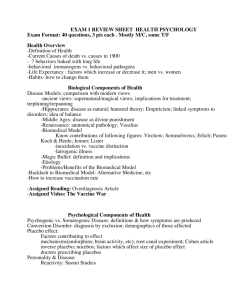
Results of a multicenter, randomized, doubleblind, phase III study of TAS-102 plus best supportive care (BSC) versus placebo plus BSC in patients with metastatic colorectal cancer (mCRC) refractory to standard therapies (RECOURSE) Takayuki Yoshino, M. D. National Cancer Center Hospital East Chiba, Japan Robert Mayer, Alfredo Falcone, Atsushi Ohtsu, Rocio Garcia-Carbonero, Nobuyuki Mizunuma, Kentaro Yamazaki, Yasuhiro Shimada, Josep Tabernero, Yoshito Komatsu, Alberto Sobrero, Eveline Boucher, Marc Peeters, Ben Tran, Heinz-Josef Lenz, Alberto Zaniboni, Howard Hochster, Fabio Benedetti, Manuel Aivado, Lukas Makris, Masanobu Ito, Eric Van Cutsem, and the RECOURSE study Group Conflict of Interest Disclosure • The presenter has no conflicts of interest associated with this trial TAS-102; Mechanism of Action TPase F3dThd (FTD) Inhibition of tumor growth FTY (inactive form) TPI F3dTMP F3dTDP TAS-102 DNA dysfunction (Oral Combination Drug) FTD TPI F3dTTP FTD incorporation into DNA Molar ratio = 1 : 0.5 FTD:Trifluridine TPI:Tipiracil-HCl Differentiation between 5-FU and TAS-102 5-FU TAS-102 5-FU FTD FdUMP F3dTMP F3dTDP Phosphorylation F3dTTP Inhibit Incorporation into DNA TS dUMP DNA duplication dTMP dTTP Inhibit DNA duplication DNA damage FTD T T Thymidine(T) Preclinical Results with TAS-102 • In pre-clinical studies, TAS-102 was effective against cell lines with acquired resistance to 5-FU 1 • In an animal study, co-administration with TPI increased the plasma AUC of FTD by 100-fold 2 • In Xenograft Models, the anti-tumor effect of TAS-102 appeared to occur through FTD incorporation into DNA 3 ; incorporation of FTD into DNA was 700-fold greater than that of 2’-deoxy-5fluorouridine (FdUrd) 4 • 5-FU, capecitabine, S-1, and UFT work primarily by inhibiting thymidylate synthase whereas TAS-102, while structurally similar, acts as an antimetabolite (i.e., incorporated into DNA) 1. Emura T, et al., Int J Mol. Med. 2004:545-49 2. Emura T, et al., Int J Oncol. 2005;27:449-55 3. Tanaka N, et al., AACR 2012 (Abstr 1783) 4. Data on file Clinical Rationale for TAS-102 in mCRC: Phase I and Phase II Experiences • Japanese Randomized Phase II trial for Patients with mCRC 1: – Total 172 patients, who received all of prior fluoropyrimidine, irinotecan and oxaliplatin, were randomized – The median OS was 9.0 vs. 6.6 months (HR=0.56 p=0.0011) – The most common grade 3 or 4 toxicity was hematological toxicity The recommended dose (RD) was determined to be 35 mg/m2/dose orally twice daily 2,3 1. Yoshino T, Ohtsu A, et al., Lancet Oncol. 