ImPACT Program Lovell, Collins & French
advertisement
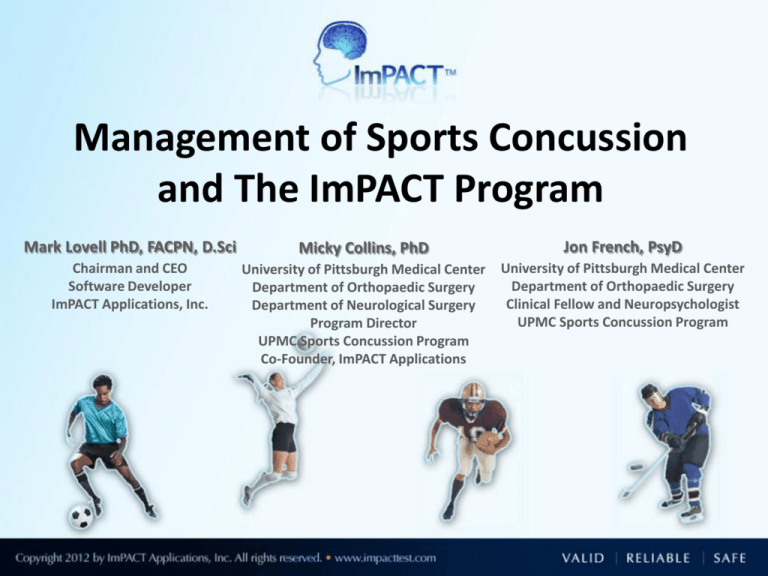
Management of Sports Concussion and The ImPACT Program Mark Lovell PhD, FACPN, D.Sci Micky Collins, PhD Jon French, PsyD Chairman and CEO Software Developer ImPACT Applications, Inc. University of Pittsburgh Medical Center Department of Orthopaedic Surgery Department of Neurological Surgery Program Director UPMC Sports Concussion Program Co-Founder, ImPACT Applications University of Pittsburgh Medical Center Department of Orthopaedic Surgery Clinical Fellow and Neuropsychologist UPMC Sports Concussion Program Workshop Goals To Provide Background Information Regarding Concussion Management To Present Data Pertaining to Outcomes and Risk Factors Associated with Sports Concussion To Discuss Academic Needs for Recovering Student Athlete with Concussion To Review the Utility of Computerized Neurocognitivie Testing and ImPACT as a Tool for Effective Concussion Management To Review Clinical Case Material Concussion 101: Biomechanics, Pathophysiology, Definition Micky Collins, PhD Associate Professor and Director UPMC Sports Medicine Concussion Program Copyright © 2011 Neurometabolic Cascade Following Cerebral Concussion/MTBI 500 (Giza & Hovda, 2001) Calcium % of normal 400 K+ 300 Glucose 200 Glutamate 100 50 2 6 0 Cerebral Blood Flow 12 minutes 20 30 6 hours 24 3 6 days UCLA Brain Injury Research Center 10 Concussion Management: Areas of Focus Rule out more serious intracranial pathology • CT, MRI, neurologic examination primary diagnostic tests Prevent against Second Impact Syndrome Prevent against cumulative effects of injury • Less biomechanical force causing extension of injury Prevent presence of Post-Concussion Syndrome Most Commonly Reported Symptoms – 1-7 days following concussion SYMPTOM PERCENT #1 Headache 75% #2 Difficulty Concentrating 57 % #3 Fatigue 52 % #4 Drowsiness 51 % #5 Dizziness 49 % #6 Foggy 47 % #7 Feeling Slowed Down 46 % #8 Light Sensitivity 45 % #9 Balance Problems 39 % # 10 Difficulty with Memory 38 % Kontos, Elbin, French Collins, Data Under Review; N = 1,438 Post-Concussion Symptom Groups • • • • • • • • • Headaches Visual Problems Dizziness Noise/Light Sensitivity Nausea N=327, High School and University Athletes Within 7 Days of Concussion More emotional Sadness Nervousness Irritability • • • • • Attention Problems Memory dysfunction “Fogginess” Fatigue Cognitive slowing • Difficulty falling asleep • Sleeping less than usual (Pardini, Lovell, Collins, et al. 2004) The Evolving Definition of Concussion CDC Physicians Toolkit 2007 A concussion (or mild traumatic brain injury) is a complex pathophysiological process affecting the brain, induced by traumatic biomechanical forces secondary to direct or indirect forces to the head. Disturbance of brain function is related to neurometabolic dysfunction, rather than structural brain injury, and is typically associated with normal structural imaging findings (CT Scan, MRI). Concussion may or may not involve a loss of consciousness. Concussion results in a constellation of physical, cognitive, emotional, and sleep-related symptoms. Recovery is a sequential process and symptoms may last from several minutes to days, weeks, months, or even longer in some cases.” Management of MTBI: Topics of Concern Grading systems ineffective/not data based. CT and MRI insensitive to subtleties of injury. Self-report predicates management directives. Variability in clinician recommendations. Lack of education and awareness of injury. Inadequate/Improper recommendations from ED/Trauma Departments. 