Behçet's disease: Diagnosis
advertisement

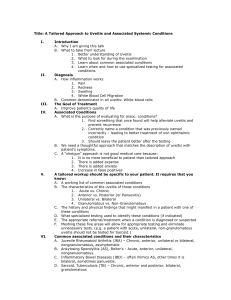
Faculty of Medicine, Cairo University Clinical significance of interleukin-23 and gene polymorphism in Behçets disease Tamer A Gheita, MD Professor of Rheumatology and Clinical Immunology, Faculty of Medicine, Cairo University Egypt The following will be considered: Behçet’s disease Interleukin-23 The Clinical Study Behçet’s disease Behçet’s disease: Historical Background Behçet’s disease (BD) is a multisystemic vasculitis and chronic relapsing inflammatory disease of unknown cause, characterized by recurrent oral ulcers, genital ulcers, uveitis and skin lesions [1] Behçet’s disease Historical Background Behçet’s disease: Historical Background Behçet's disease (BD) refers to Halusi Behçet (1889-1948), a Turkish dermatologist who recognized the triple-complex of recurrent oral ulcers, genital ulcers and uveitis. In 1936, he published it in Archives of Dermatology and Venereal Disease [2] Halusi Behçet (1889-1948) An initial description was also made 1930 by Benedict Adamantiades (1875-1962) the Greek ophthalmologist from Prussia, Asia minor (nowadays Bursa, Turkey) who presented ‘A case of relapsing iritis with hypopyon’ [3]. Behçet’s disease Epidemiology Behçet’s disease: Epidemiology Prevalence: The highest prevalence is reported along the ancient Silk route extending from Eastern Asia to the Mediterranean basin [4,5] Ancient Silk route Behçet’s disease: Epidemiology Global distribution of BD: Dot size reflects prevalence [6,7] Turkey has the highest prevalence (80-370 cases/100.000). It is lower in UK (0.64 cases) and about 0.2 cases/100.000 in USA. Behçet’s disease: Epidemiology In Germany, the prevalence among citizens of Turkish origin is 21/100.000, which is lower than that in Turkey but far higher than that among German natives [1,8]. Onset: is typically in the 3rd- 4th decade of life [6]. Gender preference: More common in males in the Middle East while in Japan/Korea (Far East), females are more affected [4,8,9]. A more equal M:F ratio has been shown [10]. Frequency within families: is 2-5%, (10-15% in Middle East) [11]. Rate among twins: is unknown, however a pair of concordant monozygotic twins and 2 discordant pairs were described [12,13]. Behçet’s disease Etiopathogenesis Behçet’s disease: Etiopathogenesis The pathogenesis of BD is still a mystery. There is consensus on the effect of possible environmental factors as infectious agents being responsible for triggering an immunological reaction and systemic features of BD in genetically susceptible individuals [14]. Behçet’s disease: Etiopathogenesis Many factors play a role in the pathogenesis of BD: Genetic Susceptibility is strongly associated with the presence of HLA-B51 allele [1] Infection HSV and Streptococci Bacterial/viral antigens may cross react with human peptides Autoimmunity Endothelial and vascular dysfunction Apoptosis Interesting immunological data promise a way out of the existing dilemma Behçet’s disease: Etiopathogenesis Etiopathogenesis of Behçet’s disease. TNF, tumor necrosis factor; IL, interleukin; CTLA-4, cytotoyic T-lymphocyte antigen-4 [6,7]. Behçet’s disease: Etiopathogenesis Genetic factor: The prevalence of the HLA-B51 allele is high among BD patients (81% of Asians and 13% in Western countries) [15]. Computer illustration of HLA-B*5101 with HIV peptide in the binding pocket. Identification of genes responsible for this susceptibility may lead to more definitive diagnostic tests and new approaches to the management of this potentially blinding condition [14]. Behçet’s disease: Etiopathogenesis Genes as: HLA-B51, MHC-class-I-Chain-related gene A (MICA) and Tumor