Appendix 1. The following investigators, coordinators, and centers
advertisement

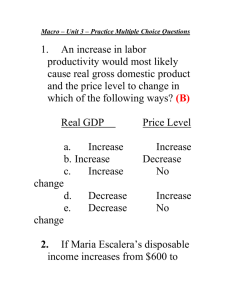
Appendix 1. The following investigators, coordinators, and centers participated in the study: P. Desai, M. Betzen, D. DeLuna, Amarillo Heart Clinical Research Institute, Amarillo; J. Whitehill, J. Hatch, L. Janak, R. Cherry, Austin Heart P.A., Austin; E. Gonzalez, I. Cruz, Baptist Cardiac & Vascular Institute, Miami; E. Johnson, C. Allbritton, V. Derrick, Baptist Memorial Hospital, Memphis; R. Fishman, V. Assalone, L. Mahon, Bridgeport Hospital, Bridgeport; D. Lustgarten, M. Rowen, M. Bessette, B. Alemy, Fletcher Allen Health Care, Burlington; D. Dan, K. Picardi, Fuqua Heart Center, Atlanta; C. Schuger, J. Dzidowski, M. McCarthy, P. Fields, S. Alexander, Henry Ford Hospital, Detroit; G. Nair, R. Kovacs, D. Beasley, T. Strickland, J. Marks, IU Health Methodist Research Institute, Indianapolis; S. Beau, J. Tableriou, B. Griffin, Little Rock Cardiology Clinic, Little Rock; J. Shani, M. Stokes-McCarthy, G. Tan-Augenstein, G. Pace, H. Brosnan, Maimonides Medical Center, New York; J. Hayes, K. Mancl, K. Maassen, Marshfield Clinic, Marshfield; D. Fintel, L. Karpf, T. Abraham, K. Campione, E. Martin, Northwestern Memorial Hospital, Chicago; D. Bello, I. Viera Fleetwood, M. Tinetti, R. Rock, Orlando Regional Medical Center, Orlando; J. Simonson, S. Barnes, J. Letexier, M. Strothman, J. Mattson, Park Nicollet Institute, Minneapolis; C. Albert Shoultz III, S. Ali, Providence Healthcare Network; D. Abbott, M. Medeiros, J. McKeon, Rhode Island Hospital/Brown Medical School, Providence; A. Nichols, T. Edwards, C. Watts, C. Alley, Riverside Methodist Hospital, Columbus; M. Romanelli, D. Steffen, R. Henschel, S. Teller, L. Froehlich, R. Bess, St. John Hospital & Medical Center, Detroit; W. Warnica, B. Smith, D. Eichman, D. Scarcelli, University of Calgary, Calgary; N. Badhwar, P. Malone, D. Green, S. Iyer, University of California at San Francisco, San Francisco; R. Germany, C. Murray, G. Straughn, K. Drennan, University of Oklahoma, Oklahoma City; O. Marroquin, L. Dennis, C. Farrow, L. Baxendell, S. Grate, M. Enlow, University of Pittsburgh Medical Center, Pittsburgh; W. Zareba, I. Chaudhary, P. Laduke, V. Conary-Rocco, L. Caufield, C. Patterson, University of Rochester - Strong Memorial Hospital, Rochester; A. Warner, J. Johnson, West Los Angeles VA Medical Center, Los Angeles; J. Germano, W. Drewes, B. George, B. Yoo, D. Patel, Winthrop University Hospital, Mineola. Steering Committee - R. Bonow*, Northwestern University, Chicago; M. Cuffe*, Hospital Corporation of America; A. Dyer, Northwestern University, Chicago; P. Greenland, Northwestern University, Chicago J. Goldberger*, Northwestern University, Chicago; R. O’Rourke, University of Texas Health Science Center at San Antonio, San Antonio; Y. Rosenberg*, National Heart, Lung, and Blood Institute, Bethesda; P. Shah*, Cedar-Sinai Medical Center, Los Angeles; S. Smith*, University of North Carolina, Chapel Hill. * current members (all original members are listed) Observational Study Monitoring Board- R. Byington, Wake Forest University Health Science, Winston-Salem, N.C.; Z. Feng, Fred Hutchinson Cancer Research Center, Seattle; S. Goldstein, Henry Ford Hospital, Detroit; J. Kirkpatrick, Hospital of the University of Pennsylvania; C. Love, New York University Medical Center, New York; S. Singh, Veteran Affairs Medical Center, Washington, D.C. National Heart, Lung, and Blood Institute - Y. Rosenberg, S. Goldberg, M. Kwak, A. Rao, P. Srinivas Northwestern University Clinical and Data Coordinating Center- J. Goldberger, C. Ball, J. Cahill, A. Schaechter, D. Alexander, K. Ma, T. Plant, A. Rosenfeld, J. Scofic, J. Simon, H. Subačius APPENDIX 2 This Appendix provides detail on the implementation of propensity score adjustment. First, we show the SAS code used to calculate the propensity score. Second, we present the parameters obtained in the propensity score model. Third, we show the histogram of the propensity scores for each treatment arm. We used the propensity score as a control variable (including quadratic and cubic polynomials) in a proportional hazards frailty regression model identical to all other survival analyses in this manuscript. There are two advantages of this approach over matching. First, no patients are excluded from the sample on account of non-overlapping propensity scores among the four groups, providing a larger sample size. Second, it is challenging in practice to do propensity score matching when there are more than 2 treatment arms, in particular 4 groups for this analysis. 