23 Return to Play Following mTBI: In some cases (not all), athletes will minimize difficulties Athletes are naïve to the subtleties of the injury Young athletes lack insight into self-assessment of MTBI symptoms Studies suggest that up to 50% of athletes experience concussion symptoms per year but only 10 % report having an injury Need for comprehensive understanding of athletes recovery status Computer-Based Neurocognitive Testing Cogsport (Axon) Headminders (CRI) ANAM CNS Vital Signs ImPACT ImPACT Mark Lovell, PhD, FACPN, Dsci, Software Developer, ImPACT Micky Collins, PhD - UPMC Dept. of Orthopaedic Surgery Joseph Maroon, MD - UPMC Dept. of Neurological Surgery ImPACT: Post-Concussion Evaluation Demographic / Concussion History Questionnaire Concussion Symptom Scale 21 Item Likert Scale (e.g. headache, dizziness, nausea, etc) 8 Neurocognitive Measures Verbal Memory, Visual Memory, Reaction Time, Processing Speed Summary Scores Detailed Clinical Report Outlines Demographic, Symptom, Neurocognitive Data Automatically Computer Scored Internal baseline validity checks built into program Desktop and On-Line Versions Available Extensive normative data available from ages 11-60 Over 100 peer-reviewed research articles/books/chapters, published since 2000 Extensive data published on reliability, validity, sensitivity/specificity of test Neurocognitive Testing: What it is and Isn’t IS a tool to help determine recovery from injury. IS a tool to help manage concussion (e.g. return to academics, return to exertion return to play). IS a tool to help communicate post-concussion status to coaches, parents, clinicians. IS NOT a substitute for medical evaluation / treatment Baseline Testing Supervised at School Or clinic Concussion Remove From Play First Follow-Up Evaluation Follow-up Testing as needed Return to Play Measuring Neurocognitive Recovery from Sports mTBI Authors Sample Size Population Tests Utilized Total Days Cognitive Resolution Total Days Symptom Resolution Lovell et al. 2005 95 Pro (NFL) Paper and Pencil NP 1 day 1 day McCrea et al. 2003 94 College SAC <1 Day 7 days McCrea et al. 2003 94 College Paper and Pencil NP 5-7 days 7 days Echemendia 2001 29 College Paper and Pencil NP 3 days 3 days Guskiewicz et al. 2003 94 College Balance BESS 3-5 Days 7 Days Bleiberg et al. 2005 64 College Computer NP (ANAM) 3-7 days Did Not Evaluate Iverson et al. 2006 30 High School Computer NP (ImPACT) 10 days 7 Days McClincy et al. 2006 104 High School Computer NP (ImPACT) 14 days 7-10 Days Lovell, Collins et al 2008 208 High School Computer NP (ImPACT) 26 days 17 Days Covassin et al 2011 72 High School Computer NP (ImPACT) 21 days 7 Days Maugans et al 2011 12 Ages 11-15 Computer NP (ImPACT) 30 days 14 Days Three-year prospective study in Western PA. 17 high school football teams (2,141 total sample) 134 athletes with diagnosed concussion (6.2%) All athletes referred for evaluation at UPMC Recovery determined by “Back to Baseline” on computer neurocognitive test scores & symptom inventory Determined by Reliable Change Index Scores-RCI’s) 100 90 80 70 60 50 40 30 20 10 0 WEEK 1 WEEK 2 WEEK 3 WEEK 4 WEEK 5 80% RECOVERED 60% RECOVERED N=134 High School Male Football Athletes 40% RECOVERED 1 3 5 All Athletes 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 38 40+ No Previous Concussions 1 or More Previous Concussions Over 200 High School Athletes Studied using fMRI Tested w/in 7 days of concussion and at point of clinical recovery Hyperactivation predicts CLINICAL recovery time Resolution of hyperactivation correlates with recovery on ImPACT Lovell et al., Neurosurgery, 2007 (Lovell, Pardini, Collins et al; Neurosurgery 2007) Mean Age: 16.2 yrs Gender: 78% male Days to Recover Range 4 – 211 days* Mean 26.2 days * End of study period N = 208 Cumulative Percent Recovery 15 days 25% 26 days 50% 45 days 75% 92 Days 90% Prognosticating Concussion Outcomes: An Evidence-Based Analysis Micky Collins, Ph.D. University of Pittsburgh Medical Center Associate Professor Department of Orthopaedic Surgery Department of Neurological Surgery Director UPMC Sports Concussion Program Helps to set up clear communication to player, coaches, and medical personnel