necrosis factor (TNF) are located on chromosome 6 of MHC and play a crucial role Only HLA-B51 is directly related to the pathogenesis; Other disease related genes have strong linkage disequilibrium with HLA-B51 [10, 16-19]. The search for genes related to BD continues [20]. Behçet’s disease: Etiopathogenesis Role of Cytokines: In BD, the overproduction of proinflammatory cytokines constitutes an important aspect [21]. and are considered markers of disease activity [10, 17, 22,23]. A central pathogenetic role of TNF in the inflammatory process of BD has been suggested and a therapeutic benefit of TNF-α blockers has been reported [24,25]. Behçet’s disease Diagnosis Behçet’s disease: Diagnosis Behçet's disease - can present in a myriad of ways - can involve nearly every organ & system and - has a tendency to recur. Behçet’s disease: Diagnosis Manifestations of BD are extremely diverse: Clinical spectrum ranges from mild mucocutaneous lesions to severe ocular, vascular or neurological disability [24,26,27] Mucocutaneous manifestations constitute the hallmark, while uveitis, meningoencephalitis and large vessel disease are the most serious [28]. Diagnosis is sometimes difficult to confirm as there are no pathognomonic laboratory findings [10] Behçet’s disease: Diagnosis Diagnostic criteria: The most commonly used is the 1990 International Study Group (ISG) Criteria (sensitivity =91% and specificity =96%)[29] A major limitation of these criteria is the inability to diagnose BD in the absence of recurrent oral ulceration [30]. Behçet’s disease: Diagnosis ISG Criteria for diagnosis of Behcet’s disease. Criterion Recurrent Oral ulcers Definition Minor/major aphthous or herpetiform ulceration (observed by physician/patient) which recurs at least 3 times/year Plus two of the following criteria Recurrent Genital ulcers Aphthous ulceration or scarring observed by physician or patient Eye lesions Anterior/posterior uveitis, or cells in vitreous on slit lamp examination; or retinal vasculitis observed by ophthalmologist. Skin lesions Erythema nodosum observed by physician/patient, pseudofolliculitis, papulopustular lesions; or acneform nodules observed by physician in postadolescent patients not on corticosteroid treatment. +ve pathergy test Read by physician at 24-48 hours. Findings are applicable only in absence of other clinical explanations. Presence of recurrent oral ulcers and any 2 of the remaining criteria yields a sensitivity of 91% and specificity of 96% [29] Behçet’s disease: Diagnosis Aphthous ulcer of the labial mucosa [31] Uveitis [ NHS Wales] Behçet’s disease: Diagnosis Papulo-pustules [Quizlet] Erythema nodosum [Medical Point] Behçet’s disease: Diagnosis The frequency of clinical manifestation of BD is: Oral ulcers (100%), followed by genital lesions (80-100%), then ocular lesions (50-79%), and followed by skin lesions (35-60%). Arthritis comes 5th (30-50%), followed by major vessel occlusion/aneurysm (10-37%), then neurological involvement (10-30%) and finally gastrointestinal involvement (0-25%) [32]. Behçet’s disease Disease activity Behçet’s disease: Disease activity The Behçet’s Disease Current Activity Form (BDCAF) scoring appears to be relatively simple to use, reliable and free of bias [33]. Behçet’s disease: Disease activity Behçet’s disease: Disease activity Scoring system for Activity form: Scoring depends on the symptoms present over the preceding 4 weeks prior to assessment. Only clinical features that the clinician feels are due to BD should be scored. (1) To complete the self rating scale of overall wellbeing for the last 4 weeks, please ask the patient the following question: “Here are some faces expressing various