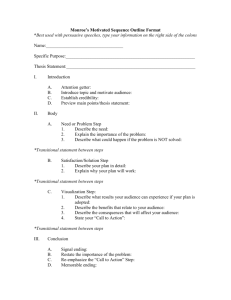
Numbering Technique/Approach to Report LSTV
advertisement
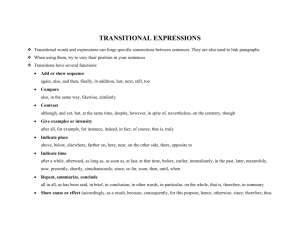
PRESENTATION NUMBER eEdE-212 Disclosure • No potential conflicts of interest to disclose. Lumbosacral Transitional Vertebrae Classifications & Clinical Significance Eman Mahdi, MD Anousheh Sayah, MD MedStar Georgetown University Hospital; Washington DC ASNR 2015 – Chicago, IL Index 1. 2. 3. 4. 5. Objectives Introduction Definition Classifications Examples and Cases 6. Numbering techniques 7. Clinical significance 8. Conclusion 9. References Objectives • Review the anatomical landmarks and criteria used to label Lumbosacral Transitional Vertebra (LSTV) • Review cases to demonstrate this variant anatomy and the various classifications using different modalities • Discuss the approach to reporting LSTV • Demonstrate the clinical significance of transitional vertebra Introduction • Variability in spine numbering in the lumbosacral region is a common challenge in reporting of spine imaging cases. • Most worrisome is the possibility of wrong-level spine surgery based upon imaging reports. • LSTV have been purported as a cause of low back pain, notably in the young. Definition of LSTV • LSTVs are congenital spinal anomalies defined as either sacralization of the lowest lumbar segment or lumbarization of the most superior sacral segment. • Prevalence is 4%–30% in general population. • Higher rate in men than in women. Classification & Identification • Castellvi classification • O’Driscoll classification • Identifying Landmarks: Iliolumbar ligament Difference in vertical mid-vertebral angles (DiffVMVA) Lower Lumbar/Upper Sacral segment shape Vascular structures Lumbosacral Intervertebral Disc Angle (LSIVDA) Castellvi classification Based on transverse process morphology Type I: Unilateral (Ia) or bilateral (Ib) enlarged dysplastic transverse processes with a height more than 19 mm. Type II: Unilateral (IIa) or bilateral (IIb) Pseudoarthrosis of the transverse process and the sacrum. Type III: Unilateral (IIIa) or bilateral (IIIb) complete osseous fusion of the transverse process(es) to the sacrum. Type IV: Pseudoarthrosis (type II) on one side and complete fusion on the other side(type III). *(1) Examples of Castellvi Classification B A Castellvi type I (Enlarged bilateral transverse processes) Castellvi Type IIa (Unilateral pseudoarthrosis on the right) A: AP X-ray, B: Axial T2 MRI Examples of Castellvi Classification Castellvi type IIIb (bilateral osseous fusion of the transverse process to the sacrum) Classification & Identification • Castellvi classification • O’Driscoll classification • Identifying Landmarks: Iliolumbar ligament Difference in vertical mid-vertebral angles (DiffVMVA) Lower Lumbar/Upper Sacral segment shape Vascular structures Lumbosacral Intervertebral Disc Angle (LSIVDA) O’Driscoll Classification Based on first sacral disk morphology & AP length by sagittal MR Type I: Type II: Type III: Type IV: No disk material Small residual disk Well-formed disk extending the entire AP length of the sacrum Similar to type 3 with addition of squaring of the presumed upper sacral segment Example of O’Driscoll Classification L1 L1 L2 L2 L3 L3 L4 L4 L5 # L5 S1 # S1 * * Type IV O’Driscoll. Well formed disc* with squaring# of S1 Identifying Landmarks in Assessing LSTV 1. Iliolumbar ligament denoting the lowest lumbar type vertebral segment and the lumbosacral junction (does not always represent L5 level). It is a low-signal-intensity structure on both axial T1 and T2 weighted MR images, extending from the transverse process of ‘L5’ to the posteromedial iliac crest.(3) Anterior band L5 Posterior band Classification & Identification • Castellvi classification • O’Driscoll classification • Identifying Landmarks: Iliolumbar ligament Difference in vertical mid-vertebral angles (DiffVMVA) Lower Lumbar/Upper Sacral segment shape Vascular structures Lumbosacral Intervertebral Disc Angle (LSIVDA) Identifying Landmarks in Assessing LSTV 2. Difference in vertical mid-vertebral angles (DiffVMVA) of the most 2 caudal vertebral segments, in single midsagittal MRI or lumbosacral x-ray. Difference of ≤+10° has 100% sensitivity and 89% specificity in solid bony bridge (i.e. Castellvi type 3 & 4). (4) L4 L4 Diff-VMVA = VMVA of Lowest segment – VMVA One above lowest segment A: LSTV ≤+10 (24-27= -3) B: Normal >+10 (48-6= +42) A B Identifying Landmarks in Assessing LSTV 3. Squaring (* Fig A) of the upper sacral segment when it is lumbarized and Wedging (↑ Fig B) of the lowest lumbar segment when it is sacralized.