regarding recovery expectations May help to alleviate some pressure on RTP issue May help to immediately provide individualized clinical management recommendations (e.g. need for academic accommodations/physical rest, etc.) Begins to create a risk profile for sports concussion and may set stage to effectively research treatment and rehabilitation strategies. Because it is the next stage in our scientific understanding of this injury…. Which On-Field Symptoms Predict Protracted Recovery (i.e. Post-Concussion Syndrome)? Which On-Field Symptoms Increase Risk of Post Concussion Syndrome in High School Football Players? 176 Male HS Football Players (Mean Age = 16.2 years) Athletes had baseline ImPACT testing and were revaluated within 3 days of injury. All followed until clinical recovery (Mean = 4.1 evaluations) Within RCI of baseline on ImPACT for neurocognitive/symptom scores 32% of sample required < 7 days until recovery (N =56) “Rapid Recovery” (Mean = 4.9 days) 39% of sample required 7-14 days until recovery (N = 68) 17% of sample required > 21 days until recovery (N = 31) “Protracted Recovery” (Mean = 33.2 days) 12% lost to follow up (e.g. did not RTP or no follow-up in clinic) (N = 21) MANOVA used to determine differences between rapid/> 3 week recovery ATC’s documented on-field markers (e.g. LOC, Amnesia) and on-field Symptoms (e.g. headache, dizziness, etc) Lau B, Kontos A, Lovell MR, Collins MW, AJSM 2011 Which On-Field Markers/Symptoms Predict 3 or More Week Recovery from MTBI In High School Football Players On-Field Marker N Chi2 P Odds Ratio 95% Confidence Interval Posttraumatic Amnesia 92 1.29 0.257 1.721 0.67-4.42 Retrograde Amnesia 97 .120 0.729 1.179 0.46-3.00 Confusion 98 .114 0.736 1.164 0.48-2.82 LOC 95 2.73 0.100 0.284 0.06-1.37 On-Field Symptom N Chi2 P Odds Ratio 95% Confidence Interval Dizziness** 98 6.97 0.008 6.422 1.39-29.7 Headache 98 0.64 0.43 2.422 0.26-22.4 Sensitivity LT/Noise 98 1.19 0.28 1.580 0.70-3.63 Visual Problems 97 0.62 0.43 1.400 0.61-3.22 Fatigue 97 0.04 0.85 1.080 0.48-2.47 Balance Problems 98 0.28 0.59 0.800 0.35-1.83 Personality Change 8 0.86 0.35 0.630 .023-1.69 Vomiting 97 0.68 0.41 0.600 0.18-2.04 The total sample was 107. Due to the normal difficulties with collecting on-field markers, there were varying degrees of missing data. The number of subjects who had each coded ranged from 92-98. The N column represents the number of subjects for whom data were available for each category. Markers of injury are not mutually exclusive. **p<.01 Lau, Kontos, Collins, Lovell , AJSM 2011 On-Field Symptom Summary Brief LOC (<30 sec) not predictive of subacute or protracted outcomes following sports-concussion Amnesia important for sub-acute presentation, but may not be as predictive of protracted recovery On-Field dizziness best predictor of protracted recovery and “post concussion syndrome” Etiology of dizziness? • • • • • Migraine variant? Central Vestibular Dysfunction? Peripheral Vestibular Dysfunction? Cervico-genic? Psychiatric? Which Subacute Symptoms Predict Protracted Recovery? 108 concussed high school football players • Athletes had baseline ImPACT testing and were revaluated within 3 days of injury (Mean = 2.2 days) • All followed until clinical recovery - Within Reliable Change Score of baseline for neurocognitive/symptom scores • 43.5% of sample recovered < 10 days = “Quick” - Mean = 5.9 Days • 56.5% of sample required >10 days until recovery = “Protracted” - Mean = 29.2 Days • MANOVA conducted on which individual symptoms and neurocognitive domains predicted “quick” versus “protracted” recovery Lau B, Lovell MR, Collins MW; Pardini J; CJSM 2009 (3):216-21 Current Symptoms Headache Nausea Vomiting Balance Problems Dizziness Fatigue Trouble falling asleep Sleeping more than usual Sleeping less than usual Drowsiness Sensitivity to light Sensitivity to noise Irritability Sadness Nervousness