feelings, thinking about your Behçet’s disease only, which of these faces describe how you have been feeling over the last 4 weeks?” To complete the self rating scale of wellbeing Today, please ask the patient the following question: “Here are some faces expressing various feelings, thinking about your Behçet’s disease only, which of these faces describe how you feel today?” (2) Scoring for fatigue, headache, oral and genital ulceration, skin lesions, joint symptoms, and gastrointestinal symptoms is based on duration of symptoms (round up to nearest week). Please ask “Over the last 4 weeks, for how many weeks in total have you had………?” 0 1 2 3 4 No symptoms Symptoms for 1 week Symptoms for 2 weeks Symptoms for 3 weeks Symptoms for 4 weeks (1-7 days in total) (8-14 days in total) (15-21 days in total) (22-28 days in total) (3) Eye involvement: Eye activity may be present if the following symptoms are present: Red eye Blurred vision Painful eye Please ask the following question (Tick if symptom is present): “Over the last 4 weeks have you had a red eye_, a painful eye_ or a blurred or reduced vision_?” If any of these symptoms are present or if you feel there may be eye activity refer patient to ophthalmologist who will determine the eye score (Behçet’s Oculopathy Index) Nervous system: Please ask the following question (Tick if symptom is present): “Over the last 4 wks have you had any blackouts_, difficulty of speech or hearing, double vision, weakness or loss of feeling in the face, arm or leg_, memory loss_ or loss of balance_?” If the answer to all these is ‘no’ then answers to Q1-5 are deemed negative; otherwise determine the following: Q1. Are there new symptoms or signs consistent with meningeal involvement? Q2. Are there new symptoms or signs consistent with isolated cranial nerve involvement? Q3. Are there new symptoms or signs consistent with brainstem or cerebellar involvement? Q4. Are there new symptoms or signs consistent with cerebral hemisphere involvement? Q5. Are there new symptoms or signs consistent with spinal cord involvement? Major vessel involvement (exclude neurological involvement): Please ask the following question (Tick if symptom is present): “Over the last 4 weeks have you had chest pain_, breathlessness_,coughed up blood_,or had any pain, swelling or discoloration of either the face_, arm_or leg_?” If the answer to all these is ‘no’ then answers to Q1-4 are deemed negative; otherwise determine the following: Q1. Are there new symptoms or signs consistent with peripheral deep venous thrombosis? Q2. Are there new symptoms or signs consistent with central deep venous thrombosis? Q3. Are there new symptoms or signs consistent with peripheral arterial thrombosis/aneurysm? Q4. Are there new symptoms or signs consistent with pulmonary arterial thrombosis/aneurysm? Behçets disease Management Behçet’s disease: Management Therapeutic approach to BD. . TNF: Tumor Necrosis Factor, IFN: Interferon [6,7] Interleukin-23 Interleukin-23 Over the last decade our knowledge of the role of IL-23 and IL-17 cytokine pathways in immunity and immune-mediated inflammatory diseases, has grown exponentially [34]. Interleukin-23 IL-23 is a member of the IL-12 family of cytokines with proinflammatory properties. Its ability to potently enhance the expansion of T helper 17 (Th17) cells indicates the responsibility for many of the inflammatory autoimmune responses. It is a key participant in central regulation of the cellular mechanisms involved in inflammation. Both IL-23 and IL-17 form a new axis through Th17 cells Interleukin-23 Function of interleukin (IL)-12 and IL-23 on effector cells. IL-12-specific effects are designated red; IL-23-specific