1. SAS Code for calculation of the propensity score %let Class = Male White Hispanic SmokeCurrent Diabetes Hypertension HyperChol STEMI Lytic_IH PPCI_IH PrevMI CABG ReVasc COPD ESRD CHFHx CHFDx CVATIA Anterior ICDall ASA ACEIARB Statin Clopidogrel MetoprololDC CarvedilolDC; %let Cubic = Age|Age|Age lnTroponin|lnTroponin|lnTroponin LVEF|LVEF|LVEF lnLOS|lnLOS|lnLOS BMI|BMI|BMI RestSBP|RestSBP|RestSBP PRestHR|PRestHR|PRestHR; /* Calculate the Propensity Score--Risk-Adjusted Dose */ proc GLIMMIX data=OutMi; by _Imputation_; class SiteNumber; model BBDosePctN = &Class &Cubic random SiteNumber; run; Note that PS calculation and PH regression were both done on 5 sets of multiply imputed data; hence, the “by_Imputation_;” line in the SAS code. 2. SAS output of the propensity score model Effect Estimate Standard Error DF t Value p-value Intercept 73.3402 27.3697 25 2.68 0.0128 Male 1.5484 5972 2.08 0.0373 White -2.4658 0.8674 5972 -2.84 0.0045 Hispanic -2.651 1.3689 5972 -1.94 0.0528 Current smoker -1.4012 0.7751 5972 -1.81 0.0707 Diabetes 0.5209 0.7763 5972 0.67 0.5022 Hypertension 5.8958 0.7846 5972 7.51 <0.0001 Hyperlipidemia 1.9786 0.7125 5972 2.78 0.0055 STEMI -0.9833 0.9018 5972 -1.09 0.2756 Anterior location 1.0747 5972 0.99 0.3206 Thrombolytic therapy -2.0679 1.3413 5972 -1.54 0.1232 Primary PCI -4.2603 0.91 5972 -4.68 <0.0001 Previous MI 2.0496 0.8681 5972 2.36 0.0183 History of CABG 7.1149 1.0619 5972 6.7 <0.0001 In-hospital revascularization -3.0209 0.9034 5972 -3.34 0.0008 COPD -2.1153 1.1341 5972 -1.87 0.0622 ESRD 2.0759 1.8872 5972 1.1 0.2714 CHF History 4.1411 1.2163 5972 3.4 0.0007 Heart failure on admission -1.0349 1.2118 5972 -0.85 0.3931 CVA/TIA 2.145 1.108 5972 1.94 0.0529 ICD 4.3632 1.9198 5972 2.27 0.0231 ASA 0.02195 1.3538 5972 0.02 0.9871 ACE-I/ARB 1.5641 0.738 5972 2.12 0.0341 Statin 0.9858 1.1329 5972 0.87 0.3842 Clopidogrel 1.7464 0.8085 5972 2.16 0.0308 Metoprolol -11.7374 1.3423 5972 -8.74 <0.0001 Carvedilol -13.5138 1.5081 5972 -8.96 <0.0001 Age linear -1.0941 0.9973 5972 -1.1 0.2727 Age quadratic 0.0186 5972 1.14 0.253 0.7435 1.0818 0.01627 Age cubic -0.00011 0.000086 5972 -1.27 0.2032 ln(Troponin) 0.09247 0.357 5972 0.26 0.7956 ln(Troponin) quadratic 0.1224 5972 0.74 0.4622 ln(Troponin) cubic -0.02285 0.02931 5972 -0.78 0.4357 LVEF linear 0.06153 0.4686 5972 0.13 0.8955 LVEF quadratic 0.003227 0.01111 5972 0.29 0.7715 LVEF cubic -0.00004 0.000083 5972 -0.46 0.6448 ln(LOS) linear 3.441 6.3559 5972 0.54 0.5883 ln(LOS) quadratic 2.438 3.0462 5972 0.8 0.4235 ln(LOS) cubic -0.7217 0.4552 5972 -1.59 0.1129 BMI linear -1.5172 0.8868 5972 -1.71 0.0872 BMI quadratic 0.05293 0.02482 5972 2.13 0.033 BMI cubic -0.00048 0.00022 5972 -2.18 0.0296 Admission SBP linear -0.5449 0.2697 5972 -2.02 0.0434 Admission SBP quadratic 0.00387 0.00183 5972 2.11 0.0345 Admission SBP cubic -7.17E-06 4.04E-06 5972 -1.78 0.0757 Admission HR linear 0.07088 0.2491 5972 0.28 0.776 Admission HR quadratic 0.00052 0.002421 5972 0.21 0.8298 Admission HR cubic -1.91E-06 7.39E-06 5972 -0.26 0.796 0.1664 Abbreviations as in Table 1: ASA-aspirin, ACE-I-angiotensin converting enzyme inhibitor, ARB-angiotensin receptor blocker, BMI-body mass index, CABG-coronary artery bypass graft surgery, CHF- congestive heart failure, COPD-chronic obstructive pulmonary disease, CVA-cerebrovascular accident, ESRD-end stage renal disease, HR-heart rate, ICDimplantable cardioverter defibrillator, LOS-length of stay, LVEF-left ventricular ejection fraction, MI-myocardial infarction, PCI-percutaneous coronary intervention, SBP-systolic blood pressure, STEMI-ST elevation MI, TIA-transient ischemic attack Histogram of the propensity scores by discharge beta-blocker category. It can be seen that the propensity scores of all four dose categories overlap for a substantial portion of the distribution, noting that the dose category >50% has more propensity scores with higher values. The propensity score adjustment can reduce selection bias caused by such imbalance in covariate values.