Feeling more emotional Numbness or tingling Feeling slowed down Feeling mentally foggy Difficulty concentrating Difficulty remembering Visual problems (blurry or double vision) FOGGY NAUSEA LIGHT SENS DIFF CONC HEADACHE NOISE SENS VOMIT SLOWNESS NUMBNESS DIZZY BALANCE 2 1.5 1 0.5 0 Expressed as Effect Sizes (Cohen’s D). Only includes symptoms with large (greater than .80) effect sizes. Sample is composed of 108 male HS football athletes. “It is like going from a high definition TV world to standard TV world” “Feeling one step removed from my surroundings” “It is like my vision is impaired, but it isn’t” “Feeling like I am underwater” Factor Analysis, Post-Concussion Symptom Scale (Pardini, Lovell, Collins et al. 2004) • • • • • • • • • Headaches Visual Problems Dizziness Noise/Light Sensitivity Nausea N=327, High School and University Athletes Within 7 Days of Concussion More emotional Sadness Nervousness Irritability • • • • • Attention Problems Memory dysfunction “Fogginess” Fatigue Cognitive slowing • Difficulty falling asleep • Sleeping less than usual Variables Fogginess Difficulty Concentrating Vomit Dizziness Nausea Headache Slowness Balance Light Sensitivity Noise Sensitivity Numbness Trouble Sleeping Classification Cognitive Cognitive Migraine Migraine Migraine Migraine Cognitive Migraine Migraine Migraine Migraine 4.3* 2.46 2.391* 2.09 1.96 1.71 1.53 1.53 1.52 1.52 1.46 Sleep 1.231* 0.97 Visual Problems Difficulty Remembering Sleeping Less Drowsiness Fatigue Emotional Migraine Cognitive Sleep Cognitive Cognitive Neuropsychiatric Irritability Sadness Nervousness Neuropsychiatric Neuropsychiatric Neuropsychiatric Sleeping More Z-Score (Simple vs. Complex) Cognitive 0.93 .52 0.5 0.48 0.37* 0.3 0.09 -0.03 -0.05 *Symptoms with the largest contributions to differences between “quick” and “protracted” recovery in each symptom factor. The Role of Sub-Acute Migraine-Symptoms in Determining Outcomes Following Concussion Kontos AP, Elbin RJ, Simensky S, French J, Collins MW; data in preparation for publication Post-traumatic Migraine (PTM) Defined • Post-traumatic Migraine – Headache, nausea, AND sensitivity to light OR noise (International Headache Society Guidelines) • Determined by utilizing PCSS at 1-7 days post-concussion Kontos AP, Elbin RJ, Simensky S, French J, Collins MW; In preparation.. Study Overview • 174 high school athletes with a concussion – No prior hx of LD, moderate TBI, psychiatric disorder • Athletes followed until recovery – Neurocognitive scores returned to baseline (w/in RCI) – Symptom free and rest and exertion • 97 athletes met Rapid or Protracted Criteria for Recovery: – Rapid (≤7 days)= 61 – Protracted (≥21 days)= 36 • Recovery studied for three groups – – – • No headache group Headache only group Post-traumatic migraine group (headache with nausea and/or light and noise sensitivity) Data Analysis – – Chi-square analysis with Odds Ratios for Recovery Time Groups Repeated measures ANOVAs for ImPACT scores across 3 time periods Kontos AP, Elbin RJ, Simensky S, French J, Collins MW; In preparation.. How does PTM compare to No Headache and Headache groups in predicting Protracted (>21 days) Recovery from Sports Concussion? (N= 97) Variable Wald p Odds Ratio Headache v. No Headache 2.20 .14 2.83 0.72-11.20 PTM v. Headache 3.93 .04 2.57 1.10-6.54 PTM v. No Headache 7.60 .006 7.29 1.80-29.91 95% CI Kontos AP, Elbin RJ, Simensky S, French J, Collins MW; In preparation.. Comparison of Recovery for PTM, Headache, No Headache/PTM groups (χ2= 9.05, p= .009, n= 97) ImPACT Visual Memory Raw Score PTM = Post Traumatic Migraine N = 97 HS Athletes with concussion Comparison of ImPACT Visual Memory scores for PTM, Headache, and No PTM or Headache groups (λ= .88, F= 4.24, p= .002, η2 = .06)* *PTM significantly different than both groups at 1-7 and 8-14 days PTM defined as headache with nausea and sensitivity to light or noise (IHS Classification) ImPACT Reaction Time Raw Score PTM = Post-Traumatic Migraine Comparison of Reaction Time scores for PTM, Headache, and No PTM or Headache groups (λ= .87, F= 4.96, p= .001, η2= .07) *PTM significantly different than both groups at 1-7 and 8-14 days PTM defined as headache with nausea and sensitivity to light or noise (IHS Classification) Conclusion “It’s more than just a headache”: – Athletes with migraine-type symptoms (headache with nausea and/or light-noise sensitivity) exhibit more protracted recovery than with athletes with headache only – 81% of post-traumatic migraine group also reported dizziness (post-traumatic vestibular migraine??) – Important to assess for quality and type of headache in athletes with concussion Sensitivity and Specificity of ImPACT in Classifying Athletes with Concussion Schatz P, Pardini J, Lovell MR, Collins MW. Archives of Clinical Neuropsychology 2005:21;91-99. N = 138 controls/ concussed athletes Discriminate Function Analysis Statistical classification of Concussed (physician dx)/Control subjects No Clinician Input Testing completed within 3 days post injury Positive Predictive Value (90%) (Probability that that a concussion is present when test is positive) Negative Predictive Value (82%) (Probability that a concussion is not present when test is negative) Determination of Neurocognitive Cutoff Scores that Predict Protracted Recovery (at 2 days post injury) Lau B, Collins MW, Lovell MR Neurosurgery 2012;Feb 70(2):371-79. 108 concussed HS and Collegiate Athletes Athletes had baseline computerized NP testing and were revaluated within 3 days of injury (Mean = 2.2 days) All followed until clinical recovery Within Reliable Change Score of baseline for neurocognitive/symptom scores 43.5% of sample recovered < 14 days = “Quick” Mean = 5.9 Days 56.5% of sample required >14 days until recovery = “Protracted” Mean = 33.0 Days ImPACT composite cutoff scores statistically calculated at 75%, 80%, and 85% sensitivity to predict protracted recovery (i.e. 1 month or longer for clinical recovery) Lau B, Collins MW, Lovell MR. Neurosurgery In Press Cutoff Values of ImPACT Neurocognitive Scores at 2 Days Post Injury That Predict Protracted Recovery 75% 80% 85% Sensitivity Sensitivity Sensitivity Neurocognitive Domain Cutoff Cutoff Cutoff Verbal Memory 66.5 64.5 60.5 Visual Memory 48 46 44.5 Processing Speed 24.5 23.5 22.5 Reaction Time 0.72 0.78 0.86 Sensitivity is defined as the ability of the cutoff to accurately identify protracted recovery (>14 days; Mean = 1 month) in an athlete. Lau B, Collins MW, Lovell MR. Neurosurgery 2012. Predicting Quick versus Protracted Recovery from Sports mTBI - At three days post-injury, if athlete exhibit three or more RCI changes on ImPACT composite scores (relative to baseline), there is a 94% chance that recovery will require >10 days. - Exhibiting a high symptom score did not improve classification accuracy over neurocognitive test scores in isolation. - Athletes with prior history of concussion were not statistically more likely to have “protracted” recovery from concussion. Other Recent Peer Reviewed Research Examining Neurocognitive Testing Use of Computerized Neurocognitive Testing In High School Athletes (Meehan et al, 2011) 41.2% of US High Schools that employ at least 1 ATC utilized computerized neurocognitive testing during 2009-2010 academic year (25.7% in 20082009 year) 93% use ImPACT 100% of schools utilizing testing reported that scores were utilized in making RTP decisions 86% of these schools performed baseline testing Athletes who underwent computerized NP tesing were less likely to be returned to play within 10 days of injury (38.5% vs 55.7%, p < .01) and were more likely to be returned to play by a physician (60.9% vs 45.6%, p <.01) Established (?) Constitutional Risk Factors For More Complicated Recovery Age - Field, Lovell, Collins et