effects are designated green; Properties of both in blue. CXCL, chemokine (C-X-C) motif; IFNγ, interferon gamma; GMCSF, granulocyte macrophage colony stimulating factor; NKT, natural killer cells; TNFα, tumor necrosis factor. Interleukin-23 Ustekinumab mechanism of action. Ustekinumab binds to the p40 subunit of interleukin (IL)-12 and IL-23 and prevents their interaction with the cell surface IL-12Rβ1 receptor, subsequently inhibiting IL-12- and IL-23-mediated cell signaling, activation and cytokine production (image not drawn to scale). NK, natural killer. [35]. Interleukin-23 Targeting of IL-23, its receptor or axis is a potential therapeutic approach for autoimmune diseases including psoriasis, inflammatory bowel disease (IBD), rheumatoid arthritis (RA) and multiple sclerosis (MS) [36]. The Clinical Study The Clinical Study Clinical significance of serum interleukin-23 and A/G gene (rs17375018) polymorphism in Behçet’s disease: relation to neuro-Behçet, uveitis and disease activity Tamer A Gheita1, Sherif M Gamal1 , Ihab Shaker2, Hussein S El Fishawy3, Rehab El Sisi4, Olfat G Shaker5, Sanaa A Kenawy 6 1Rheumatology Department, Faculty of Medicine, Cairo University 2Neuropsychiatry Department, Faculty of Medicine, Cairo University 3internal Medicine Department, Faculty of Medicine, Cairo University 4Oral and Maxillofacial Surgeon, Faculty of Oral & Dental Medicine, Cairo University 5Medical Biochemistry and Molecular Biology, Faculty of Medicine, Cairo University 6Clinical Pharmacology Department, Faculty of Pharmacy, Cairo University The Clinical Study Letter to the Editor Joint Bone Spine, 2015; 82:209–17 The Clinical Study Background The Clinical Study: Background A substantial body of knowledge has accumulated supporting a strong genetic underpinning in BD of the MHC-related allele HLA-B51 1. Identification of additional genetic susceptibility loci has clearly caught up 1. IL-23 is involved in the pathogenesis of BD. A strong association of IL-23R single nucleoprotein (rs17375018) was found with BD in a Chinese population 2. Rs (Ref SNP): Reference single-nucleotide polymorphisms The Clinical Study Aim of the work The Clinical Study: Aim of the work The aim of this work was to measure the level of serum IL-23 and assess IL-23R (rs17375018) genotypes in Behçet’s disease (BD) patients and to study the clinical significance and relation to disease activity. Rs (Ref SNP): Reference single-nucleotide polymorphisms The Clinical Study Patients and Methods The Clinical Study: Patients and Methods 50 BD patients 3 (M:F 41:9) were recruited from Cairo University Hospitals. Disease activity was assessed using BDCAF 4. The study conforms to the 1995 Helsinki declaration. All patients gave their informed consent prior to their inclusion. 30 age and sex matched control were also included. --------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------------- Serum IL-23 was quantified by ELISA (Hu IL-23 Heterodimer kit, BioSource immunoassay, Europe S.A. Nivelles, Belgium). IL-23R (rs17375018) was genotyped by Real-time PCR-based allelic discrimination (QIA- Amp DNA-Minikit, Qiagen, Germany). The Clinical Study Results The Clinical Study: Results Table 1: Characteristics, serum IL-23 and IL-23R genotype in BD patients. Feature (mean±SD) Age (years) Disease duration (years) BMI BDCAF Steroid dose (mg/d) Colchicine dose (mg/d) Hemoglobin (g/dl) 3 TLC (x10 /mm3) Platelets (x103/ mm3) ESR (mm/1st hr) Hs-CRP (mg/dl) BD patients (50) 35.2 ±7.2 8.6 ±5.9 26.7 ±4.2 2.6 ±1.5 12.3 ±8.8 0.97 ±0.5 12.9 ±1.1 7.8 ±2.3 292.2 ±76.9 36.1 ±20.7 6.1 ±8.03 Interleukin-23 (pg/ml) 37.1 ± 12.2 IL23R (rs17375018) genotype AA AG GG n (%) 8 (16) 18 (36) 24 (48) BMI: Body mass index , BDCAF: Behcets disease current activity form, TLC: Total leucocytic count, ESR: Erythrocyte sedimentation rate, hs-CRP: Highly sensitive-C-reactive protein Serum IL-23 was significantly higher in patients compared to control (21.9±6.3 pg/ml; p<0.0001) and in females (47.3±13.6 pg/ml) compared to males (34.9±10.8pg/ml; p=0.03). The Clinical Study: Results Table 2: Serum IL-23 level according to the presence and absence of clinical characteristics in Behçet’s disease (BD) patients. Clinical Characteristic n (%) Oral ulcers 50 (100) Genital ulcers 41 (82) Uveitis 24 (48) Skin lesions 37 (74) Neuro-Behçets 19 (38) Pulmonary 11 (22) Arthritis 19 (38) DVT 17 (34) FMS 12 (24) +ve pathergy 14 (28) Serum IL-23 (pg/ml) in BD patients (n=50) Presence Absence p value 36.6±12.03 39.5 ±14.6 0.61 42.6±12.9 32.04 ± 9.1 0.002 38.6±12.4 32.9 ±11.2 0.13 42.6±14.4 33.7 ± 9.4 0.02 38.2±12.8 36.8 ±12.2 0.75 37.6±12.5 36.8 ±12.3 0.84 41.3±10.3 34.9 ±12.7 0.06 43.7±12.9 35.04 ±11.4 0.054 41.5±12.1 35.4 ±12 0.13 DVT: deep venous thrombosis, FMS: fibromyalgia syndrome. Only nine of those with uveitis had concomitant neuro-Behçet. IL23 level significantly correlated with BDCAF (r=0.62,p<0.0001) and disease duration (r=0.42,p=0.002). The Clinical Study: Results IL23R genotypes were comparable between patients and control AA 8/50(16%) vs 6/30(20%), AG 18/50(36%) vs 10/30(33.3%), GG 24/50(48%) vs 14/30(46.7%) (p>0.05) were similar according to gender. in neurobehçets was AA(5.3%), AG(36.8%), GG(57.9%) and those without: AA(22.6%),AG(35.5%),GG(41.9%) in those with uveitis had AA(8.3%), AG(33.3%), GG(58.3%) while those without had AA(23.1%),AG(38.5%), GG(38.5%). BDCAF was significantly lower in AA genotype (1.88±1.13) compared to AG (2.06±1.39) and GG (3.17±1.49) patients (p=0.02) The Clinical Study Conclusions The Clinical Study: Conclusions Serum IL-23 level was significantly increased in BD patients. Serum IL-23 level was significantly higher in BD patients with uveitis. This confirms the findings of others 5. neuro-Behçet's. A crucial role for IL-6/IL-15 in the pathogenesis of neuro-Behçet‘s was found. The precise role of IL-23 remains elusive. IL-23R is upregulated by IL-6 6-8. Serum IL-23 level significantly correlated with BD activity. This is in accordance to the result of Na et al.9. There was a tendency to elevated IL23 in BD patients with FMS. Cytokine involvement in FMS was favored 10. GG-genotype was higher with neuro-Behçet's and uveitis GG-genotype was reported to be of higher prevalence in BD patients 2. The Clinical Study: Conclusions This is the first study to report the possible role played by IL-23 and IL-23R gene polymorphism in neuroBehçet's (and not only uveitis) with a significant relation to disease activity making both potential markers. Larger scale longitudinal studies are required to confirm the role of IL-23 and IL-23R gene polymorphism in neuro-Behҫet and to study their impact on the response to therapy. Cairo University Kasr Al-Ainy School of Medicine Thank You Referenes (Part 1 and 2) [1] Sakane T, Takeno M, Suzuki N, Inaba G. et al. Behçet’s disease. N Engl J Med 1999;341:1284-91 [2] Behcet H. Some observation on clinical picture of the so called triple symptom complex. Dermatologica, 1940, 81:73-83 [3] Adamantiades B. A case of recurrent hypopyon iritis. Athens Greece: Medical Society of Athens. 1930;40:586-93 [4] Kaklamani VG, Variopoulos G, Kaklamanis PG. Behçet's disease. Semin Arthritis Rheum 1998;27:197-217 [5] Dogan S.A., Birdane A. Korkmaz C., Ata N. Timuralp B. Right Ventricular Thrombus with Behçet's Syndrome. Successful Treatment with Warfarin and Immunosuppressive Agents. Tex Heart Inst J. 2007;34(3):360–62. [6] Kastner DL. Intermittent and periodic arthritic syndromes. In: Koopman WJ, ed. Arthritis and allied conditions: a textbook of rheumatology. 