2012;13(10):993-1001 2. Doi T, Ohtsu A, Yoshino T, et al., Br J Cancer 2012;107(3):429-34 3. Patel M, Bendell J, Mayer RJ, et al., J Clin Oncol 2012; 30 (suppl; abstr 3631) Global Randomized Phase III study RECOURSE: Refractory Colorectal Cancer Study (NCT01607957) Metastatic colorectal cancer (mCRC) • 2 or more prior regimens • Refractory / Intolerable – fluoropyrimidine – irinotecan – oxaliplatin – bevacizumab – anti-EGFR if wild-type KRAS • ECOG PS 0-1 • Age ≥ 18 (target sample size: 800) R A N D O M I Z A T I O N TAS-102 + BSC (n = 534) 35 mg/m2 b.i.d. p.o. d1-5, 8-12 q4wks 2:1 Placebo + BSC Endpoints Primary: OS Secondary: PFS, Safety, Tolerability, TTF, ORR, DCR, DoR, Subgroup by KRAS (OS and PFS) (n = 266) d1-5, 8-12 q4wks • • Treatment continuation until progression, intolerant toxicity or patient refusal Multicenter, randomized, double-blind, placebo-controlled, phase III – Stratification: KRAS status, time from diagnosis of metastatic disease, geographical region • • Sites: 13 countries, 114 sites Enrollment: June 2012 to October 2013 RECOURSE: Endpoints Primary Endpoint: Overall Survival (OS) – OS comparison between the two treatment arms are based on the intent-to-treat (ITT) population – Designed to detect an OS hazard ratio of 0.75 (25% risk reduction), with a 1-sided type I error of 0.025, 90% power – A target of 571 events was required – Planned sample size was 800 Key Secondary Endpoints – – – – Progression Free Survival (PFS) Overall Response Rate (ORR) Disease Control Rate (DCR) Safety RECOURSE: Key Eligibility • Histologically or cytologically confirmed adenocarcinoma of the colon or rectum • Received at least 2 prior regimens of standard chemotherapies for mCRC and is refractory to or failing those chemotherapies – Patients who have progressed based on imaging during or within 3 months of the last administration of each standard chemotherapy, including fluoropyrimidines, irinotecan, oxaliplatin, bevacizumab, and cetuximab/panitumumab for wild-type KRAS patients – Patients who discontinued a treatment due to intolerance to that therapy were also eligible • ECOG performance status 0-1 Patient Demographics and Characteristics (Intent-to-treat population) TAS-102 N=534 Placebo N=266 63.0 (27-82) 63.0 (27-82) Male 61.0 62.0 Female 39.0 38.0 White 57.3 58.3 Asian 34.5 35.3 Black 0.7 1.9 Japan 33.3 33.1 Western 66.7 66.9 Europe 50.7 49.6 US 12.0 13.2 3.9 4.1 0 56.4 55.3 1 43.6 44.7 Age, median (range) Gender, % Race, % Geographic Region, % Australia ECOG PS, % Patient Disease Characteristics (Intent-to-treat population) TAS-102 N=534 Placebo N=266 Colon 63.3 60.5 Rectum 36.7 39.5 Wild-type 49.1 49.2 Mutant 50.9 50.8 Time since diagnosis of metastasis, % < 18 months 20.8 20.7 > 18 months 79.2 79.3 Number of prior regimens for metastatic, % 1-2 25.8 25.6 3 28.8 25.6 >4 45.3 48.9 Fluoropyrimidine 100 100 Irinotecan 100 100 Oxaliplatin 100 100 Bevacizumab 100 99.6 Anti-EGFR (if wild KRAS*) 99.6 99.3 Regorafenib 17.0 19.9 Primary site, % KRAS mutational status, % All prior systemic cancer therapeutic agents, % *Based on historical patient record Patient Disease Characteristics (cont’d) (Intent-to-treat population) TAS-102 N=534 Placebo N=266 100 100 Refractory to Fluoropyrimidine at any time it was given 97.6 99.6 Refractory to Fluoropyrimidine last time it was given 92.7 89.8 Patients receiving 5-FU as last Regimen Prior to Randomization, % 61.4 58.6 Patient receiving