(8) L5 S1 * S2 A 4. Vascular landmarks such as aortic bifurcation at L4, right renal artery origin at L1/L2 disc, and IVC confluence at L5. These are not reliable due to variability in anatomy and due to the fact that they are not always imaged. L4 L5 S1 B Identifying Landmarks in Assessing LSTV 5. Lumbosacral Intervertebral Disc Angle (LSIVDA): the angle between lines drawn along the inferior endplate of the lowest lumbar vertebra and the superior endplate of the first sacral vertebra. Note -- Recent studies have found no significant correlation between LSIVDA and LSTV.(3) Numbering Technique/Approach to Report LSTV The approach used in vertebral numbering should be mentioned in the report and/or discussed with the referring physician. Discuss number of non-rib bearing lumbar type vertebra. Describe presence of any LSTV: • Lumbarized S1 • Sacralized L5 Formally label the last lumbar type vertebra, whether it be L4, L5, L6, or S1, depending on the method chosen. Numbering Technique/Approach to Report LSTV Additional imaging options: • Sagittal whole spine MR localizer may be used to better evaluate LSTV.(5) • Coronal MR cervicothoracic localizer increases the accuracy of identifying LSTV. Numbering Technique/Approach to Report LSTV • Coronal T1WI MRI of the lumbosacral junction and sacrum can also identify LSTV which can sometimes be the cause for S1 radicular symptoms – in this case, the cause was not identified on the sagittal and axial MRI sequences.(6) Castellvi IIb LSTV with bilateral pseudoarthroses (black arrows) and osteophytic compression of S1 nerve roots (white arrows) Clinical significance • Relationship of low back pain and LSTV, termed “Bertolotti Syndrome” • Wrong-Level Spine Surgery Clinical significance • Symptoms can originate from: The anomalous articulation itself The contralateral facet joint (when unilateral) Instability and early degeneration of the level cephalad to the transitional vertebrae Nerve root compression from hypertrophy of the transverse process. Types II and IV had higher prevalence and severity of low back pain and buttock pain.(7) 67 year old patient with right sided radiculopathy L5 S1 Sagittal and axial T2 MRI shows large right L5 transverse process with pseudoarthrosis impinging on the right exiting L5 nerve root. Arrow denotes the normal left L5 exiting nerve root. Conclusion • Prevalence of LSTV is 4%–30% in the general population. • Assessment of LSTV is essential in reporting spine MRI. • Describing the method of vertebral numbering in the report is crucial in helping to avoid wrong level spine surgery. References • 1. Konin GP, Walz DM. Lumbosacral transitional vertebrae: classification, imaging findings, and clinical relevance. AJNR Am J Neuroradiol. 2010 Nov;31(10):1778-86. • 2. Hughes RJ, Saifuddin A. Numbering of lumbosacral transitional vertebrae on MRI: role of the iliolumbar ligaments. AJR Am J Roentgenol. 2006 Jul;187(1):W59-65. • 3. Carrino JA, Campbell PD Jr, Lin DC, et al. Effect of Spinal Segment Variants on Numbering Vertebral level at Lumbar MR imaging. Radiology. 2011 Apr;259(1):196-202. • 4. Farshad M, Aichmair A, Hughes AP, et al. A reliable measurement for identifying a lumbosacral transitional vertebra with a solid bony bridge on a single-slice midsagittal MRI or plain lateral radiograph. Bone Joint J. 2013 Nov;95-B(11):1533-7. • 5. Hanson EH, Mishra RK, Chang DS, et al. Sagittal whole-spine magnetic resonance imaging in 750 consecutive outpatients: accurate determination of the number of lumbar vertebral bodies. J Neurosurg Spine. 2010 Jan;12(1):47-55. • 6. Bezuidenhout AF, Lotz JW. Lumbosacral transitional vertebra and S1 radiculopathy: the value of coronal MR imaging. Neuroradiology. 2014 Jun;56(6):453-7. • 7. Nardo L, Alizai H, Virayavanich W, et al. Lumbosacral transitional vertebrae: association with low back pain. Radiology. 2012 Nov;265(2):497-503. • 8. Tokgoz N, Ucar M, Erdogan AB, et al. Are spinal or paraspinal anatomic markers helpful for vertebral numbering and diagnosing lumbosacral transitional vertebrae? Korean J Radiol. 2014 Mar-Apr; 15(2):258-66.