13th ed. Vol. 1. Baltimore: Williams & Wilkins, 1997:1279-306 [7] Cho SB, Cho S, Bang D. New Insights in the Clinical Understanding of Behçet's Disease. Yonsei Med J. 2012;53(1):35-42. [8] Gutiérrez E.: Behçet's Syndrome. In: Latinis K.M., Dao K.H., Gutiérrez E., Sheperd R.M., Velazquez C.R. (eds): The Washington Manual Rheumatology Subspeciality Consult, 1st ed. Philadelphia, Lippincott Williams&Wilkins. 2004;31:165-8. [9] Nakae K, Masaki F, Hashimoto T, Inaba G, Mochizuki M, Sakane T. Recent epidemiological features of Behçet's disease in Japan. In: Wechsler B, Godeau P, eds. Behçet's disease. Amsterdam: Excerpta Medica, 1993:145-51 [10] Garton RA, Ghate JV. Jorizzo JL. Behçet's disease. In: Harris E.D., Budd R.C., Genovese M.C., Firestein G.S., Sargent J.S., Sledge C.B. (eds): Kelley's Textbook Of Rheumatology, 7th ed., Philadelphia, Elsevier Saunders; 2005;86:1396-401 [11] Zouboulis CC, Kotter I, Djawari D, et al. Epidemiological features of Adamantiades-Behçet's disease in Germany and in Europe. Yonsei Med J 1997;38:411-22 [12] Hamuryudan V, Yurdakul S, Ozbakir F, Yazici H, Hekim H. Monozygotic twins concordant for Behçet's syndrome. Arthritis Rheum 1991;34:1071-2 [13] Gul A, Inanc M, Ocal L, Aral O, Carin M, Konice M. HLA-B51 negative monozygotic twins discordant for Behçet's disease. Br J Rheumatol 1997;36:922-923 [14] Durrani K, Papaliodis GN. The genetics of Adamantiades-Behçet’s Disease. Semin Ophthalmol. 2008;23(1):73-9. [15] Mizuki N, Inoko H, Ohno S. Pathogenic gene responsible for the predisposition to Behçet's disease. Int Rev Immunol 1997;14:33-48 [16] Taylor PV, Chamberlain MA, Scott JS. Autoreactivity in patients with Behçet's disease. Br.J.Rheumatol. 1993; 32:908-910. [17] Zouboulis CC, May T. Pathogenesis of Adamantiades-Behcet's disease. Adv Exp Med Biol 2003;528: 161-71 [18] Pay S, Abbasov T, Erdem H, Musabak U, Simsek I, Pekel A, et al. Serum MMP-2 and MMP-9 in patients with Behçet's disease: do their higher levels correlate to vasculo-Behçet’s disease associated with aneurysm formation? Clin Exp Rheumatol 2007;25:S70-5. [19] Mizuki N, Inoko H, Ando H, Nakamura S, Kashiwase K, Akaza T et al. Behçet's disease associated with one of the HLA-B51 subantigens, HLA-B*5101. Am. J. Ophthalmol. 1993;116(406-9 [20] Nishiyama M, Takahashi M, Manaka K, et al. Microsatellite polymorphisms of the MICA gene among Japanese patients with Behcet's disease. Can J Ophthalmol ;2006; 41(2):210-5. [21] Yazici H, Yurdakul S, Fresko I. Behçet's Syndrome. In: Isenberg DA, Maddison PA, Woo P, Glass D, Breedveld FC (eds): Oxford Textbook of Rheumatology , 3rd ed., New York, Oxford Univ Press Inc.2004;10 (6): 988-93 [22] Düzgün N, Ayaslioglu E, Tutkak H, Aydintug OT. Cytokine inhibitors: soluble tumor necrosis factor receptor 1 and interleukin-1 receptor antagonist in Behçet's disease. Rheumatol Int; 2005;25(1):1-5. [23] Cekman M, Evereklioglu C, Er H, Inalöz HS, Doganay S, Türköz Y, Ozerol IH. Vascular endothelial growth factor levels are increased and associated with disease activity in patients with Behçet's syndrome. Int J Dermatol 2003;42(11):870-5. [24] Sfikakis PP. Behcet's disease: a new target for anti-tumor necrosis factor treatment. Ann Rheum Dis 2002;61 Suppl 2: ii51-3 [25] Park K, Kim N, Nam J, et al. Association of TNFA promoter region haplotype in Behçet's Disease. J Korean Med Sci 2006;21(4):596-601. [26] Sezen Y, Buyukhatipoglu H, Kucukdurmaz Z, Geyik R. Cardiovascular involvement in Behçet's disease. Clin Rheumatol 2010;29:7-12. [27] Mumcu G., Inanc N., Yavuz S. Direskeneli H. The