prior 5-FU, % Refractory to Fluoropyrimidine 91.8 89.7 Overall Survival Events # (%) 100 TAS-102 N=534 Placebo N=266 364 (68) 210 (79) HR (95% CI) 90 0.68 (0.58-0.81) Stratified Log-rank test p<0.0001 Survival Distribution function 80 Median OS, months 7.1 5.3 Median follow-up: 8.4 months 70 Alive at, % 60 50 6 months 58 44 12 months 27 18 40 30 20 10 0 N at Risk: TAS-102 Placebo 0 3 6 534 266 459 198 294 107 9 12 Months from Randomization 137 47 64 24 15 18 23 9 7 3 Progression-free Survival 100 Progression-free Distribution function 90 Events # (%) 80 TAS-102 N=534 Placebo N=266 472 (88) 251 (94) HR (95% CI) 0.48 (0.41-0.57) Stratified Log-rank test p<0.0001 70 Median PFS, months 60 2.0 1.7 Tumor assessments performed every 8 weeks 50 40 30 20 10 0 0 N at Risk: TAS-102 Placebo 2 4 6 8 10 12 14 16 5 1 4 1 2 0 Months from Randomization 534 266 238 51 121 10 66 2 30 2 18 2 Overall Response (tumor response evaluable population, investigator assessment) Best response, % Complete response or Partial response* Stable disease Disease control rate** Progressive disease Per RECIST version 1.1 *Not significant **CR, PR or SD, p<0.0001 TAS-102 N=502 Placebo N=258 1.6 0.4 42.4 15.9 44.0 16.3 51.8 75.6 Key Subgroup Analysis of OS Subgroup Favors Placebo Favors TAS-102 Events/N HR [95% CI] Median (mos) TAS-102 : PBO 574 / 800 0.68 [0.58, 0.81] 7.1 : 5.3 Wild Type Mutant Type 280 / 393 294 / 407 0.58 [0.45, 0.74] 0.80 [0.63, 1.02] 8.0 : 5.7 6.5 : 4.9 Geographic Region Japan West (AU/EU/US) 227 / 266 347 / 534 0.75 [0.57, 1.00] 0.64 [0.52, 0.80] 7.8 : 6.7 6.5 : 4.8 317 / 441 0.75 [0.59, 0.96] 6.8 : 4.9 All Subjects KRAS Status Refractory to 5-FU when given as last therapy prior to randomization* 0 0.5 1 1.5 2 Hazard Ratio: TAS-102 versus Placebo (95% CI) *Not prespecified subgroup Non-Hematologic Adverse Events Occurring in >10% of Patients (as-treated population) Non-Hema Adverse events, % TAS-102 (N=533) Placebo (N=265) All Gr. Gr. 3 Gr. 4 All Gr. Gr. 3 Gr. 4 Nausea 48.4 1.9 0 23.8 1.1 0 Decreased appetite 39.0 3.6 0 29.4 4.9 0 Fatigue 35.3 3.9 0 23.4 5.7 0 Diarrhea 31.9 2.8 0.2 12.5 0.4 0 Vomiting 27.8 2.1 0 14.3 0.4 0 Pyrexia 18.4 0.9 0.2 14.0 0.4 0 Asthenia 18.2 3.4 0 11.3 3.0 0 Constipation 15.2 0.2 0 15.1 1.1 0 Abdominal pain 14.8 2.1 0 13.6 3.4 0 Cough 10.7 0.4 0 11.3 0.8 0 Dyspnoea 10.5 2.1 0.4 12.8 2.3 0 Oedema peripheral 9.9 0.2 0 10.2 0.8 0 Weight decreased 7.7 0 0 10.2 0 0 One treatment-related death was observed in TAS-102 Hematologic Laboratory Abnormalities Occurring in >10% of Patients (as-treated population) Lab abnormalities, % TAS-102 (N=533) Placebo (N=265) All Gr. Gr. 3 Gr. 4 All Gr. Gr. 3 Gr. 4 Leukopenia 77.1 18.6 2.8 4.6 0 0 Anemia 76.5 18.2 0* 33.1 3.0 0 Neutropenia 66.9 26.5 11.4 0.8 0 0 Lymphocytopenia 64.6 18.2 3.3 39.7 9.2 0.8 Thrombocytopenia 42.2 4.5 0.6 8.0 0 0.4 Hematology *One case of grade 4 was reported in AE Occurring in < 10% of Patients but Clinically Important Adverse Events (as-treated population) Adverse events, % TAS-102 (N=533) Placebo (N=265) All Gr. Gr. 3 Gr. 4 All Gr. Gr. 3 Gr. 4 Febrile neutropenia 3.8 2.8 0.9 0 0 0 Stomatitis 7.9 0.4 0 6.0 0 0 Hand-foot syndrome 2.3 0 0 2.3 0 0 Cardiac ischaemia events, % 0.4 0.2 0 0.4 0 0.4 Acute myocardial infarction 0.2 0.2 0 0 0 0 Angina pectoris 0.2 0 0 0 0 0 Myocardial ischaemia 0 0 0 0.4 0 0.4 Conclusions • TAS-102 demonstrated a clinically relevant improvement in OS and PFS compared with placebo in mCRC pts refractory / intolerant to standard therapies – TAS-102 prolonged overall survival across all major prespecified subgroups including KRAS and region, and across the subgroup with patients refractory to 5-FU • TAS-102 was well tolerated – The most frequently observed toxicities were gastrointestinal and hematologic, the rate of febrile neutropenia was 3.8% • The RECOURSE results support TAS-102 as a new treatment option for patients with refractory mCRC Thanks to the Patients, Their Families and Study Team/Participants Austria: Australia: Belgium: Czech Republic: France: Germany: Ireland: Italy: Japan: Spain: Kathrin Strasser-Weippl, Andreas Petzer, Werner Scheithauer, Josef Thaler Ben Tran, Timothy Price, Nick Pavlakis, Niall Tebbutt, Guy van Hazel Jean-Luc Canon, Yves Humblet, Stephanie Laurent, Jean Luc Van Laethem, Eric Van Cutsem, Marc Peeters Eugen Kubala, Jan Vydra Antoine Adenis, Thierry Andre, Denis Smith, Fabienne Portales, Eveline Boucher, Christophe Borg Andreas Block, Dirk Buschmann, Volker Heinemann, Elke Jaeger, Goetz von Wichert, Markus Moehler, Ingo Schwaner, Hans-Joachim Schmoll, Heinz-Dieter Hofheinz, Meinolf Karthaus, Claus-Henning Koehne, Gunnar Folprecht, Thomas Zander Ray McDermott, David Fennelly, Brian Bird Alessandro Bertolini, Corrado Boni, Fortunato Ciardiello, Maria di Bartolomeo, Alfredo Falcone, Emiliano Tamburini, Alberto Sobrero, Marco Tampellini, Alberto Zaniboni, Giacomo Carteni', Salvatore Siena Yoshito Komatsu, Yasushi Tsuji, Hirofumi Fujii, Toshikazu Moriwaki, Kensei Yamaguchi, Takayuki Yoshino, Tadamichi Denda, Nobuyuki Mizunuma, Yasuo Hamamoto, Yasuhiro Shimada, Norisuke Nakayama, Kentaro Yamazaki, Kei Muro, Masahiro Goto, Naotoshi Sugimoto, Akihito Tsuji, Tetsuji Takayama, Tomohiro Nishina, Taito Esaki, Hideo baba Jesus Garcia Foncillas, Laura Lema, Carles Pericay, Maria Jose Safont, Josep Tabernero, Rocio GarciaCarbonero, Andres Cervantes Ruiperez, Alberto Carmona Bayonas, Jose Manzano, Manuel Benavides, Federico Longo, Antonieta Salud Sweden: Jan-Erik Frodin, Bengt Glimelius UK: USA: Stephen Falk, Leslie Samuel, David Cunningham, John Bridgewater, Daniel Swinson, David Cunningham Jerilyn Hart, Philip Stella, Ari Baron, Ronald Yanagihara, Christopher Vaughn, Derrick Spell, Heinz-Josef Lenz, James Knost, Robert Mayer, Nashat Gabrail, Howard Hochster, Ali Khojasteh, Timothy Kasunic, David Ryan, Omar Kayaleh, Pei Hua Lu, Brian DiCarlo, Steven Hager, Devinder Singh, Jyotsna Fuloria, J. Marc Pipas, Heinz Lenz, Patrick Loehrer, Timothy O'Brien RECOURSE was supported by Taiho Oncology Inc./Taiho Pharmaceutical Co. Ltd.