al. J of Pediatrics, 2003 Pellman, Lovell et al. Neurosurgery, 2006 Migraine History & Symptoms - Mihalik, Collins,Lovell et al, J Neurosurgery, 2006 Learning Disability - Collins, Lovell et al, JAMA, 1999 Kontos, Elbin, Collins, Data submitted for publication Repetitive Concussion? - Collins, Lovell et al, Neurosurgery, 2004 Iverson et al, CJSM, 2004 Moser et al, JCEN, 2011 Gender? - Colvin, Lovell, Pardini, Mullin, Collins, AJSM, 2009 Covassin et al, CJSM, 2009 Outcomes are highly variable Vestibular-related symptoms following injury predict more protracted recoveries Migraine-type symptoms (and potentially preexisting history of migraine) may place individuals at increased risk of injury and longer recovery Neurocognitive testing is valuable in determining prognosis and recovery in sports-related mTBI Clinical management key to preventing poor outcomes The “mild” injuries may become severe and the “severe” injuries may become mild Sports Concussion Scientific Evolution and Building Consensus: Where are we Headed? CDC Physician Toolkit (Collins, Gioia, et al. 2007) Recommended Sports Concussion Management Post-Injury Management Removal from contest if concussion suspected-no RTP in same game No return to play while symptomatic or if symptomatic with exertion Carefully monitored and graded increase in exertion over time Need to be mindful of cognitive exertion on role of recovery Need for conservative management in children/adolescents Neurocognitive testing recommended for athletes sustaining concussion Criteria for Return to Play 1. 2. 3. Symptom-Free at Rest Symptom-Free with Cognitive/Physical Exertion Normal Neurocognitive Data/Objective Evaluation - “Conservative” approach to management of concussion - Out of play for game/practice with any LOC, amnesia, or confusion - Out of play for game/practice if new and persistent dizziness, headache (particularly if accompanied by photo/phonophobia, dizziness, nausea, or vomiting) or any other persistent symptoms of concussion - Follow up evaluation to be conducted by team physician as well as independent “neurological consultant ” - Clearance for RTP required by both - Baseline and post-injury neurocognitive testing mandated by league - No return to play until athlete exhibits normal neurological evaluation and is… 1) asymptomatic at rest 2) asymptomatic with progressive exertion, and 3) neurocognitive test scores back to baseline (within RCI indices on ImPACT) Copyright © 2011 - Institutions must have concussion plan on file - Any athlete exhibiting signs/symptoms of concussion shall be removed from practice/game and evaluated by healthcare practitioner with training in management of concussion-no RTP until formal clearance - Neuropsychological testing is an important component of an institutional concussion management plan. - “Best Practices” should include a baseline/post injury assessment using, at minimum, sideline tool (e.g. symptom checklist, SAC, SCAT, BESS), and, optimally, formal computerized or paper and pencil neurocognitive testing - Education necessary- Dept of Education will post concussion educational information; Student/parents must sign form prior to participation that they have reviewed concussion fact sheet. Coaches must complete concussion management training course on yearly basis. Informational school meetings are encouraged that educate on concussion management and importance of baseline assessments that can aid in evaluation and management of injury. - Any athlete exhibiting signs/symptoms of concussion shall be removed from practice/game and no RTP on day of injury. Medical clearance must occur from: Physician trained in concussion management OR licensed physician designee trained in concussion management, OR licensed neuropsychologist (fellowship trained) who has specific training in concussion management. Penalties occur with any infraction. Copyright © 2011