role of infectious agents in the pathogenesis, clinical manifestations and treatment strategies in Behçet's disease. Clin Exp Rheumatol.2007;25(4 Suppl 45):S27-33. [28] Yurdakul S, Mat C, TuzunY, Ozyazgan Y, Hamuryudan V, Uysal O, Senocak M, Yazici H. "A double-blind trial of colchicine in Behcet's syndrome". Arthritis Rheum 2001;44 (11):2686-92 [29] International Study Group for Behcet's Disease. Criteria for diagnosis of Behçet's disease. Lancet 1990; 335(8697):1078-80. [30] Yousefi, M, Ferringer, T, Lee, S, Bang D, Fivenson D, Butler D et al. Dermatologic Aspects of Behcet Disease. eMedicine from WebMD. Updated: Jul 9, 2012. Available at: http://emedicine.medscape.com/article/1122381-overview [31] Scully C, Felix DH. Oral medicine — Update for the dental practitioner Aphthous and other common ulcers. British Dental Journal 2005;199:259-64 [32] Enzenauer R.J. Behçet's Syndrome. In: West S.G.(ed): Rheumatology Secrets, 2nd ed, Philadelphia, Hanley & Belfus Inc. 2002;36:244-8. [33] Bhakta BB., Brennan P. James TE., Chamberlain M.., Noble BA. Silman, A.J. Behçet's disease: evaluation of a new instrument to measure clinical activity. Rheumatology 1999;38:728-33 [34] Smith JA, Colbert RA. Review: The interleukin-23/interleukin-17 axis in spondyloarthritis pathogenesis: Th17 and beyond. Arthritis Rheumatol. 2014;66(2):231-41. [35] Benson JM, Peritt D, Scallon BJ, Heavner GA, Shealy DJ, Giles-Komar JM et al. Discovery and mechanism of ustekinumab: a human monoclonal antibody targeting interleukin-12 and interleukin-23 for treatment of immune-mediated disorders. MAbs. 2011;3(6):535-45. [36] Tang C, Chen S, Qian H, Huang W. Interleukin-23: as a drug target for autoimmune inflammatory diseases. Immunology. 2012;135(2):112-24. References (Part 3) 1. Maldini C, Lavalley MP, Cheminant M, de Menthon M, Mahr A. Relationships of HLA-B51 or B5 genotype with Behcet's disease clinical characteristics: systematic review and meta-analyses of observational studies. Rheumatology (Oxford). 2012;51(5):887-900. 2. Jiang Z, Yang P, Hou S, Du L, Xie L, Zhou H, Kijlstra A. IL-23R gene confers susceptibility to Behcet's disease in a Chinese Han population. Ann Rheum Dis. 2010;69(7):1325-8. 3. International Study Group for Behcet’s Disease. Criteria for diagnosis of Behçet’s disaese. Lancet. 1990;335:1078–80 4. Bhakta BB, Brennan P, James TE,Chamberlain MA, Noble BA, Silman AJ. Behçet's disease: evaluation of a new instrument to measure clinical activity. Rheumatology (Oxford). 1990;38(8):728-33. 5. Sugita S, Kawazoe Y, Imai A, Yamada Y, Horie S, Mochizuki M. Inhibition of Th17 differentiation by anti-TNF-alpha therapy in uveitis patients with Behçet's disease. Arthritis Res Ther. 2012;14(3):R99. 6. Borhani Haghighi A, Ittehadi H, Nikseresht AR, Rahmati J, Poorjahromi SG, Pourabbas B, et al. CSF levels of cytokines in neuro-Behçet's disease. Clin Neurol Neurosurg.2009;111(6):507-10 7. Hamzaoui K, Hamzaoui A, Ghorbel I, Khanfir M, Houman H. Levels of IL-15 in serum and cerebrospinal fluid of patients with Behçet's disease. Scand J Immunol. 2006;64(6):655-60. 8. McGeachy MJ, Chen Y, Tato CM, Laurence A, Joyce-Shaikh B, Blumenschein WM, et al. The interleukin 23 receptor is essential for the terminal differentiation of interleukin 17-producing effector T helper cells in vivo. Nat Immunol. 2009;10(3):314-24. 9. Na SY, Park MJ, Park S, Lee ES. Up-regulation of Th17 and related cytokines in Behçet's disease corresponding to disease activity. Clin Exp Rheumatol. 2013;31(3 Suppl 77):32-40. 10. Pernambuco AP, Schetino LP, Alvim CC, Murad CM, Viana RS, Carvalho LS, et al. Increased levels of IL-17A in patients with fibromyalgia. Clin Exp Rheumatol. 2013;31(6 Suppl 79):S60-3.